Abstract
Aim:
This study evaluates the impact of the minimal incision repair of rectus abdominis diastasis (MIRRAD) procedure on physical activity, muscle strength, quality of life, and overall satisfaction in women with postpartum rectus abdominis diastasis (PP-RAD).
Methods:
A cohort of 31 female patients, aged 20–50 years, diagnosed with PP-RAD unresponsive to conservative treatment, underwent the MIRRAD procedure. Assessments were conducted preoperatively and 1 year postoperatively, these included the Modified Abdominal Trunk Function Protocol (MATFP), Disability Rating Index (DRI), and Urinary Disability Index (UDI) questionnaires. Physical activity intensity was monitored using accelerometers.
Results:
Significant improvements were observed in vigorous physical activities (Z = −2.352, p = 0.019), vector magnitude counts per minute (Z = −2.163, p = 0.031), and steps per minute (Z = −3.131, p = 0.002). DRI showed significant improvements in physical tasks like dressing, walking, and strenuous work (Z ranging from −2.705 to −4.603, p < 0.001). UDI indicated significant improvements in urinary symptoms, including reduced frequency (Z = −2.984, p = 0.003) and less urinary leakage (Z = −2.357, p = 0.018). MATFP demonstrated gains in back and abdominal muscle strength (Z = −4.321, p < 0.001) and trunk stability (Z = −3.991, p < 0.001).
Conclusion:
The MIRRAD procedure significantly improves physical strength, trunk stability, and urinary function, enhancing daily activities and overall physical health in women with PP-RAD. Further research is recommended to evaluate long-term outcomes.
Introduction
Rectus Abdominis Diastasis (RAD) is defined as separation of the rectus muscles by more than 2 cm [1]. It is a common condition where separation of the rectus abdominis muscles results in a widening of the linea alba, the connective tissue running down the midline of the abdomen. This separation is often due to increased intra-abdominal pressure and hormonal changes, which can arise for various reasons, most notably during pregnancy. The expanding uterus can stretch the abdominal wall, leading to RAD during pregnancy. This usually reverts, but in some women this leads to postpartum rectus abdominis diastasis (PP-RAD) [2].
PP-RAD can cause significant functional impairments and a range of symptoms. A primary concern is the instability and weakness of the abdominal wall resulting from compromised muscular and fascial integrity. This instability can weaken core strength and trunk function, potentially affecting the pelvic floor muscles. The condition manifests with both direct and indirect symptoms that can significantly impact daily life and physical activities.
Direct symptoms of PP-RAD include a visible bulge or “pooch” along the midline of the abdomen, especially noticeable during activities that engage the abdominal muscles such as sit-ups or lifting. This can lead to abdominal discomfort and a sense of weakness due to the lack of adequate core support. Research also indicates that PP-RAD can impair trunk biomechanics, triggering a series of musculoskeletal problems [3, 4].
Indirect symptoms linked to PP-RAD include low back pain, pelvic discomfort, and urinary stress incontinence. These occur because the abdominal and pelvic floor muscles provide less support, crucial for maintaining posture, spinal stability, and continence. Studies have shown that women with PP-RAD often report reduced quality of life due to these symptoms, experiencing difficulties in performing everyday tasks, participating in physical activities, or returning to pre-pregnancy exercise routines [1, 2, 5].
In addition to physical symptoms, PP-RAD can have substantial psychological effects. Many women report a negative body image and diminished self-confidence, as the persistent abdominal bulge can make them appear “pregnant,” causing social discomfort and emotional distress. Recent studies have linked these body image issues with lower self-esteem and a reluctance to engage in social or physical activities [6].
Complications associated with PP-RAD include an increased risk for hernias along the linea alba, particularly midline hernias where abdominal contents protrude through the weakened fascia. Additionally, PP-RAD can lead to hyperlordosis [7].
Recent research has advanced our understanding of RAD complications and management strategies. A 2021 systematic review published in the Journal of Women’s Health Physical Therapy highlighted the effectiveness of targeted physiotherapy interventions in managing PP-RAD symptoms [4]. These interventions focus on strengthening deep abdominal muscles and improving pelvic floor function, which can alleviate symptoms like low back pain and incontinence. Studies have shown that surgical correction of PP-RAD enhances functional outcomes such as core strength and pelvic stability. Women who opted for surgical repair reported higher satisfaction with their body image and fewer symptoms related to back pain and urinary incontinence compared to those who chose conservative management [8, 9].
While some women may find relief through physiotherapy and lifestyle modifications, others, particularly those with severe diastasis or associated hernias, may require surgical intervention. A comprehensive understanding of the wide range of symptoms and treatment options is crucial for providing holistic care that addresses both the physical and psychological impacts of PP-RAD [10, 11].
