- 1Department of Psychiatry, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia
- 2Department of Public Health, Kutaber Health Center, Kutaber, Ethiopia
- 3School of Veterinary Medicine, Woldia University, Woldia, Ethiopia
Introduction: Substance use during the perinatal period is a significant public health concern, as it can have potential adverse effects on maternal and neonatal health outcomes. Unexpectedly, no previous studies have been conducted to assess the prevalence of substance use during the perinatal period among Ethiopian women. Therefore, this study aimed to determine the magnitude of substance use and its determinant factors during the perinatal period.
Method: We conducted a hospital-based descriptive cross-sectional study among a systematically selected sample of 418 women who attended perinatal care between May and July 2022. Data were collected using an interviewer-administered structured questionnaire. Multivariate logistic regression analysis, with a 95% confidence interval and p-values less than 0.05, was employed to identify factors associated with substance use behavior.
Result: The prevalence of perinatal substance use was found to be 38.3% (95% CI: 33.5–43.5). Of the women who used substances, 109 (26.1%) reported using chat, 46 (11.0%) reported alcohol consumption, and 5 (1.20%) reported using shisha. Factors significantly associated with substance use behavior during the perinatal period included a history of obstetric complications (AOR = 1.722, 95% CI: 1.022–2.902), the presence of chronic medical conditions (AOR = 3.784, 95% CI: 2.164–6.615), experiencing physical abuse (AOR = 5.323, 95% CI: 2.171–13.050), depression (AOR = 1.963, 95% CI: 1.028–3.749), and experiencing sleep disturbances (AOR = 2.016, 95% CI: 0.975–4.168). Conversely, giving birth to a live baby was found to be a protective factor against substance use behavior (AOR = 0.389, 95% CI: 0.187–0.810).
Discussion: This study highlights a high prevalence of substance abuse among women during the perinatal period. In light of these findings, a comprehensive approach is recommended to address perinatal substance use among Ethiopian women. This should include the integration of preventive educational programs into perinatal care.
Introduction
Substance use during the perinatal period poses a significant public health concern due to the potential for adverse maternal and neonatal health outcomes [1]. Globally, more than 190 million people use substances, with alcohol and khat being the most commonly used [2]. Substance use can have detrimental physical, psychological, and social consequences for women, their children, and their families [1, 3, 4]. However, the nature and severity of these effects depend on factors such as dosage, frequency, route of administration, and type of substance [2, 5]. Due to various reasons, women of childbearing age may be more vulnerable to substance use and related disorders [6].
Studies in Europe have reported varying prevalence rates of substance use among women during the perinatal period, ranging from 2% to 27% [5]. The adverse health consequences of substance use affect not only the mother but also the developing fetus and the newborn child [7–13]. Maternal substance use poses a significant risk to child care and disrupts the stability of family life [4, 14]. Common substances used during the perinatal period include alcohol, tobacco, cannabis, and opioids [6].
Substance use during the perinatal period has wide-ranging biological, psychological, social, and economic impacts [10–12]. Maternal substance use, particularly alcohol, is associated with a substantial risk of fetal alcohol spectrum disorders and fetal alcohol syndrome [10]. The World Health Organization (WHO) has identified perinatal substance use, especially alcohol, as a determinant of intellectual and developmental disability [15, 16].
Substance use during the perinatal period is linked to adverse outcomes such as miscarriage, intrauterine growth restriction, early labor, and intrauterine fetal demise [16]. It is strongly associated with reduced birth weight [13, 17], inadequate parenting [14], stillbirth, spontaneous abortion, premature birth, and intrauterine growth retardation [1, 10, 17, 18]. Cigarette smoking and prenatal alcohol exposure are the leading preventable causes of pregnancy-related morbidity, mortality, and developmental problems [16, 19].
Maternal substance use during pregnancy and the postnatal period commonly leads to neurocognitive deficits in children, affecting language, motor, and cognitive functions [17, 20]. Additionally, it can impact other organ systems, such as the heart, skeleton, kidneys, eyes, and auditory system [11, 17, 18]. Substance use is also consistently associated with other mental health conditions, particularly anxiety and depression [21].
A study in the United States reported that the prevalence of substance use in the prenatal period was 25.8% and that unemployment, unmarried status, and psychopathology played a role in it [21]. A study in the United Kingdom also reported that alcohol consumption varied widely (from 10% to 54%) [22]. A study conducted at a university in Ethiopia shows that 46.2% of the study population had used at least one substance in their lifetime and that gender, religion, and income were significantly associated factors [2]. Another study conducted in Jimma town among pregnant women reported that 37.9% were current substance users and that educational status, family history of substance use, occupational status, and gestational age were all found to be associated with substance use [3]. To our knowledge, there are no published Ethiopian data on substance use among women in the perinatal period. Therefore, the aim of this study is to assess the extent of substance use and associated factors among women attending perinatal services at the Kutaber district government health facilities and at the Boru Meda General Hospital in the Amhara region of Ethiopia.
