- 1Department of Renal Medicine, Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom
- 2Leeds Institute of Health Sciences, Faculty of Medicine and Health, University of Leeds, Leeds, United Kingdom
- 3Division of Psychological and Social Medicine, Leeds Institute of Health Sciences, University of Leeds, Leeds, United Kingdom
- 4Department of Renal Medicine, Bradford Teaching Hospitals NHS Foundation Trust, Bradford, United Kingdom
- 5Leeds Institute of Medical Research, Faculty of Medicine and Health, University of Leeds, Leeds, United Kingdom
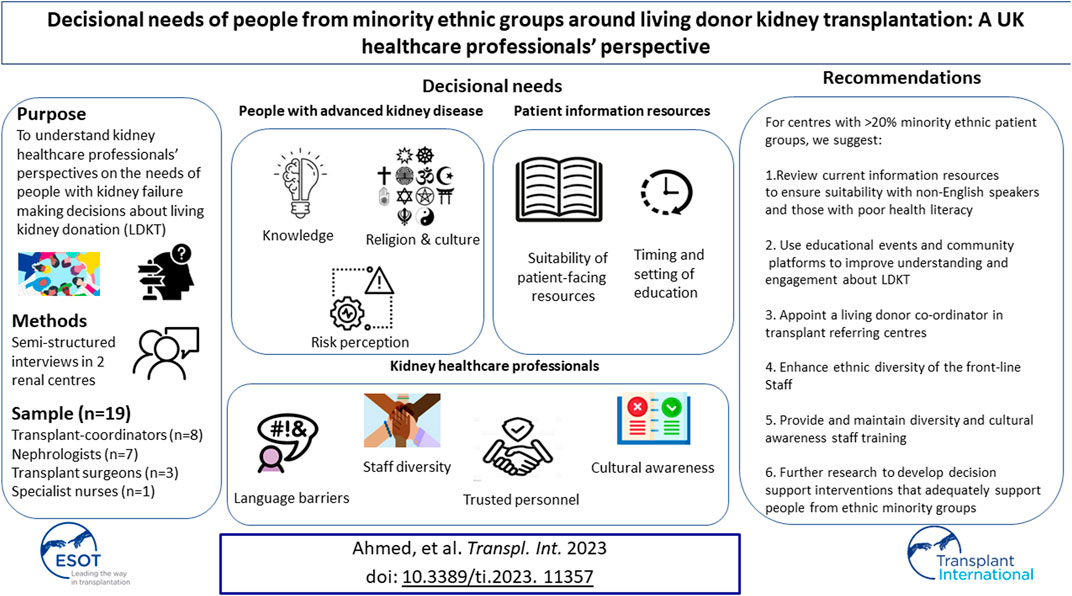
Despite improved patient and clinical outcomes, living donor kidney transplantation is underutilized in the United Kingdom, particularly among minority ethnic groups, compared to deceased donor kidney transplantation. This may in part be due to the way in which kidney services present information about treatment options. With a focus on ethnicity, semi structured interviews captured the views of 19 kidney healthcare professionals from two renal centres in West Yorkshire, about the decisional needs and context within which people with advanced kidney disease make transplant decisions. Data were analysed using thematic analysis. Themes were categorized into three groups: 1) Kidney healthcare professionals: language, cultural awareness, trusted personnel, and staff diversity, 2) Patient information resources: timing and setting of education and suitability of patient-facing information and, 3) People with advanced kidney disease: knowledge, risk perception, and cultural/religious beliefs. To our knowledge, this is the first study in the United Kingdom to investigate in depth, healthcare professionals’ views on living donor kidney transplantation decision making. Six recommendations for service improvement/delivery to support decision making around living donor kidney transplantation among minority ethnic groups are described.