In conclusion, PP-RAD is more than a cosmetic concern; it has profound implications for core function, posture, and overall quality of life. Continued research is refining our understanding and management of this condition, offering hope for effective treatments that enhance both the physical and emotional wellbeing of these women.
The aim of this study was to evaluate the impact of a minimally incision repair of rectus abdominis diastasis procedure on quality of life and daily function.
Materials and Methods
Study Design and Participants
This prospective study included women diagnosed with postpartum rectus abdominis diastasis (PP-RAD) with an inter-rectus distance of ≥3 cm. The study was conducted at the Hernia Center, Region Örebro Län, Sweden, from October 2021 to August 2024. The study has been registered at ClinicalTrials.gov. All procedures were performed in compliance with the European Union’s General Data Protection Regulation (GDPR).
Inclusion Criteria:
• Female patients aged 20–50 years.
• Diagnosed with PP-RAD with an inter-rectus distance of ≥3 cm.
• At least 12 months postpartum and Unresponsive to conservative treatment.
• Decided against future pregnancies.
• No previous surgery involving the linea alba.
Exclusion Criteria:
• Inability or unwillingness to provide informed consent.
• Contraindications to general anesthesia.
• Pregnant or plan to become pregnant in the future.
• BMI >32 kg/m2
These patients, aged between 20 and 50 years, were all diagnosed with a minimum inter-rectus separation of 3 cm. After attempting conservative treatment without satisfactory improvement, they opted for surgical repair. To be eligible for the study, participants were required to be at least 1 year postpartum and to have decided against future pregnancies, as per the study criteria. All participants received comprehensive information about the study, both verbally and in writing.
A total of 50 patients were assessed for eligibility. Of these, 33 met the inclusion criteria and provided informed consent to participate in the study. A flowchart detailing patient selection, inclusion, exclusion, and follow-up is presented in Figure 1.
FIGURE 1
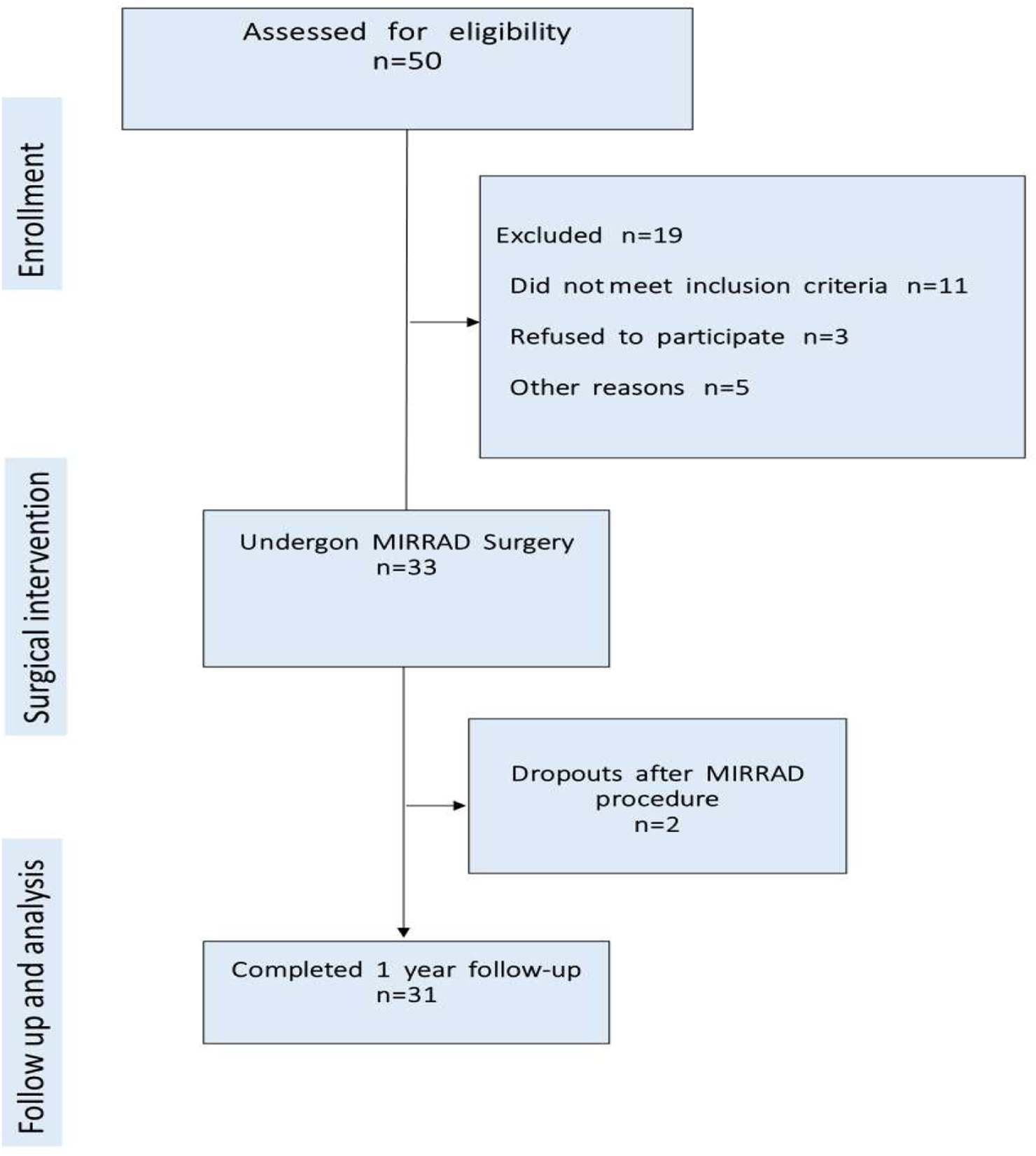
Patient election and follow-up.