Methods and materials
A cross-sectional study was conducted in Kutaber District and at the Boru Meda General Hospital, Amhara, Ethiopia, from March to June 2022. The study included women who received perinatal services during this period. Eligible participants were women aged 18 years or older, with regular antenatal and postnatal care attendance, and those willing to participate. Women with hearing or speech impairments and those who were severely ill and unable to complete the questionnaires were excluded. The desired sample size of 418 was calculated using a double population proportion formula with a 95% confidence level, 80% study power, a 2:1 ratio of exposed to unexposed groups, an outcome rate of 37.8% in the unexposed group, and an adjusted odds ratio of 1.71 from a previous study [23].
We recruited the study participants using a systematic random sampling method. The total estimated number of women who visited the study area per day is 65 (30 and 35 in the Kutaber district health facility and at the Boru Meda General Hospital, respectively). In 1 month, a total of 1,430 women (663 in Kutaber and 767 at the Boru Meda General Hospital) were visited. Since the number of required study participants is 418, the sampling interval (k) was calculated as 1430/418 = 3. Accordingly, we selected one participant for every three women. A proportional allocation was made to the study area. These 194 and 224 women were recruited from the Kutaber district health facility and the Boru Meda General Hospital, respectively. Finally, the first starting number of each study site was picked randomly using the lottery method from the registration counter. We used a structured interviewer-administered questionnaire to obtain socio-demographic, obstetric, behavioral, and other relevant associated information from the respondents.
The data collection tool was a structured questionnaire consisting of socio-demographic, obstetric substance use-related characteristics (substance use before and during the perinatal period), and personal and social factors. The questionnaire was first prepared in English and then translated into Amharic languages and back into English to facilitate understanding and ensure consistency during administration. To screen for perinatal substance use, a modified form of ASSIST was used, which was developed by an international group of substance abuse researchers at WHO to detect and manage substance use and related problems in primary and general medical care settings. It consists of a series of questions asking individuals about the frequency and quantity of substance use in the past 3 months. The average reliability test coefficients for ASSIST ranged from Cronbach’s α of 0.58–0.90, indicating good to excellent reliability [24, 25]. Perinatal depression, anxiety, and stress were assessed by using the Depression Anxiety and Stress Scale-21 (DASS-21), which contains relevant items (seven statements each for depression, anxiety, and stress subscales) to recognize the presence and severity of symptoms of these three psychological conditions. The internal consistency and reliability of the DASS-21 were very impressive in Ethiopia, with Cronbach’s α of 0.75, 0.72, 0.86, and 0.95 for the DASS depression, anxiety, stress, and total scales, respectively [26]. These coefficients demonstrated good internal consistency, with cut-off values for DASS depression, anxiety, and stress of 9, 7, and 14, respectively [26–30].
The Epworth Sleepiness Scale was used to measure a subjective report of daytime sleepiness in women. The ESS has excellent psychometric validity for screening daytime sleepiness in the Ethiopian population [31, 32] with a reliability test of 0.725 [32]. Women with an ESS score >10 were included in the sleepy group, and those with a score ≤10 were included in the non-sleepy group [33–37].
Socio-demographic characteristics and obstetric variables such as pregnancy trimester, previous pregnancy and labor complications, previous history of stillbirth, previous history of abortion, plan of current pregnancy, previous psychiatric history, baby’s father’s support, partner’s feelings on current pregnancy, and community support were all collected by a structured and pre-tested questionnaire.
Data were collected by four BSc graduate female clinical nurses and under the supervision of two MSc public health professionals. The completeness and consistency of the collected data were checked daily by the supervisors and the principal investigator. Ethical approval for the study was granted by the Institutional Review Board (IRB) of Wollo University College of Medicine and Health Science, Ethiopia. A letter of permission was obtained from the Kutaber District Health Office and Boru Meda Hospital. Before starting to fill out the questionnaire, written consent was collected from every participant.
Data quality control
To ensure data quality, 2 days of training (1 day theoretical and 1 day practical) were given to data collectors and supervisors. A pretest was conducted on 10% of the total sample size attending the perinatal service at Haroye Health Center to assess the simplicity, flow, and consistency of the questionnaire. Data entry was performed using Epi-Info™ version 7.1. After a full inspection for completeness and consistency, these were then exported to the Statistical Package for the Social Sciences, SPSS v. 26 (IBM, Armonk, USA) for analysis. Categorical descriptive results were expressed as an actual number (frequency). To determine the association between independent and dependent variables, binary logistic regression was performed. Variables in bivariable analysis with a p < 0.2 were selected for multivariable logistic regression. In the multivariable analysis, variables with a p < 0.05 and a 95% CI were considered significant factors for perinatal substance use. Hosmer and Lemshow goodness-of-fit tests were performed to assess model fitness at p > 0.05. In addition to p values, crude odds ratio and adjusted odds ratios with a 95% CI were reported.
Ethical clearance was obtained from the Institutional Review Board (IRB) of Wollo University College of Medicine and Health Science. A permission letter was obtained from the Kutaber District Health office and Boru Meda Hospital and written consent was taken from each study participant. Personal identifying details were not recorded.