Introduction
Living donor kidney transplantation (LDKT) has superior patient and clinical outcomes for people with advanced kidney disease (AKD), including better quality of life, survival, graft success compared to deceased donor transplantation, and is more cost effective than dialysis [1, 2]. Despite this, few people with kidney disease receive a live donor transplant compared to other renal replacement options; [3], and ethnic and socio-demographic differences in the uptake of LDKT are reported; [4]. AKD is up to five times more common among minority ethnic groups due to a higher prevalence of long term conditions such as diabetes mellitus and hypertension [5, 6]. In the United Kingdom (UK), 27% of people on renal replacement therapy (RRT) are from minority ethnic groups [6]. More than half of transplant centres in the UK have >20% of their waiting list from people from ethnic minority groups with a third of these centres with >20% people from South Asian heritage [6, 9]. Yet the ethnic diversity of living kidney donors in United Kingdom (UK) has remained the same between 2006 and 2017 [7]. South Asians, the second largest ethnic group in the UK [8], receive only 17% of live donor kidney transplants compared to 33% for White and 11% for Black ethnic groups [9]. The disproportionately low number of organ donors from these groups results in longer waiting times for a deceased donor, and worse outcomes because of longer periods of dependence on dialysis treatments [10, 11].
National frameworks recommend timely preparation of people with AKD for renal replacement therapy (RRT), options including LDKT. This includes offering balanced, accurate information about all forms of RRT and how they may impact on people’s lives [12]. However, these guidelines do not address how variations in practice might impact on treatment uptake rates (by ethnicity), nor do they identify which interventions are most effective in helping to prepare people to make treatment decisions [13–15]. Several challenges exist for kidney services providing decision support as outlined below:
1) People making decisions about LDKT are presented with multiple treatment decisions often considered simultaneously, i.e., dialysis modality decisions, alongside decisions about deceased donor and living kidney donor transplantation. Each treatment has multiple different options, attributes, and consequences [16, 17]. Some patient information and patient decision aids present these treatment options equally, despite LDKT having optimal patient and clinical outcomes and the potential to forgo the need of dialysis with pre-emptive transplantation [18]. It is unknown how transplantation options should be described in patient information to accurately reflect how services present these to individuals with AKD [13]. Significant systemic changes and new ways of thinking are required to increase the uptake LDKT and furthermore to achieve it prior to the need for dialysis treatments [19].
2) Patient leaflets are most used to support face to face discussions within consultations. Quality assessments of this information suggests that it is presented in a way that is difficult to understand, does not signpost to cultural/religious relevant information and focusses more on preparation for surgery and treatment and/or service information that is not relevant to decision making [20–22].
3) People with AKD seeking LDKT take an active role in seeking and approaching potential donors. To do so, they must have knowledge about the transplantation process. This may be particularly challenging for people from ethnic minorities, as health literacy rates, i.e., people’s ability to read, understand and act upon health information, are often low [23, 24]. This may in part explain why some people prefer to adopt a “watch and wait” approach in the hope of being called up for a deceased kidney donor transplantation [25, 26]. Designing interventions to support people with low health literacy may improve people’s understanding and decision making [27].
To date, decision support interventions for people making LDKT decisions have been developed in non-UK settings and address various aspects of the decision making process, including interventions targeting recipient [28–30] or donor education [31, 32], decision coaching [33], and decision aids for healthcare providers [34]. In the UK, whilst various groups have started to explore decisional needs for LDKT, these studies have lacked diversity in terms of ethnicity and inclusion of non-English language speakers [35, 36]. Our team are undertaking research studies to develop an understanding of the decision needs for LDKT decision making in a diverse population including non-English speakers and minority ethnic groups, particularly South Asians [37]. This exploratory research aims to understand the decisional needs of people from minority ethnic groups in relation to LDKT from the perspective of kidney healthcare professionals (HCPs). This will increase our understanding about the type(s) of interventions that can enhance LDKT decision making.
Methods and Materials
Design
This study employs a qualitative methodology using semi-structured interviews with kidney HCPs. Research governance approvals via the Health Research Authority and NHS Research Ethics committee were granted in June 2020 (Reference: 21/NW/0095).