The primary outcomes assessed were improvements in physical health and overall life satisfaction.
Reasons for Exclusion
Out of 50 eligible patients assessed, 19 were excluded prior to surgery for reasons including not meet inclusion criteria (11), refusal to participate (3), seeking repairs elsewhere (3) and undergoing surgery elsewhere (2). Consequently, 33 patients underwent MIRRAD procedure. Two patients were excluded post-surgery, resulting in a final analysis of 31 patients.
Most patients were referred to the Hernia Center due to a diagnosed hernia or suspected hernia in the linea alba. All patients had at least one hernia, with the majority having hernias measuring ≤1 cm. Additionally, all patients presented with an inter-rectus distance (D2 H1) of at least 3 cm, with a mean width of 4.4 cm (SD ± 1.0 cm) (Table 1).
TABLE 1
| T (Type) | D (inter-rectus distance) | H (concomitant umbilical and/or epigastric hernia) |
|---|---|---|
| T1 = after pregnancy | D1 = >2 cm | H0 = Without |
| D2 = >3–5 cm | ||
| T2 = With adiposity | H1 = Present | |
| D3 = >5 cm |
European Hernia Society (EHS) classification of RD guidelines.
Each participant completed the Disability Rating Index (DRI), the Urogenital Distress Inventory-6 (UDI-6), and the Incontinence Impact Questionnaire-7 (IIQ-7) both before the surgery and 1 year postoperatively [12, 13]. Additionally, they underwent a Modified Abdominal Trunk Function Protocol (MATFP) assessment, conducted by a certified physiotherapist, both preoperatively and 1 year after the surgical repair [14]. Before surgery, participants were also provided with an accelerometer to monitor their physical activity levels.
MIRRAD Procedure
Minimally Incision Repair of Rectus Abdominis Diastasis (MIRRAD) surgery is a minimal incision procedure to plicate PP-RAD. The procedure is performed under general anaesthesia through a small skin incision near the umbilicus. It involves the plication of the rectus abdominis diastasis using barbed sutures as double-line suture, and if a concomitant hernia is found, it is sutured with 2.0 prolene before the plication. The umbilicus is then reattached to the fascia with single stitch of 4-0 PDS. The skin is closed with absorbable intradermal 3.0 Monocryl sutures, allowing for same-day discharge, which reduces hospital stay and cost Figure 2. All patients were provided an elastic abdominal binder before surgery and were advised to use it 6 weeks postoperatively. The hernia defects were repaired using non-absorbable sutures, while the rectus diastasis was closed with a 0-PDS double-lined barbed suture. All procedures were performed by the same experienced consultant surgeon at the Hernia Center, Region Örebro Län, Sweden. This repair method utilized an open surgical approach through a small skin incision near the umbilicus. While achieving similar results to the SCOLA method, the MIRRAD technique does not require mesh reinforcement. This method may serve as a bridge between traditional open surgeries and advanced laparoscopic techniques, offering a cost-effective and efficient solution for abdominal wall reconstruction. This technique is particularly appealing to patients seeking a less invasive option, delivering a balance between effective repair and a faster recovery.