Results and discussion
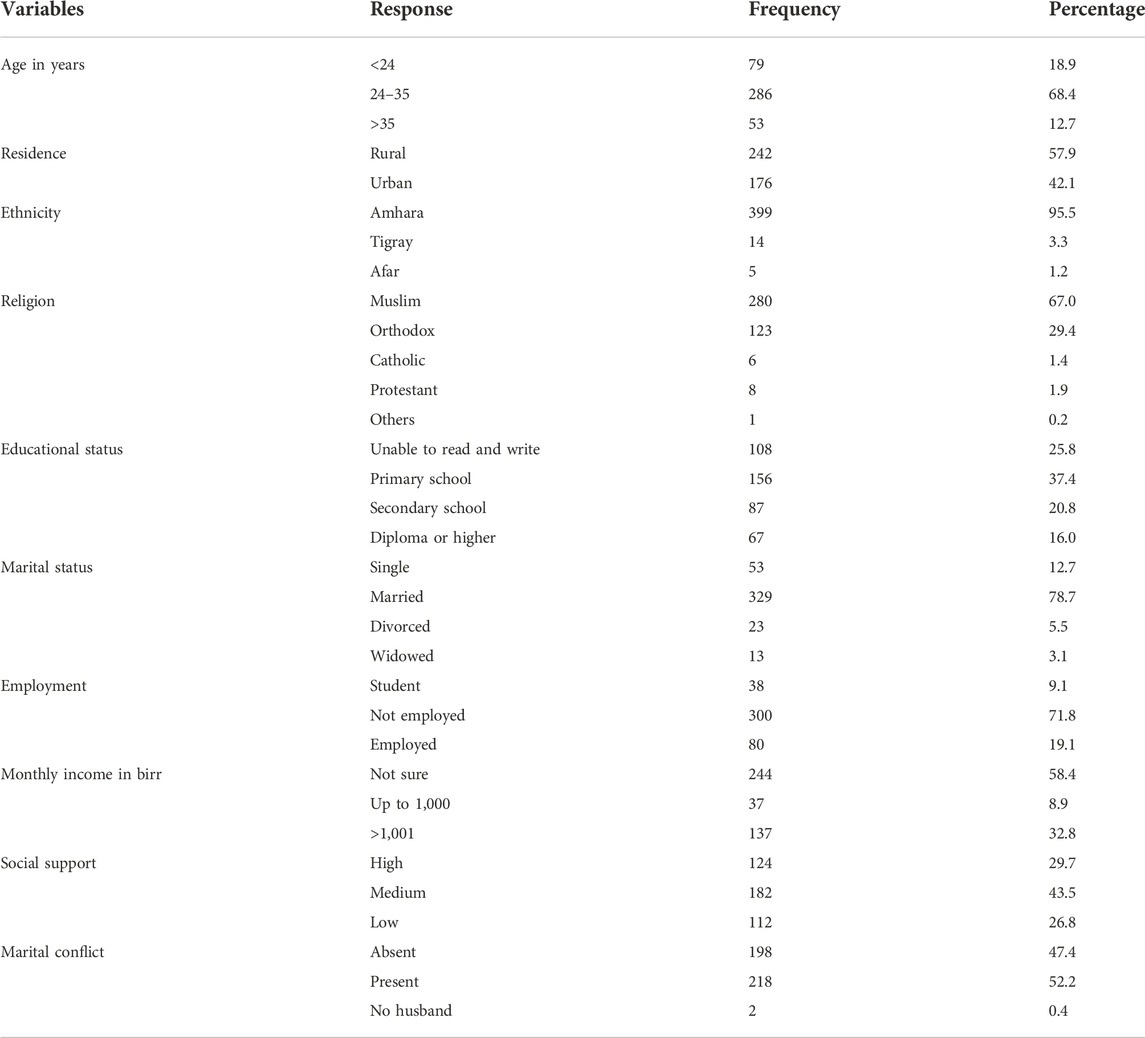
In this study, 418 women were recruited, resulting in a 100% response rate. All respondents were between 18 and 45 years of age, with a mean age of 29.9 ± 5.44 (SD). The median age was 29.5 years, and the mode was 30 years. Among the participants, 286 (68.4%) were aged 24–30 years, 242 (57.9%) lived in rural areas, 399 (95%) identified as Amhara by ethnicity, 329 (78.7%) were married, and 280 (67%) identified as Muslim by religion (Table 1).