Setting
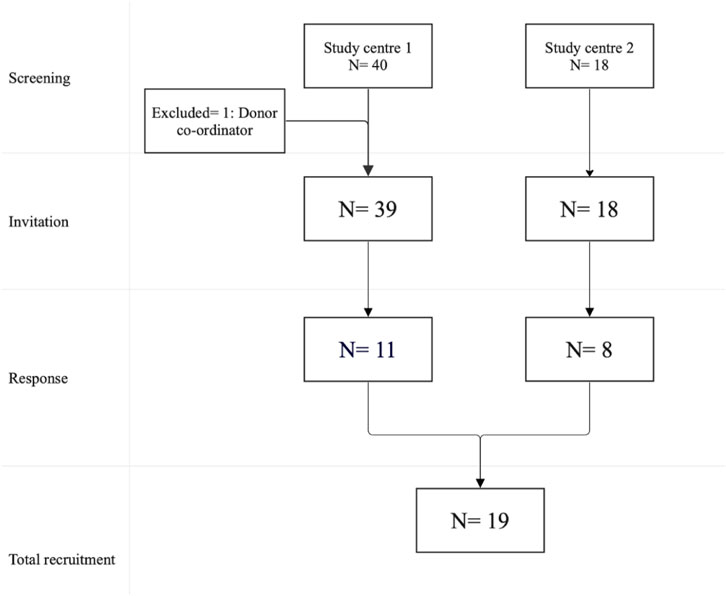
The study was conducted at Leeds and Bradford renal units in West Yorkshire, UK. The Leeds Renal Unit is the regional transplanting centre and oversees the care of 1,200 kidney transplant recipients and 450 living donors, with around 200 transplants performed annually. The Bradford Renal Unit is a transplant referral centre and provides care for 430 kidney transplant recipients and approximately 50 living donors. There are 150 patients active on the national transplant waiting list for Leeds and Bradford centres, combined. Around 40% and 18% of people with AKD on RRT in Bradford and Leeds respectively are from minority ethnic groups [3].
Sample
Non-probability sampling was employed [38]. Participants were eligible to take part if they met the following inclusion criteria: Kidney HCPs directly involved in assisting people with AKD in making LDKT decisions. The following groups were not eligible to participate: Kidney HCP with no direct involvement in transplantation, those who support living-donors or paediatric patients and colleagues (authors) directly involved in conduct of this research.
Recruitment
Eligible participants were contacted via NHS email. Figure 1 describes the recruitment process in the study centres.
Study Materials
An interview guide was developed using published literature on people decision making about LDKT and guided by the expertise of the research team and relevant stakeholders from each renal centre. The interview guide contained three parts: 1) Introduction: Briefing, demographics and describing clinical context 2) Exploration of views: HCP perspectives on patient’s decisional needs and patient information resources supporting LDKT decision making 3) close: opportunity to add any additional comments. For further information see Supplementary Material.
Data Collection
Semi-structured interviews were conducted virtually via Microsoft Teams (version 4.2.4.0) by researcher (AA) and took an average of 41 min (range 27–63 min). Participants were given the opportunity to ask questions about the study and provided their written consent to take part, before the interview. Data were transcribed using Otter software (Otter.ai, Indigo, 2.2.22/26 June 2020). Interviews were conducted until saturation of themes [39].
Data Analysis
Interviews were analysed using thematic analysis [40]. NVivo software (QSR International, release 1.7.1) was used to manage the data.
Results
The characteristics of the participants (P) are described in Table 1.
Themes are categorised under three broad headings: a) Kidney HCPs, b) patient information resources c) people with AKD.
Kidney HCPs
Language Barriers
HCPs believed that communication with non-English speaking patients could be difficult.
“We have language deficits; I think that's a massive issue. Clearly, we have a major second language probably Urdu /Hindi variant” P 3, F, Transplant co-ordinator
In these instances, hospital interpreters and family members were used to support discussions, and HCPs preferred hospital interpreters because of their familiarity with medical terminology. However, hospital interpreters were also felt to be time consuming, and less likely to provide accurate and complete translations.
“I think it's difficult to get information across, however good the translator is, and when some time is spent in translation, it means that maybe you haven't got the time to focus on those other important things, like live donation” P 11, M, Transplant surgeon
Cultural Awareness, Trusted Personnel and Staff Diversity
HCP highlighted several ways in which services could improve the delivery of information to people from ethnic minority groups who are making LDKT decisions. These included, improving the ethnic diversity of front-line staff, trusted personnel to improve communication, engagement with the kidney services and overcoming cultural barriers in LDKT decision making.