FIGURE 2
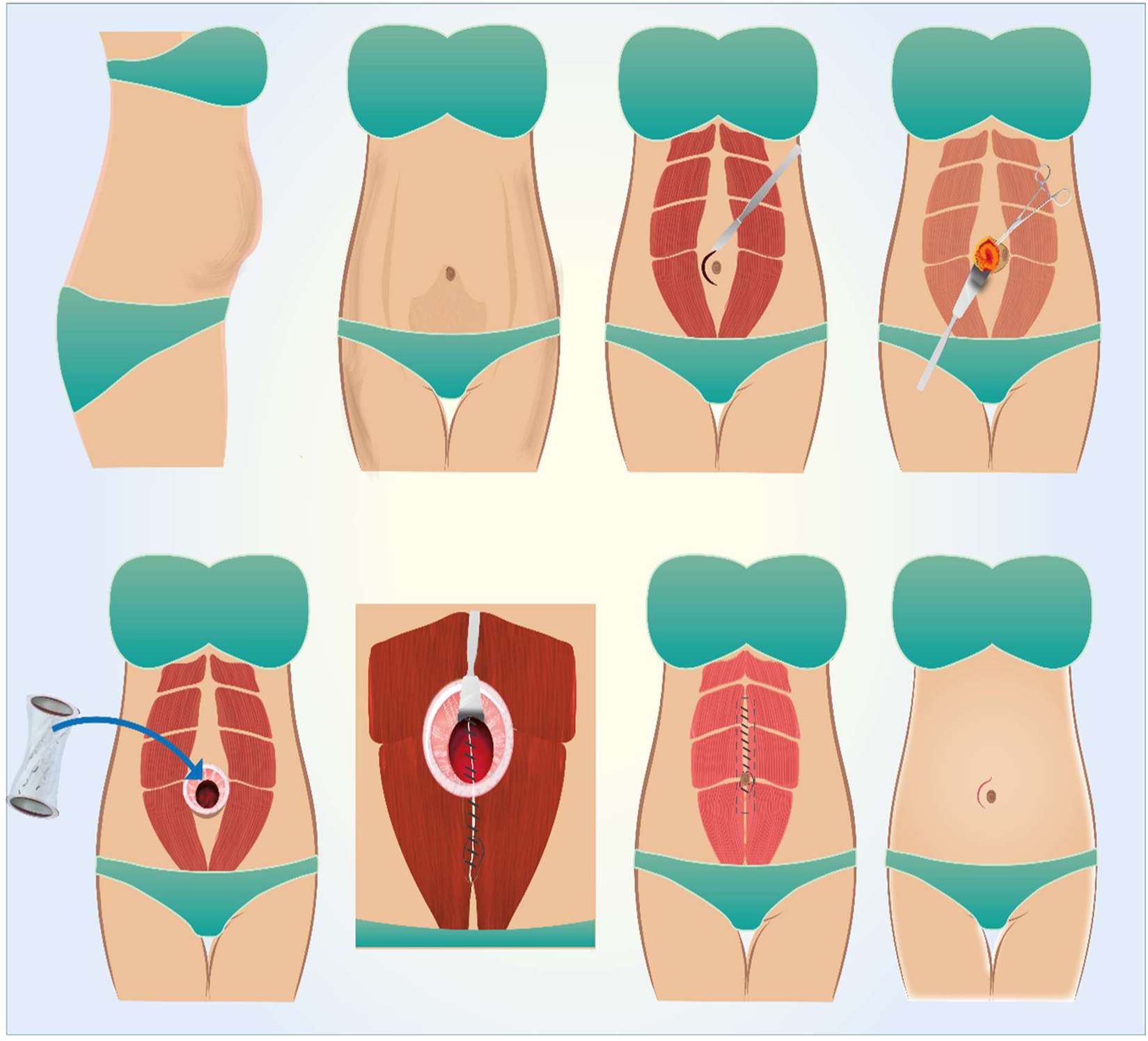
Illustrating the MIRRAD repair procedure. Illust. from the author’s library.
Data Collection and Analysis
All women included in the study were aged between 20 and 50 years, with a BMI range of 18.8–30.1. None of the participants had undergone previous surgery involving the linea alba. According to the study protocol, all women were enrolled at least 12 months after their most recent delivery and had decided not to pursue further pregnancies. Current illnesses (classified by ICD codes) and ongoing medications were recorded for all participants.
Data were collected electronically using Greenlight Guru Clinical (formerly Smart-trial) software. All data was stored according to the European data protection policy. Standardized assessments were conducted preoperatively and at 1 year postoperatively. An accelerometer is a device that measures acceleration forces in one or more directions, typically in three axes: X (horizontal), Y (vertical), and Z (depth). It detects changes in velocity over time, which can be used to measure motion, orientation, and vibration. It works by sensing motion through tiny sensors called MEMS (Micro-Electro-Mechanical Systems). These parts move when the device moves, generating an electrical signal that the device uses to calculate acceleration. The participants carried the device at all times while awake (except during showers and baths) for 5 days. After this period, they returned the device in a padded envelope to the principal researcher for computerised analysis. Each participant also kept a simple activity diary during this period with the accelerometer.
