Dear Editors,
Autoimmune/inflammatory syndrome induced by adjuvants (ASIA) is an immune-mediated disorder triggered by exposure to different substances, most of which are used in cosmetic plastic surgery, such as paraffin and silicone [1]. Several reports relate ASIA with severe dermatomyositis (DM). We report a case of anti-melanoma differentiation-associated gene 5 (MDA5) antibody-positive clinically amyopathic DM (CADM) associated with prior silicone breast implants (SBIs), which had a favorable prognosis.
A 49-year-old female patient who underwent bilateral mammoplasty 11 years ago was referred to our hospital because of erythematous hyperkeratosis on her palms and soles (Figures 1A, B), these skin lesions had been appeared for 2 months. The patient presented with periungual erythema, Gottron’s sign, and erythema in the nasal alar and upper back areas. In the fingertips of the upper extremities, vasodilation of the nail bed was observed using a dermoscopy. Moreover, the palm area was a finding of inverse Gottron’s sign, which was characteristic of anti-MDA5 antibody-positive. The patient had no clinical muscle weakness. Blood samples revealed normal serum creatine kinase and high KL-6 levels (600 U/mL) with elevated anti-MDA5 antibodies (7200; normal range <32 by ELISA). All other autoantibodies (nuclear, DNA, RNP, Smith, Aminoacyl-tRNA Synthetase, transcription intermediary factor 1-γ and Mi-2) were negative. Chest computed tomography detected a slight ground-glass shadow in the left upper lobe and a silicone bag in both breasts (Figure 1C). Moreover, the buttocks and vastus lateralis muscles showed increased signal intensity on magnetic resonance imaging. Skin biopsy revealed hyperkeratosis and liquefaction degeneration of the epidermis, lymphocytic infiltration around blood vessels, and edema of the upper layer (Figure 1D). The rheumatologist in our hospital administered oral 60 mg (1 mg/kg/day) of prednisolone and 150 mg of cyclosporine to the patient, and the arthritis and skin rash improved within 1 week. Steroids were tapered, and symptoms improved. We are suggesting that the patient undergo resection of the SBI, but consent is not obtained yet. Three years after starting treatment, the dose of prednisone is reduced to 7 mg (0.12 mg/kg/day), and there has been no recurrence of the skin lesions or pneumonia.
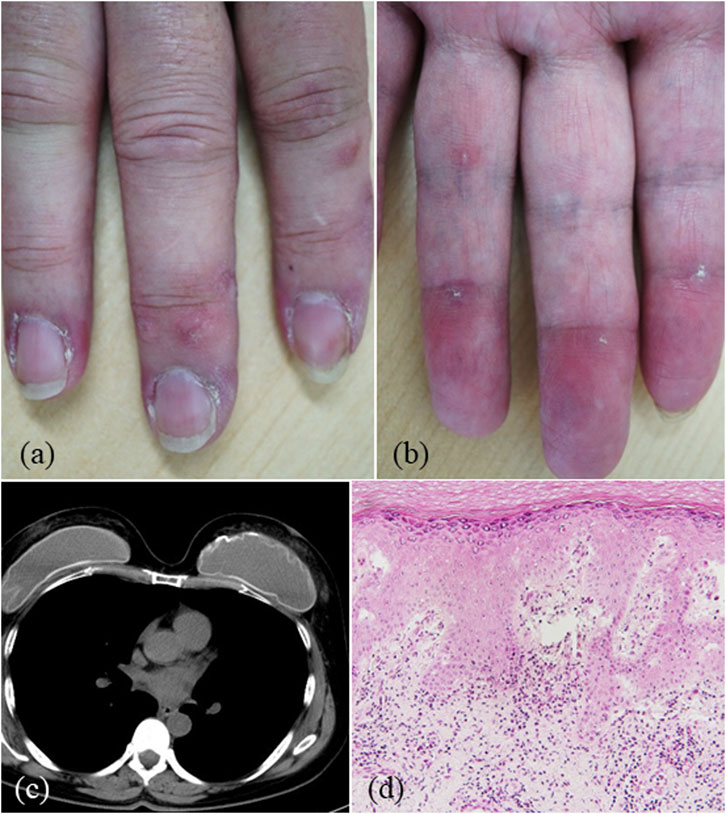
Figure 1. (A,B) Clinical findings: erythematous hyperkeratosis of the palms. (C) Chest computed tomography revealing silicone breast implants. (D) Pathological findings (Hematoxylin Eosin: ×200): hyperkeratosis and liquefaction degeneration of the epidermis, lymphocyte infiltration around blood vessels, and edema in the upper layer.