“I'd be very honest to say that all the transplant coordinators are from white ethnicity. Having someone from same community who has a real understanding of the issues that affect donation in that community, would be useful” P 6, M, Consultant nephrologist
“Let's put the effort in, before we approach patients, to get them to engage we need to know how living donation sits within their culture” P, 14, Female, Specialist nurse
A lack of trust was thought to relate to peoples’ prior experiences with health services, as well as more generalised concerns about how people of different ethnic groups are treated by the NHS. Furthermore, participants highlighted the need for training about gender-related cultural issues, and different religious viewpoints. One participant cited the importance of their cultural improvement officer for enhancing rapport and patient engagement.
“There may be some sort of distrust if they've kind of not grown up necessarily in this country. And I think it's very important when we meet with those patients to address some of those issues, or find out why people aren't coming forward” P 1, F, Transplant co-ordinator
“I think there are worries, you know, certainly at the moment, in terms of how people with different ethnicities that are treated in different areas of the NHS, you must know about the high maternity deaths among Black ethnic groups” P 4, F, Transplant co-ordinator
Patient Information Resources
Timing of Education
HCPs suggested that information and education designed to prepare people for making decisions about renal replacement therapies should be provided at an earlier stage of the kidney disease pathway. They recognised that people with AKD are often asked to consider different treatment options, e.g., dialysis and transplantation at the same time, and that it would be beneficial to have more time to consider the options.
“When they are in low clearance clinic, they are already symptomatic, you are asking them what option do you want? dialysis? what sort of dialysis? Ok let me tell you about transplant. But you need to make a decision about dialysis as well. You need access. Do you have a live donor? too much and need to be spaced” P 2, F, Consultant nephrologist
Setting of Education
HCPs saw value in providing group education sessions to help people make treatment decisions and dispel misconceptions about transplantation, rather than in one-to-one consultations with nephrologists and transplant co-ordinators. They proposed a variety of settings such as the renal unit, primary care and community and faith-based community settings.
“I have attended community events where we talked about and promoted transplantation and donation, people feel more comfortable sometimes [to go] somewhere [where] they are used to [going] and [engaging] in different discussions” P 1, F, Transplant co-ordinator
Suitability of Patient Facing Information
HCP use information leaflets to supplement their discussions with patients. They valued these resources’ ability to provide people with AKD with basic treatment information. However, they believed that this generic information might not be appropriate for non-English speakers and those with lower levels of health literacy. Apart from one booklet in Urdu, HCPs reported that the current written resources are all in English. It was suggested that resources should be translated into regional languages, particularly for people from South Asia, as this ethnicity makes up a significant proportion of their local population.
“I think in somewhere like [Study centre 2] where there's a large Asian population, it will be a great help for this literature and booklets to be available in the local language, predominantly local language” P 15, M, Consultant nephrologist
Additionally, HCPs had concerns about the readability of the patient facing materials they use to supplement their LDKT discussions.
“Potentially, some patients may find them difficult to understand, their language sometimes can be a little bit complex for some people, they need to be simplified to suit more people” P 19, F, transplant co-ordinator
HCPs felt that patient-facing materials should include clarification of common misconceptions about the transplantation process, and information related to different cultures and religions in relation to transplantation.
“We are all concerned about live donation in South Asians and Muslims, but those books don’t really [talk] about live donation in Islam. Or how helping someone else sits with that culture” P 14, F, Specialist nurse
“Sometimes little things can make big difference, for example displaying a cartoon picture of a Sikh person with a turban can make people more trusting and willing to know more about treatments like this” P, 14, Female, Specialist nurse.
Furthermore, HCPs thought that it was valuable for people with AKD to talk to other people in a similar situation to share their experiences
“Sometimes people find it easier if they see the story of someone who had the same journey” P 4, F, Transplant co-ordinator
People With Advanced Kidney Disease
Knowledge About LDKT
HCPs believed that people with AKD do not have enough knowledge about the advantages and disadvantages of LDKT, alternative treatment options, the transplantation process, donor-work up and donation suitability, to make an informed decision. They believed that knowledge gaps are more prevalent among people with low levels of health literacy particularly those with low education, low socioeconomic status and the non-English speakers.
“You know, we have many of the non-English speaking patients around this region, also some have low education and bad social circumstances. They are low in literacy, they may not have the required knowledge, they even sometimes have wrong knowledge about live donation” P 3, F, Transplant co-ordinator
Risk Perception
Healthcare professionals felt that this lack of knowledge about transplantation could lead to concerns about the short- and long-term consequences of transplantation, the physical risk of an operation and the financial implications of donation.