Physical Function and Strength Assessments
Modified Abdominal Trunk Function Protocol (MATFP): Conducted by a certified physiotherapist to evaluate abdominal wall strength and trunk stability.
Accelerometer Monitoring: Physical activity levels were measured using ActiGraph wGT3X-BT accelerometers over five consecutive days. Participants were instructed to wear the device during waking hours, except during bathing or swimming.
Questionnaires
Disability Rating Index (DRI): Assessed the impact of symptoms on daily activities.
Urogenital Distress Inventory-6 (UDI-6): Evaluated urinary symptoms.
Incontinence Impact Questionnaire-7 (IIQ-7): Measured the impact of urinary incontinence on quality of life.
Pain Assessment: Visual Analogue Scale (VAS): Used to measure postoperative pain at 4 h, 1 week, and 1 month after surgery.
Statistical Analysis
Data were exported to IBM SPSS Statistics version 29.0.0.0 for analysis. Continuous variables were expressed as mean ± standard deviation (SD) or median with interquartile range (IQR) as appropriate. The Wilcoxon signed-rank test was used to compare preoperative and postoperative outcomes. A p-value of <0.05 was considered statistically significant.
Ethical Considerations
The study was conducted in accordance with the Declaration of Helsinki and complied with the GDPR for data protection. All participants provided written informed consent after receiving detailed information about the study’s purpose, procedures, and potential risks and benefits. The study was approved (Dnr. 2021-04599) by the Swedish Board of Ethics (Etikprövningsmyndigheten).
Recovery and Follow-Up
All study patients were followed up clinically by a surgeon and a physiotherapist 1 year after the procedure. Patients were encouraged to contact the clinic if they experienced any signs of complications. If any complications were suspected, the patient was invited for an additional visit, which included clinical examination, laboratory tests, or radiological assessment as necessary. All events related to the procedure were documented in Smart-trial, and additional visits were scheduled according to local protocols. Additionally, all patients were provided with an abdominal binder and advised to use it for 6 weeks postoperatively.
Results
Patient Enrollment and Follow-Up
Out of 50 patients assessed, 33 met the inclusion criteria and were enrolled in the study. Two patients did not participate in the 1-year follow-up. One cited the long distance to the hospital, and the other provided no explanation. Both reported no complications at the 1-month postoperative follow-up. One-year follow-up data were successfully collected from the 31 participants who completed the study (Figure 1). Mean preoperative inter-rectus distance was 4.4 ± 1.0 cm. All participants were at least 1 year postpartum and had decided against future pregnancies. At the 1-year follow-up, no cases of hernia or rectus diastasis recurrence were reported. Two patients developed seromas, confirmed radiologically at 1 week and 1-month postoperative. Nausea was reported by five patients. No other surgery-related complications were observed. Postoperative pain was assessed using a Visual Analogue Scale (VAS), with mean pain scores of 2.8 at 4 h, 3.2 at 1 week, and 1.7 at 1 month following surgery.
The Wilcoxon signed rank test showed statistically significant improvements in physical activities, strength, and overall functional ability 1 year postoperatively compared to preoperative assessments. The analysis demonstrated significant enhancements in physical activities, strength, and overall ability. Notable reductions were recorded in urinary frequency, urinary leakage, and pain, alongside improvements in the ability to engage in leisure activities.
However, trends in household chores, travelling, and social activities did not reach statistical significance.
Accelerometer
Data were collected pre- and postoperatively to assess changes in physical activity. A Wilcoxon signed rank test revealed significant improvements in vigorous activities (Z = −2.352, p = 0.019), vector magnitude counts per minute (Z = −2.163, p = 0.031), and steps per minute (Z = −3.131, p = 0.002), indicating enhanced physical performance following surgery (Table 2).
TABLE 2
| Type of physical activity (preoperative vs. postoperative) | Z | P-value |
|---|---|---|
| Light physical activity - preoperative vs. postoperative | −1.207 | 0.227 |
| Moderate physical activity - preoperative vs. postoperative | −1.731 | 0.083 |
| Vigorous physical activity - preoperative vs. postoperative | −2.352 | 0.019 |
| Vector_Magnitude_CPM | −2.163 | 0.031 |
| Steps Per Minute - preoperative vs. postoperative | −3.131 | 0.002 |
Accelerometer data summary using count per minute (CPM).
Wilcoxon Signed Rank Test. Based on positive rank.
Source: Katawazai et al., 2025.