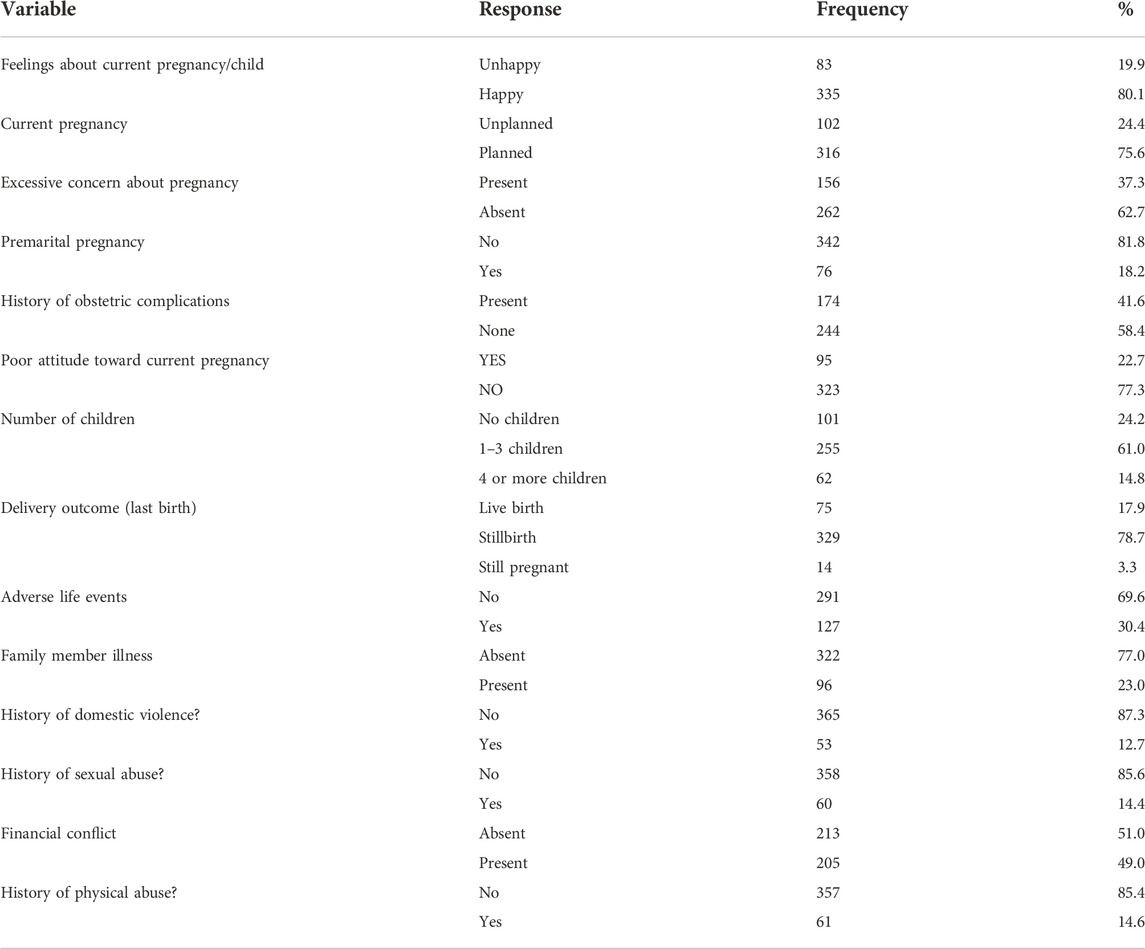
Concerning their feelings about the current pregnancy/child, 355 women (80.1%) reported feeling happy, 316 (75.6%) stated that the pregnancy/child was planned, 262 (62.7%) did not have excessive pregnancy-related concerns, and 342 (81.8%) indicated that the pregnancy/child was post-marital (Table 2).
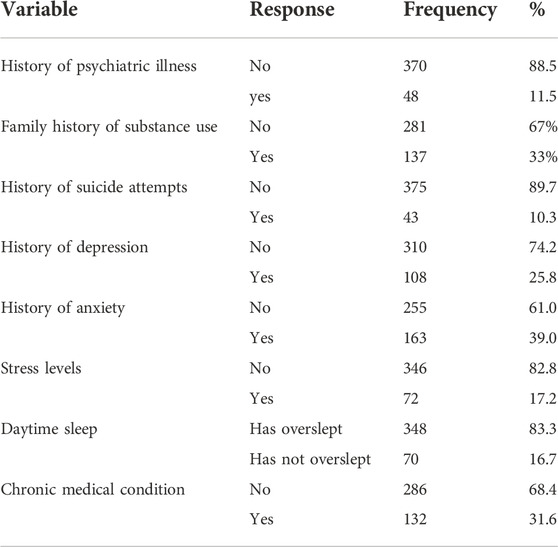
Clinically, among the women recruited, 48 (11.5%) had a history of previous psychiatric problems, 43 (10.3%) had attempted suicide, and 108 (25.8%), 163 (39.0%), 72 (17.2%), and 70 (16.7%) experienced symptoms of depression, anxiety, stress, and sleepiness, respectively. Additionally, 132 women (31.6%) had other medical conditions (Table 3).
Of the 418 women in the sample, 160 (38.3%) reported using substances. Among substance users, 109 (26.1%) used khat, 46 (11.0%) consumed alcohol, and 5 (1.20%) used shisha. Of these substance users, 63 (46.0%) had a family history of substance use. In terms of frequency, 20 (4.8%) used substances daily, 75 (17.9%) weekly, 39 (9.3%) monthly, 9 (2.2%) irregularly, and 17 (4.1%) only once or twice in their lifetime.
Factors associated with substance use
To identify factors associated with substance use, bivariate analyses were conducted between substance use and various sociodemographic, obstetric, psychosocial, and clinical variables. Factors with p values less than 0.20 in bivariate analyses were included in a multivariate logistic regression for further analysis.
Substance use was significantly associated with having a history of obstetric complications (AOR = 1.722, 95% CI: 1.022–2.902), the presence of chronic medical conditions (AOR = 3.784, 95% CI: 2.164, 6.615), physical abuse (AOR = 5.323, 95% CI: 2.171, 13.050), depression (AOR = 1.963, 95% CI: 1.028, 3.749), and sleepiness (AOR = 2.016, 95% CI: 0.975, 4.168). On the other hand, having a live birth was a protective factor against perinatal substance use (AOR = 0.389, 95% CI: 0.187, 0.810) (Table 4).