“Because of what they have been through with kidney disease, some people have genuine concerns about how someone could have a healthy life with one kidney, those are the ones who won’t ask their family even if that means they stay on dialysis forever if they don’t get a kidney from the list” P 7, M, Consultant nephrologist
“They do often worry and ask how long till their donors are able to work? What about their job, etc. And specially when it's a donor coming from abroad, they worry about airfare and loss of earnings” P 12, M, Consultant nephrologist
Cultural and Religious Beliefs
Healthcare professionals identified instances where they felt that cultural and religious beliefs impacted on decision making. For example, Muslims were thought to require greater clarification about their religion stance on donation.
“Islam in the Great Britain is not a homogenous entity. So, communities are very dependent on what their own Imam thinks. Certainly, some Imams don't take the same lead as the Muslim Council of Great Britain. So, I suppose there are a lot of different perceptions about living donation” P 6, M, Consultant nephrologist
Healthcare professionals also suggested that in their experience, people from ethnic minorities were less likely to trust the health service, and people from South Asia were more private and less willing to discuss their health and had concerns about others perception of a woman’s suitability for marriage after donation.
“So sometimes we have kind of media campaigns, Our South Asian patients will not consider this, obviously, not a lot of people like that, but they like to keep more private” P 4, F, Transplant co-ordinator
“It tends to be older women from the Asian community who end up donating, they worry if a young girl donated a kidney, she's somehow seen as less suitable when it comes to marriage” P 15, M, Consultant nephrologist
Discussion
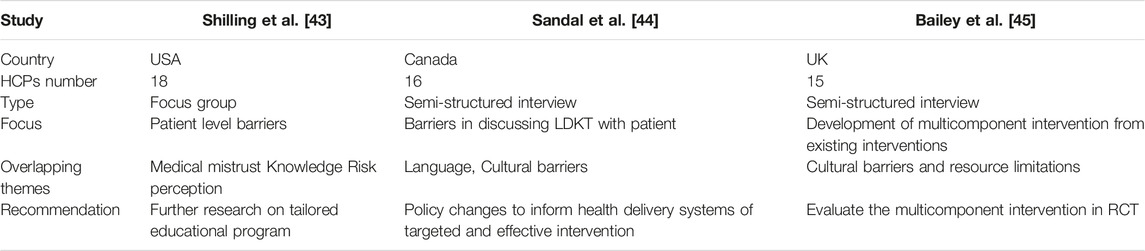
This study identifies themes that HCPs believed were important in supporting people to make decisions about LDKT. Some of the themes pertain to the individual characteristics of people with AKD, such as knowledge, religion, and culture, whereas others, such as the way in which education about LDKT is delivered (including timing and setting), are linked to the range and availability of resources that may assist them in making transplant decisions. While some themes are thought to be shared by all ethnic groups, others such as knowledge gaps were thought to be more prevalent among non-English speakers and those with lower socioeconomic status. The multitude of these attributes within minority ethnic groups add another layer of complexity when considering tailored interventions to improve LDKT uptake [60]. Understanding how to support people with AKD who need to make treatment decisions requires an appreciation of the different goals, values, knowledge, skills and motivation of the key stakeholders who support the decision making process, including families/carers and HCPs [41, 42]. There are few qualitative studies assessing the perspective of HCPs each with a difference focus, including African American populations patient level [43], communication barriers [44], and interventions to improve access to LDKT using existing models [45] (Table 2). To our knowledge, we have conducted the first UK based study that explores the views of HCPs about the decisional needs of minority ethnic groups around LDKT, with a view to developing a culturally sensitive decision support intervention.
Consistent with other studies, we found that religious and cultural beliefs and trust are consistently reported as major barriers to people pursuing LDKT, particularly in minority ethnic groups [46, 47, 61]. Information should signpost to religious and cultural information relevant to transplantation that is available in patient-facing resources [20] and within community outreach and informal promotions. The latter associates with a higher number of people pursuing LDKT [44]. In the UK, community- and faith-based platforms have been used to address cultural and religious barriers to LDKT [48]. These outreach interventions have increased awareness and interest in LDKT however there has been only a limited effect on uptake rates [49].