Disability Rating Index (DRI)
The postoperative data showed significant improvements across all assessed activities. Dressing and undressing without assistance showed a statistically significant improvement (p = 0.048). Walking, climbing stairs, sitting for an extended period, standing bent over a sink, carrying a bag or package, making a bed, running, performing light physical work, performing strenuous physical work, and engaging in exercise or sports all demonstrated highly significant improvements, with Z values ranging from −2.705 to −4.603 and (p- < 0.001). Overall, the results show considerable improvements in physical abilities and daily activities 1 year after the procedure (Table 3).
TABLE 3
| Type of activity (Preoperative vs. postoperative) | Z | P-value |
|---|---|---|
| Dressing and undressing without assistance – Preop. Vs. postop. | −1.974a | <0.048 |
| Walking – Preop. Vs. postop. | −3.466a | <0.001 |
| Climbing stairs – Preop. Vs. postop. | −3.450a | <0.001 |
| Sitting for an extended period – Preop. Vs. postop. | −3.798a | <0.001 |
| Standing bent over a sink – Preop. Vs. postop. | −3.357a | <0.001 |
| Carrying a bag or package – Preop. Vs. postop. | −4.023a | <0.001 |
| Making a bed – Preop. Vs. postop. | −2.705a | <0.001 |
| Running – Preop. Vs. postop. | −3.933a | <0.001 |
| Physical work – Preop. Vs. postop. | −3.836a | <0.001 |
| Strenuous physical work – Preop. Vs. postop. | −4.603a | <0.001 |
| Exercise/sports – Preop. Vs. postop. | −4.389a | <0.001 |
DRI activity improvements pre- and 1-year post-operative.
Wilcoxon Signed Rank Test.
Based on positive rank.
Source: Katawazai et al., 2025.
Urogenital Distress Inventory-6, Incontinence Impact Questionnaire−7 (UDI-6, IIQ-7)
The postoperative results show significant improvements in several areas. There was a notable reduction in the frequency of urination and in urinary urgency incontinence associated with physical activity, coughing, or sneezing. Minor leakage incidents also decreased significantly. Additionally, improvements were observed in difficulty emptying the bladder and in pain or discomfort in the lower abdomen or genital area.
Significant improvements were also seen in leisure activities and mental health, with a reduction in frustration levels. There were trends towards improvement in performing household chores, travelling, and participating in social activities, although these were not statistically significant (Table 4).
TABLE 4
| Type of activity/Symptom (Preoperative vs. postoperative) | Z | P-value |
|---|---|---|
| Need to go to the bathroom very often – Preop. Vs. postop. | −2.984a | 0.003 |
| Urinary leakage associated with a strong need to urinate – Preop. Vs. postop. | −2.357a | 0.018 |
| Urinary leakage associated with physical activity, coughing, or sneezing – Preop. Vs. postop. | −2.289a | 0.022 |
| Small amounts of urinary leakage (drops) – Preop. Vs. postop. | −3.000a | 0.003 |
| Postop._Difficulty emptying the bladder – Preop. Vs. postop. | −2.352a | 0.019 |
| Pain or discomfort in the lower abdomen or genital area – Preop. Vs. postop. | −2.951a | 0.003 |
| Postop._Ability to perform household chores (cooking, cleaning, laundry) – Preop. Vs. postop. | −1.732a | 0.083 |
| Postop._Leisure activities such as walking, swimming, or other physical activities – Preop. Vs. postop. | −3.957a | <0.001 |
| Entertainment (e.g., movies, concerts) – Preop. Vs. postop. | −0.378a | 0.705 |
| Ability to travel by car or bus more than 30 min from home – Preop. Vs. postop. | −1.890a | 0.059 |
| Participation in social activities outside the home – Preop. Vs. postop. | −1.811a | 0.070 |
| Mental health (nervousness, depression, etc.) – Preop. Vs. postop. | −2.887a | 0.004 |
| I feel prevented from doing what I want – Preop. Vs. postop. | −3.106a | 0.002 |
UDI-6 and IIQ-7 results pre- and 1-year post-operation.
Wilcoxon Signed Rank Test.
Based on negative rank.
Source: Katawazai et al., 2025.
Modified Abdominal Trunk Function Protocol Assessment (MATFP)
The postoperative results showed significant improvements in muscle strength and trunk stability compared to the preoperative state. Both back and abdominal muscle strength increased significantly after the procedure, as did trunk stability in the side plank exercise. There were also notable improvements in overall levels reached in the assessment. Overall, these results indicate considerable gains in muscle strength and trunk stability following the procedure (Table 5).
TABLE 5
| MATFP results (preoperative vs. postoperative) | Z | P-value |
|---|---|---|
| Back muscle strength (number of seconds) – Preop. Vs. postop. | −4.206a | <0.001 |
| Abdominal muscle strength (number of seconds) – Preop. Vs. postop. | −4.321a | <0.001 |
| Trunk stability in side-plank (Side plank) (seconds) – Preop. Vs. postop. | −3.991a | <0.001 |
| Reached level – Preop. Vs. postop. | −3.328a | <0.001 |
| Lifting right leg – Preop. Vs. postop. | −2.646a | 0.008 |
| Lifting left leg – Preop. Vs. postop. | −1.265a | 0.206 |
MATFP results pre- and 1-year post-operation.