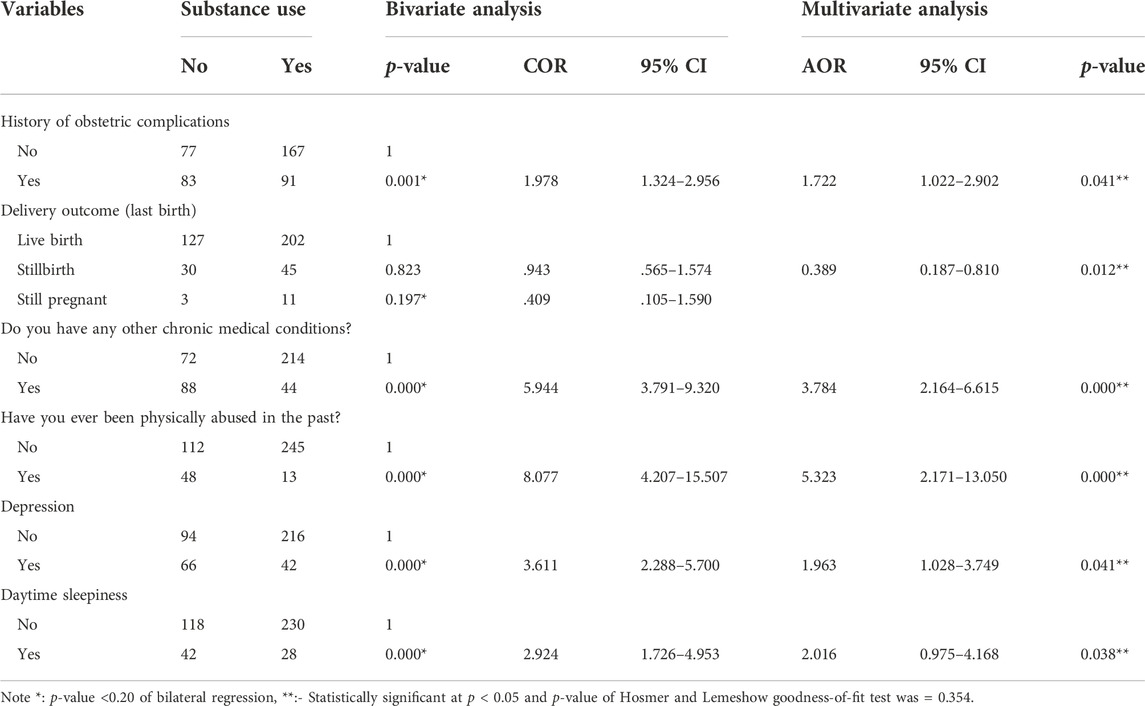
TABLE 4. Factors associated with substance use (bivariate and multivariate logistic regression analysis) (N = 418).
The study found that the overall prevalence of substance use among women in the perinatal period was 38.3% (95% CI: 33.5–43.45). This prevalence is similar to a systematic meta-analysis study among pregnant women in the Amhara region, which reported a prevalence of 36.7% [38]. The prevalence of substance use in this study was higher than in other studies conducted in the USA among pregnant women at 25.8% [21], in Iran among pregnant women at 15% [39], and in Ethiopia among college students at 26.6% [40]. In contrast, the prevalence in this study is lower than in another study in Ethiopia among university students (55.2%) [2].
The variation could be due to the differences in study participants, geographical location, demographic characteristics, methodological differences, sample size, economic factors, lifestyle, substance availability, early diagnosis and treatment, availability of counseling services, and criteria used to define substance use.
In terms of associated factors, the study found that women with a history of obstetric complications were more likely to engage in risky substance use during the perinatal period (AOR = 1.722, 95%: 1.022–2.902). This is consistent with other studies conducted in Germany [13], in the United States [41], in South Africa [42], and in Ethiopia [10]. This suggests that stress and anxiety related to previous complications may lead some women to turn to substances as a coping mechanism.
Similar to other studies in the United States of America (43, 44), women with chronic medical illnesses were three times more likely to engage in substance use during the perinatal period (AOR = 3.784, 95% CI: 2.164, 6.615). This may be due to the added stress and physical discomfort associated with managing a chronic illness in combination with pregnancy.
The study also shows that women with a history of physical abuse were five times more likely to use perinatal substances (AOR = 5.323, 95%: 2.171, 13.050). This was supported by the study conducted in the USA [45]. The association may be due to the fact that women who experience physical abuse may resort to substance use as a way of coping with the trauma or stress associated with the abuse.
Compared with women without current depression symptoms, women with current depression symptoms were twice as likely to use substances in the perinatal period (AOR = 1.963, 95% CI: 1.028, 3.749). The result was consistent with other studies in the United States [21] and in Ethiopia [10]. The association may be due to the fact that women with poor mental health are more likely to use a substance for self-treatment. So, this highlights the importance of addressing mental health issues during the perinatal period to reduce the risk of substance use.
In agreement with another study conducted in New York [46], there was a trend indicating an association between sleepiness and perinatal substance use. This suggests that sleep disturbance or hypersomnia may be linked to substance abuse as women seek ways to manage their sleep-related problems.