Furthermore, our study participants highlighted the need for diversity training to improve cultural and religious awareness of factors that might impact on people’s willingness to pursue transplantation. Similar conclusions were made in a Dutch study that examined HCPs engagement with culturally diverse populations [61]. Providing regular training should improve skills and confidence over time, rather than reinforce stereotypes and leave staff feeling overcautious and uncertain and in their ability to communicate with people from ethnic minorities [50, 51]. A regular programme of staff training also is important to maintain quality of education [62]. Moreover, as recommended in the National Health Service (NHS) people plan [53], employing ethnically diverse front-line staff who are more representative of the local population can support people with AKD by improving engagement and trust in medical services [52].
Written patient information is commonly used by HCPs to supplement discussions and support shared decision-making [20]. There is considerable variation in its quality [20, 21] and HCPs in our study expressed the view that this information is not suitable for non-English speakers and people with low health literacy, who are often from minority ethnic groups [21]. Signposting people to resources produced in alternative and multi-lingual formats, use of interpreters or bilingual staff may address these language and health literacy needs [54, 61]. Such tailored resources (culturally sensitive written information and videos) have only recently been developed by community organisations working with patient groups and HCPs, including the sharing of experiences of other people with AKD who have previously made a decision about LDKT into educational sessions. The need to implement the use of these resources was advocated by participants in this study. This has already been recognised nationally with inclusion of resources in the NHS Blood and Transplant “Transplant TV” series [55], the National Black, Asian and minority ethnic (BAME) Transplant Alliance initiative [63], and other projects that support LDKT decision making [56, 57]. Recent guidance on the inclusion of narratives in patient decision aids interventions, suggest that whilst they may be beneficial to help people understand others experiences of the process with which a decision was made, they may also bias people’s decision making [58].
The timing and setting of patient education about LDKT is another important aspect of decision making. There is a wide variation in practice between renal units within the UK, with many large non-transplanting centres undertaking the work-up and evaluation of potential living kidney donors locally rather than referring them to the transplanting centre. Delays at various stages of the living donor pathway contribute to lower LDKT rates in non-transplanting renal centres, and the presence of Living Donor Coordinators (LDCs) in these centres would facilitate more timely decision making. National Health Service Blood and Transplant (NHSBT) and the UK Living Kidney Donor Network have developed a LDC workforce calculator to support the commissioning of LDCs [63] but implementation remains a challenge. In addition, a NHSBT-led UK transplant workforce survey of staff in transplanting and non-transplanting UK centres is in progress and this may help to identify unwarranted variation in staffing resource between centres.
This study recruited a range of kidney health professionals working within two large inner city kidney units; however, the findings may be limited in their generalisability to other UK kidney units as the diversity of these units may represent a proportion of the population with different needs to that as a whole. It is promising however that a national workshop involving multi-centre HCPs at the 2022 UK Living Kidney Donor Network meeting identified the same top three resource-related barriers to LDKT (cultural issues, language, and health literacy) [59].
Based on the study findings we recommend the following measures to improve LDKT decision making for people from diverse ethnic groups in units where minority ethnic groups represent >20% of the deceased donor waiting list:
1. Review current patient information resources to ensure their suitability for people particularly with low health literacy and non-English speakers, including signposting to culturally tailored information involving those communities that are most disadvantaged [20, 55, 63].
2. Explore ways in which the experience of other people with AKD can be used in educational events and platforms [55–57] to improve understanding and health literacy without biasing people’s decision making [58].
3. Appoint living donor co-ordinators in transplant referral centres as per national guidance and supported by the NHSBT LDC workforce calculator [63]. This will facilitate a dedicated and proactive LDC role within all renal centres and therefore reduce unwarranted variation in practice.
4. Enhance the ethnic diversity of the frontline staff such as transplant coordinators by affirmative recruitment, for better engagement of ethnic minority groups with kidney services and to improve the quality of decision support.
5. Develop and maintain a regular programme of diversity and cultural awareness staff training that addresses all of the issues pertinent to transplantation and organ donation.
6. Further research and review of the current evidence base to develop tailored decision support interventions that adequately support people from ethnic minority groups.