Wilcoxon Signed Rank Test.
Based on positive rank.
Source: Katawazai et al., 2025.
Patient Satisfaction
All patients rated their satisfaction with their operation on a scale from 0 to 10 (out of 10), with a mean score of 8.65, indicating high satisfaction. Postoperative pain and discomfort levels were rated from 1 to 6 (out of 10), with an average of 2.32, suggesting low to moderate discomfort after surgery (Table 6).
TABLE 6
| N | Minimum | Maximum | Mean | Std. Deviation | |
|---|---|---|---|---|---|
| How satisfied is the patient with the operation? | 31 | 2 | 10 | 8.6 | 1.7 |
| How much discomfort has the patient experienced after the diastasis surgery? | 31 | 1 | 6 | 2.3 | 1.3 |
Patient satisfaction and discomfort scores.
Source: Katawazai et al., 2025.
Regarding abdominal wall stability 1-year post-surgery, 83.9% of patients reported feeling either quite better or much better, while only one patient reported no difference.
In summary, surgery resulted in high patient satisfaction, low postoperative pain and discomfort, and significant improvements in abdominal wall stability.
Discussion
Summary of Findings
In conclusion, the MIRRAD procedure significantly improves physical strength, trunk stability, and urinary function in women with PP-RAD. One year postoperatively, participants showed significant enhancements in physical activities, reduced urinary symptoms, and improved quality of life.
Physical Function and Strength Improvements
The significant gains in back and abdominal muscle strength and trunk stability indicate the effectiveness of the MIRRAD procedure in restoring core muscle function. These improvements facilitated better performance in daily activities such as dressing, climbing stairs, and engaging in exercise, aligning with previous studies that highlight the benefits of surgical intervention for PP-RAD.
Urinary and Pain-Related Outcomes
The significant reduction in urinary frequency, urgency, and leakage suggests that repairing the rectus diastasis positively impacts pelvic floor function. Improvements in pain and discomfort, as well as better leisure activities and mental health, highlight the comprehensive benefits of MIRRAD procedure beyond mere physical strength.
Limitations and Strengths
This study has some limitations, the relatively small sample size of 31 patients may limit the generalizability of the findings. The lack of a control group prevents definitive conclusions about the procedure’s efficacy compared to non-surgical interventions. A 1-year follow-up may not capture long-term outcomes and potential late-onset complications. Despite these constraints, the study’s strengths include its prospective design and the use of validated outcome measures, which we believe add valuable insights into the treatment of rectus diastasis.
Future studies should include larger cohorts, control groups, and extended follow-up periods to validate these findings and assess the long-term effectiveness and safety of the MIRRAD procedure.
Conclusion
The MIRRAD surgical procedure is effective in improving physical strength, trunk stability, and urinary function in women with PP-RAD. The technique offers a minimally invasive option with minimal complications and significant improvements in quality of life. Despite the study’s limitations, the findings contribute valuable insights and support the use of MIRRAD as a viable surgical intervention for PP-RAD.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Swedish Ethical Review Authority. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
AK wrote the study plan, which was approved by GS and GW. The study was conducted by the corresponding author and supervised by GS and GW. All study participants were examined before and 1 year after surgery using MATFP by AÄ. Data interpretation and analysis were performed by AK and GS, with the manuscript reviewed by all authors. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontierspartnerships.org/articles/10.3389/jaws.2024.13830/full#supplementary-material
Abbreviations
MIRRAD, Minimal Incision Repair of Rectus Abdominis Diastasis; RAD, Rectus Abdominis Diastasis; PP-RAD, Postpartum Rectus Abdominis Diastasis; MATFP, Modified Abdominal Trunk Function Protocol; VAS, Visual Analogue Scale; DRI, Disability Rating Index; UDI-6, IIQ-7, Urogenital Distress Inventory-6, Incontinence Impact Questionnaire −7; VHPQ, Ventral Hernia Pain Questionnaire.
References
1.
Hernández-Granados P Henriksen NA Berrevoet F Cuccurullo D López-Cano M Nienhuijs S et al European Hernia Society Guidelines on Management of Rectus Diastasis. Br J Surg (2021) 108(10):1189–91. 10.1093/bjs/znab128
2.