Interestingly, the study found that having a live birth was a protective factor against substance use during the perinatal period. This finding is also in line with other studies of pregnant women in different parts of the world [4, 15, 18, 39]. This may suggest that women who successfully give birth to a healthy child are less inclined to use substances during the perinatal period. Further research is needed to fully understand this protective effect.
Conclusion
In the current study, a significant proportion of mothers were shown to use substances in the perinatal period in a risky way (for the mother, the growing fetus, and the born child). Having a history of obstetric complications, along with the presence of chronic medical illness, physical abuse, depression, and sleepiness, were found to be significantly associated with substance use behavior in the perinatal period. Conversely, having a live birth was a protective factor for substance use behavior in the perinatal period. In light of these findings, a comprehensive approach is recommended to address perinatal substance use among Ethiopian women. This should include the integration of preventive educational programs into perinatal care. Healthcare providers should be trained to screen women for substance use and associated risk factors, such as a history of obstetric complications, chronic illness, physical abuse, and depression, and to provide appropriate counseling and connect women to support services for substance use and mental health issues. A multidisciplinary approach, involving healthcare professionals, social workers, and counselors, is essential to effectively tackle this public health challenge and improve the wellbeing of both mothers and newborns during the perinatal period.
Recommendation
Implement routine screening for substance use and associated risk factors as part of perinatal care to identify at-risk women. Promote integrated care that addresses both physical and mental health needs during the perinatal period, especially for women with chronic medical conditions, physical abuse, psychopathology, and a history of obstetric complications. Develop support programs and interventions aimed at reducing substance use during the perinatal period, with a focus on addressing the identified risk factors. Provide health education about the effects of substance use on the mother, fetus, and child for all women in antenatal and postnatal care follow-up units.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
This study was carried out after obtaining ethical approval from the institutional review board (IRB) of Wollo University, College of Medicine and health sciences. All procedures performed were by the ethical standards of the institutional and national research committee at which the studies were conducted and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)’ legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
JS conceived the study and was involved in its conception, study design, review of the article, performing analysis, data interpretation, report writing, and drafting of the manuscript. EM and YM were involved in data interpretation, report writing, and review of the manuscript. All authors read and approved the final version of the manuscript.
Funding
The Kutaber District administrative office has contributed some funds for data collection procedures. They did not contribute to the publication of this work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We are thankful to Wollo University, College of Medicine and Health Sciences, for funding this research project. We also extend our acknowledgment to Kutaber District Health Office and Boru Meda General Hospital authorities, data collectors, supervisors, and respondents who participated in this study.
Abbreviations
ANC, Antenatal Care; AOR, Adjusted odds ratio; ASSIST, Alcohol, Smoking, and Substance Involvement Screening Test; CI, Confidence Interval; COR, Crude odds ratio; DASS-21, Depression, Anxiety and Stress Scale-21; PNC, Postnatal Care; SPSS, Statistical Package for Social Science; USA, United States of America; WHO, World Health Organization.
References
1. Meinhofer, A, Witman, A, Catherine, J, and Yuhua, M. Prenatal substance use policies and newborn health. Health Econ (2022) 31:1452–67. doi:10.1002/hec.4518
2. Adem, A, Endebu, T, Tsegaye, D, and Bogale, T. Assessment of substance use and associated factors among graduating class students of adama science and technology addiction & drug abuse open access journal. Addict Drug Abus J (2019) 2(1).
3. Fy, T, La, W, and Db, K. Magnitude of substance use and associated factors among pregnant women attending Jimma town public health facilities, Jimma zone, oromia regional state southwest Ethiopia clinics in mother and child health. Clin Mother Child Heal (2017) 14(4). doi:10.4172/2090-7214.1000275
4. Howell, EM, and Chasnoff, IJ Perinatal substance abuse treatment findings from focus groups with clients and providers. J Subst Abuse Treat (1999) 17(98):139–48. doi:10.1016/s0740-5472(98)00069-5