To our knowledge, seven cases of DM have been reported as ASIA, developing after SBI surgery. This includes two intractable cases that improved after SBI removal, and cases that developed after SBI rupture [2, 3] (Supplementary Table). These cases suggest a potential association between SBI and DM. However, there are also reports of DM occurring without SBI rupture, as in our case. Imanaka et al. [2] speculated on possible silicone gel migration throughout the elastomeric shell of the intact breast implant into the surrounding tissue producing an immune response.
Since 1945 in Japan, hydrocarbon-based substances, such as paraffin and petrolatum, and silicone-based substances, such as silicone oil and silicone gel, have been injected. Hence, foreign body granulomas and foreign substance migration have been described. In the 70s, silicone bags gained popularity. Considering the risk of bag damage due to aging degradation, cohesive silicone bags have been used for breast reconstruction and breast augmentation since 2000, thereby preventing content escape even when the bag is damaged. During the SBI surgery in this patient, cohesive silicone bags were commonly used. However, detailed information on the SBI characteristics not available.
Anti-MDA5 antibody is specifically in CADM, and MDA5 recognizes double-stranded RNA derived from virus at viruses during infection, inducing an innate immune response [4]. There is currently no solid evidence indicating that the expression of anti-MDA5 antibody is a result of adjuvant substances such as silicon. Therefore, confirming a potential association between the MDA5 antibody-positive DM and SBI is difficult because it could simply be a coincidence. Recently, it has become possible in Japan to measure anti-MDA5 antibodies through commercial means with insurance coverage (since 2016). With the exception of one case [2], previous cases have not undergone such measurements. Our case could be the first report of anti-MDA5 antibody-positive DM after SBI. Although we were able to start treatment prior to rapidly progressive changes of lung lesions in our case, anti-MDA5 antibody-positive CADM is associated with a high incidence of rapidly progressive interstitial pneumonia and has a poor prognosis [5]. Consequently, with the increasing number of cosmetic SBI surgeries, it is imperative to monitor the development of anti-MDA5 antibody-positive DM following SBI surgeries.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was not required for the studies involving humans because This is a case report and not a clinical study. Informed consent was obtained from the referred patients. The studies were conducted in accordance with the local legislation and institutional requirements. The human samples used in this study were acquired from a by-product of routine care or industry. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontierspartnerships.org/articles/10.3389/jcia.2024.13129/full#supplementary-material
References
1. Kumagai, Y, Shiokawa, Y, Medsger, TA, and Rodnan, GP. Clinical spectrum of connective tissue disease after cosmetic surgery. Observations on eighteen patients and a review of the Japanese literature. Arthritis Rheum (1984) 27:1–12. doi:10.1002/art.1780270101
2. Imanaka, Y, Nakagawa, Y, Yamaoka, T, Kotobuki, Y, Hayashi, M, Katayama, I, et al. Refractory dermatomyositis which developed in a patient with silicone breast implants. Allergol Int (2022) 71:158–60. doi:10.1016/j.alit.2021.07.008
3. Meyer, DR, Bui, HX, Carlson, JA, Ratliff, CD, Guevarra, MC, DelRosario, AD, et al. Silicon granulomas and dermatomyositis-like changes associated with chronic eyelid edema after silicone breast implant. Ophthalmic Plast Reconstr Surg (1998) 14:182–8. doi:10.1097/00002341-199805000-00007
4. Funabiki, M, Kato, H, Miyachi, Y, Toki, H, Motegi, H, Inoue, M, et al. Autoimmune disorders associated with gain of function of the intracellular sensor MDA5. Immunity (2014) 40:199–212. doi:10.1016/j.immuni.2013.12.014
Keywords: autoimmune/inflammatory syndrome induced by adjuvants, anti-melanoma differentiation-associated gene 5, silicone breast implants, rapidly progressive interstitial pneumonia, dermatomyositis
Citation: Okubo R, Hayashi S, Tokoro S and Igawa K (2024) Anti-melanoma differentiation-associated gene 5 antibody-positive clinically amyopathic dermatomyositis in a patient with silicone breast implants. J. Cutan. Immunol. Allergy 7:13129. doi: 10.3389/jcia.2024.13129
Received: 14 April 2024; Accepted: 17 May 2024;
Published: 28 May 2024.
Copyright © 2024 Okubo, Hayashi, Tokoro and Igawa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shujiro Hayashi, c2hheWFzaGlAZG9ra3lvbWVkLmFjLmpw
†ORCID: Shujiro Hayashi, orcid.org/0000-0001-6558-4818
 Reimi Okubo
Reimi Okubo