Wu L Gu Y Gu Y Wang Y Lu X Zhu C et al Diastasis Recti Abdominis in Adult Women Based on Abdominal Computed Tomography Imaging: Prevalence, Risk Factors and its Impact on Life. J Clin Nurs (2021) 30(3-4):518–27. 10.1111/jocn.15568
3.
Hills NF Graham RB McLean L . Comparison of Trunk Muscle Function Between Women With and Without Diastasis Recti Abdominis at 1 Year Postpartum. Phys Ther (2018) 98(10):891–901. 10.1093/ptj/pzy083
4.
Benjamin D Van de Water A Peiris C . Effects of Exercise on Diastasis of the Rectus Abdominis Muscle in the Antenatal and Postnatal Periods: A Systematic Review. Physiotherapy (2014) 100(1):1–8. 10.1016/j.physio.2013.08.005
5.
Kim S Yi D Yim J . The Effect of Core Exercise Using Online Videoconferencing Platform and Offline-Based Intervention in Postpartum Woman With Diastasis Recti Abdominis. Int J Environ Res Public Health (2022) 19(12):7031. 10.3390/ijerph19127031
6.
Gluppe S Ellström Engh M Bø K . Primiparous Women’s Knowledge of Diastasis Recti Abdominis, Concerns About Abdominal Appearance, Treatments, and Perceived Abdominal Muscle Strength 6–8 Months Postpartum. A Cross Sectional Comparison Study. BMC women’s health (2022) 22(1):428. 10.1186/s12905-022-02009-0
7.
Katawazai A Wallin G Sandblom G . Long-Term Reoperation Rate Following Primary Ventral Hernia Repair: A Register-Based Study. Hernia (2022) 26(6):1551–9. 10.1007/s10029-022-02645-3
8.
Emanuelsson P Gunnarsson U Dahlstrand U Strigård K Stark B . Operative Correction of Abdominal Rectus Diastasis (ARD) Reduces Pain and Improves Abdominal Wall Muscle Strength: A Randomized, Prospective Trial Comparing Retromuscular Mesh Repair to Double-Row, Self-Retaining Sutures. Surgery (2016) 160(5):1367–75. 10.1016/j.surg.2016.05.035
9.
Olsson A Kiwanuka O Wilhelmsson S Sandblom G Stackelberg O . Surgical Repair of Diastasis Recti Abdominis Provides Long-Term Improvement of Abdominal Core Function and Quality of Life: A 3-Year Follow-Up. BJS open (2021) 5(5):zrab085. 10.1093/bjsopen/zrab085
10.
Benjamin DR Frawley HC Shields N Peiris CL van de Water ATM Bruder AM et al Conservative Interventions May Have Little Effect on Reducing Diastasis of the Rectus Abdominis in Postnatal Women - A Systematic Review and Meta-Analysis. Physiotherapy (2023) 119:54–71. 10.1016/j.physio.2023.02.002
11.
Gluppe SL Hilde G Tennfjord MK Engh ME Bø K . Effect of a Postpartum Training Program on the Prevalence of Diastasis Recti Abdominis in Postpartum Primiparous Women: A Randomized Controlled Trial. Phys Ther (2018) 98(4):260–8. 10.1093/ptj/pzy008
12.
Shumaker SA Wyman JF Uebersax JS McClish D Fantl JA . Health-Related Quality of Life Measures for Women With Urinary Incontinence: The Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program in Women (CPW) Research Group. Qual Life Res (1994) 3(5):291–306. 10.1007/BF00451721
13.
Salén BA Spangfort EV Nygren AL Nordemar R . The Disability Rating Index: An Instrument for the Assessment of Disability in Clinical Settings. J Clin Epidemiol (1994) 47(12):1423–35. 10.1016/0895-4356(94)90086-8
14.
Olsson A Kiwanuka O Wilhelmsson S Sandblom G Stackelberg O . Surgical Repair of Diastasis Recti Abdominis Provides Long-Term Improvement of Abdominal Core Function and Quality of Life: A 3-Year Follow-Up. BJS Open (2021) 5(5):zrab085. 10.1093/bjsopen/zrab085
Summary
Keywords
rectus abdominis diastasis, quality of life, ventral hernia, linea alba, postpartum rectus diastasis
Citation
Katawazai A, Wallin G, Ärlebäck A and Sandblom G (2025) Impact of Minimal Incision Repair of Rectus Abdominis Diastasis on Quality of Life and Stress Incontinence: A Prospective Study. J. Abdom. Wall Surg. 3:13830. doi: 10.3389/jaws.2024.13830
Received
19 September 2024
Accepted
19 December 2024
Published
04 February 2025
Volume
3 - 2024
Updates
Copyright
© 2025 Katawazai, Wallin, Ärlebäck and Sandblom.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Asmatullah Katawazai, asmatullah.katawazai@regionorebrolan.se
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.