5. Conner, SN, Bedell, V, Lipsey, K, Cahill, AG, and Tuuli, MG. Maternal marijuana use and adverse neonatal outcomes A systematic review and meta-analysis. Obs Gynecol (2016) 128(4):713–23. doi:10.1097/AOG.0000000000001649
6. Chang, G. Maternal substance use: consequences, identification, and interventions. Alcohol Res Curr Rev (2020) 40(2):06–10. doi:10.35946/arcr.v40.2.06
7. Can, M, Radcli, P, Marlow, S, Boreham, M, and Gilchrist, G. Maternal substance use and child protection: a rapid evidence assessment of factors associated with loss of child care. Child Abuse Neglect (2017) 70:11–27. doi:10.1016/j.chiabu.2017.05.005
8. Namy, S, Carlson, C, Pala, AN, Faris, D, Knight, L, Allen, E, et al. Gender, violence and resilience among Ugandan adolescents. Child Abuse Negl (2017) 70:303–14. doi:10.1016/j.chiabu.2017.06.015
9. Petrowski, N, Cappa, C, and Gross, P. Estimating the number of children in formal alternative care: challenges and results. Child Abuse Negl (2017) 70:388–98. doi:10.1016/j.chiabu.2016.11.026
10. Wubetu, AD, Habte, S, and Dagne, K. Prevalence of risky alcohol use behavior and associated factors in pregnant antenatal care attendees in Debre Berhan, Ethiopia, 2018. BMC Psychiatry (2019) 19(250). doi:10.1186/s12888-019-2225-1
11. Vythilingum, B, Roos, A, Faure, SC, Geerts, L, and Stein, DJ. Risk factors for substance use in pregnant women in South Africa. South Africa Med J (2012) 102(11):851–4. doi:10.7196/samj.5019
12. Stone, R. Pregnant women and substance use: fear, stigma, and barriers to care. Stone Heal Justice (2015) 3(1):2. doi:10.1186/s40352-015-0015-5
13. Hacker, M, Firk, C, Konrad, K, Paschke, K, Neulen, J, Herpertz-dahlmann, B, et al. Pregnancy complications, substance abuse, and prenatal care predict birthweight in adolescent mothers. Arch Public Heal (2021) 79(137):137–9. doi:10.1186/s13690-021-00642-z
14. Anderson, MEL, Ronith, ELK, and Andres, RL. Social, ethical and practical aspects of perinatal substance use. J Subst Abuse Treat (1997) 14(5):481–6. doi:10.1016/s0740-5472(96)00152-3
15. Redding, BA, and Selleck, CS Perinatal substance abuse education: a review of existing curricula. Subst Abus (2009) 20(1):17–31. doi:10.1080/08897079909511391
16. Ordean, A, Graves, L, Chisamore, B, Greaves, L, and Dunlop, A. Prevalence and consequences of perinatal substance use — growing worldwide concerns. Subst Abus Res Treat (2017) 11:1178221817704692–4. doi:10.1177/1178221817704692
17. Popova, S, Lange, S, Probst, C, Gmel, G, and Rehm, J. Estimation of national, regional, and global prevalence of alcohol use during pregnancy and fetal alcohol syndrome: a systematic review and meta-analysis. Lancet Glob Heal (2017) 5:290–9. doi:10.1016/S2214-109X(17)30021-9
18. Behnke, M, Smith, VC, and On, CCommittee on Fetus and Newborn. Prenatal substance abuse: short- and long-term effects on the exposed fetus. Pediatrics (2013) 131(3):e1009–24. doi:10.1542/peds.2012-3931
19. Godwin, M, Green, S, Jones, H, and Robbins, SS. Perinatal substance use disorders treatment. N C Med J (2020) 81(1):36–40. doi:10.18043/ncm.81.1.36
20. Wilson, CA, Finch, E, Kerr, C, and Shakespeare, J. Alcohol, smoking, and other substance use in the perinatal period. BMJ (2020) 2020:m1627. doi:10.1136/bmj.m1627
21. Havens, JR, Ann, L, Shannon, LM, and Hansen, WF. Factors associated with substance use during pregnancy: results from a national sample. Drug Alcohol Depend (2009) 99:89–95. doi:10.1016/j.drugalcdep.2008.07.010
22. Burns, E, Gray, R, and Smith, LA. Brief screening questionnaires to identify problem drinking during pregnancy: a systematic review. Addiction (2010) 105:601–14. doi:10.1111/j.1360-0443.2009.02842.x
23. Fetene, MT, Teji, K, Assefa, N, Bayih, WA, Tsehaye, G, and Hailemeskel, HS Magnitude and associated factors of substance use among pregnant women attending antenatal care in public hospitals of eastern Ethiopia. BMC Psychiatry (2021) 21(96):96. doi:10.1186/s12888-021-03078-5
24. WHO ASSIST Working Group. The alcohol, smoking and substance involvement screening test (ASSIST): development, reliability and feasibility. Addiction (2002) 97:1183–94. doi:10.1046/j.1360-0443.2002.00185.x
25. Sainz, MT, Rosete-mohedano, MG, Rey, GN, Angélica, N, Vélez, M, García, SC, et al. Validity and reliability of the alcohol, smoking, and substance involvement screening test (ASSIST) in university students. ADICCIONES (2016) 28(1):19–27. doi:10.20882/adicciones.786
26. Damota, MD, and Robe, E. Depression, anxiety and stress among first year Addis Ababa University students: magnitude, and relationship with academic achievement. Depression (2018) 56.
27. Tran, TD, Tran, T, and Fisher, J. Validation of the depression anxiety stress scales (DASS) 21 as a screening instrument for depression and anxiety in a rural community-based cohort of northern Vietnamese women. BMC Psychiatry (2013) 13(24):24. doi:10.1186/1471-244X-13-24
28. Nordin, RB, Kaur, A, Soni, T, Por, LK, and Miranda, S. Construct validity and internal consistency reliability of the Malay version of the 21-item depression anxiety stress scale (Malay-DASS-21) among male outpatient clinic attendees in Johor. J Med J Malaysia (2017) 72(5):265.
29. Basha, E, and Kaya, M. Depression, anxiety and stress scale (DASS): the study of validity and reliability. Univers J Educ Res (2016) 4(12):2701–5. doi:10.13189/ujer.2016.041202
30. Pezirkianidis, C, Karakasidou, E, Lakioti, A, Stalikas, A, and Galanakis, M Psychometric properties of the depression, anxiety, stress scales-21 (DASS-21) in a Greek sample. Psychology (2018) 9:2933–50. doi:10.4236/psych.2018.915170
31. Dagnew, B, Andualem, Z, and Dagne, H Excessive daytime sleepiness and its predictors among medical and health science students of University of Gondar, Northwest Ethiopia: institution-based cross-sectional study. Health Qual Life Outcomes (2020) 18(1):299–7. doi:10.1186/s12955-020-01553-3
32. Manzar, MD, Salahuddin, M, Alamri, M, Albougami, A, Khan, MYA, Nureye, D, et al. Psychometric properties of the Epworth sleepiness scale in Ethiopian university students. Heal Qual Life Outcomes (2019) 17(1):30–9. doi:10.1186/s12955-019-1098-9
33. Smyka, M, Kosińska-Kaczyńska, K, Sochacki-Wójcicka, N, Zgliczyńska, M, and Wielgoś, M Sleep problems in pregnancy — a cross-sectional study in over 7000 pregnant women in Poland. Int J Environ Res Public Health (2020) 17(15):5306. doi:10.3390/ijerph17155306
34. Fernández-Alonso, AM, Trabalón-Pastor, M, and Chedraui, P. Factors related to insomnia and sleepiness in the late third trimester of pregnancy. Arch Gynecol Obs (2012) 86:55–61. doi:10.1007/s00404-012-2248-z
35. Bourjeily, G, Sabbagh, RE, Sawan, P, Raker, C, Wang, C, and Hott, B. Epworth sleepiness scale scores and adverse pregnancy outcomes. Sleep Breath (2013) 17:1125–6. doi:10.1007/s11325-013-0821-8
36. Sarberg, M, Bladh, M, Josefsson, A, and Svanborg, E. Sleepiness and sleep-disordered breathing during pregnancy. SLEEP Breath Physiol Disord (2016) 20:1231–7. doi:10.1007/s11325-016-1345-9
37. Moghadam, ZB, Rezaei, E, and Rahmani, A. Sleep disorders during pregnancy and postpartum: a systematic review. Korean Soc Sleep Med (2021) 12(2):81–93. doi:10.17241/smr.2021.00983
38. Adane, F, Seyoum, G, and Alamneh, YM. Non-prescribed drug use and predictors among pregnant women in Ethiopia: systematic review and meta-analysis. J Matern Neonatal Med (2020) 0(0):4273–84. doi:10.1080/14767058.2020.1849105
39. Tabatabaei, SM, Behmanesh-Pour, F, Salimi-Khorashad, A, Zaboli, M, Sargazi-Moakhar, ZS-MS, and Shaare-Mollashahi, S Substance abuse and its associated factors among pregnant women: a cross-sectional study in the southeast of Iran. Addict Heal (2018) 10(3):162–72. doi:10.22122/ahj.v10i3.209
40. Aklog, T, Tiruneh, G, and Tsegay, G. Assessment of substance abuse and associated factors among students of Debre Markos Poly Technique college in Debre Markos town, East Gojjam zone, Amhara regional state, Ethiopia. Glob J Med Res (2013) 13:4–9.
41. Berghella, V, Blake-lamb, T, Guille, C, Landau, R, and Minkoff, H. Substance use disorders in pregnancy: clinical, ethical, and research imperatives of the opioid epidemic: a report of a joint workshop of the Society for Maternal-Fetal Medicine, American College of Obstetricians and Gynecologists, and American Society of. Am J Obstet Gynecol (2019) 221(1). doi:10.1016/j.ajog.2019.03.022
42. Louw, K. Substance use in pregnancy: the medical challenge. Obstet Med (2018) 11(2):54–66. doi:10.1177/1753495X17750299
43. Forray, A, and Foster, D Substance use in the perinatal period. Curr Psychiatry Rep (2015) 17(11):91. doi:10.1007/s11920-015-0626-5
44. Han, BH, Termine, DJ, Moore, AA, Sherman, SE, and Palamar, JJ. Medical multimorbidity and drug use among adults in the United States. Prev Med Rep (2018) 12:214–9. doi:10.1016/j.pmedr.2018.10.007
45. Tracy, L, and Simpson, WRM. Concomitance between childhood sexual and physical abuse and substance use problems. A review. Clin Psychol Rev (2002) 22:27–77. doi:10.1016/s0272-7358(00)00088-x
Keywords: perinatal substance use, pregnancy, women, substance use, Ethiopia
Citation: Seid J, Mohammed E and Muktar Y (2023) Factors associated with perinatal substance use among Ethiopian women: an institutional-based cross-sectional study. Adv. Drug Alcohol Res. 3:11913. doi: 10.3389/adar.2023.11913
Received: 12 August 2023; Accepted: 27 September 2023;
Published: 15 November 2023.
Edited by:
Emmanuel Onaivi, William Paterson University, United StatesReviewed by:
Ephrem Engidawork, Addis Ababa University, EthiopiaFantahun Andualem, University of Gondar, Ethiopia
Mulugeta Akele, Mizan Tepi University, Ethiopia
Copyright © 2023 Seid, Mohammed and Muktar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jemal Seid, amVtYWxzMjgzQGdtYWlsLmNvbQ==
 Jemal Seid
Jemal Seid Emam Mohammed2
Emam Mohammed2