Data Availability Statement
The datasets presented in this article are not readily available because informed consent included data collection solely for this study purpose. Requests to access the datasets should be directed to AA, YWhtZWQuYWhtZWQzMEBuaHMubmV0.
Ethics Statement
The studies involving human participants were reviewed and approved by Health Research Authority and NHS Research Ethics Committee (Ref 21/NW/0095). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AA: Design, recruitment, data collection, analysis, writing and editing. AW: design, writing and critical review. SA: design, writing and critical review. JS: Design, recruitment, writing and critical review. SD: Design, recruitment, writing and critical review. All authors contributed to the article and approved the submitted version.
Funding
We acknowledge Kidney research Yorkshire (Ref: 19-127) which helped initiate this research and Leeds Hospitals Charity (Ref: A2001851) for funding the project.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontierspartnerships.org/articles/10.3389/ti.2023.11357/full#supplementary-material
References
1. Terasaki, PI, Cecka, JM, Gjertson, DW, and Takemoto, S. High Survival Rates of Kidney Transplants From Spousal and Living Unrelated Donors. N Engl J Med (1995) 333(6):333–6. doi:10.1056/NEJM199508103330601
2. Laupacis, A, Keown, P, Pus, N, Krueger, H, Ferguson, B, Wong, C, et al. A Study of the Quality of Life and Cost-Utility of Renal Transplantation. Kidney Int (1996) 50(1):235–42. doi:10.1038/ki.1996.307
3.National Health Service. Blood and Transplant Organ Donation and Transplantation Annual Activity Report 2021-2022 (2022). Available at: https://www.organdonation.nhs.uk/helping-you-to-decide/about-organ-donation/statistics-about-organ-donation/transplant-activity-report/ (Accessed January, 2023).
4. Wu, , , Robb, ML, Watson, CJE, Forsythe, JLR, Tomson, CRV, Cairns, J, et al. Barriers to Living Donor Kidney Transplantation in the United Kingdom: A National Observational Study. Nephrol Dial Transplant (2017) 32(5):890–900. doi:10.1093/ndt/gfx036
5. Goff, E Ethnicity and Type 2 Diabetes in the UK. Bet Med (2019) 36(8):927–38. doi:10.1111/dme.13895
6.UK Renal Registry. UK Renal Registry 24th Annual Report – Data to 31/12/2020 (2022). Available at: https://ukkidney.org/audit-research/annual-report (Accessed July, 2022).
7. Bailey, PK, Wong, K, Robb, M, Burnapp, L, Rogers, A, Courtney, A, et al. Has the UK Living Kidney Donor Population Changed Over Time? A Cross-Sectional Descriptive Analysis of the UK Living Donor Registry Between 2006 and 2017. BMJ Open (2020) 10(6):e033906. doi:10.1136/bmjopen-2019-033906
8.UK census. UK Census (2021), Available at: https://census.gov.uk/census-2021-results (Accessed October, 2022).
9.National Health Service. Blood and Transplant Organ Donation and Transplantation Annual Report on Ethnic Differences (2022). Available at: https://www.odt.nhs.uk/statistics-and-reports/annual-report-on-ethnicity-differences/ (Accessed January, 2023).
10. Foley, RN, Parfrey, PS, Harnett, JD, Kent, GM, Martin, CJ, Murray, DC, et al. Clinical and Echocardiographic Disease in Patients Starting End-Stage Renal Disease Therapy. Kidney Int (1995) 47:186–92. doi:10.1038/ki.1995.22
11. Cheung, A, Sarnak, MJ, Yan, G, Berkoben, M, Heyka, R, Kaufman, A, et al. Cardiac Diseases in Maintenance Hemodialysis Patients: Results of the HEMO Study. Kidney Int (2004) 65:2380–9. doi:10.1111/j.1523-1755.2004.00657.x
12.National Institute for Health and Care Excellence (NICE). Guidance on Renal Replacement Therapy and Conservative Management (NICE Guideline NG107, 03.October.2018) (2018). Available at: https://www.nice.org.uk/guidance/ng107/chapter/recommendations (Accessed January, 2023).
13. Bekker, HL, Winterbottom, A, Gavaruzzi, T, Finderup, J, and Mooney, . Decision Aids to Assist Patients in Choosing the Right Treatment for Kidney Failure. Clin Kidney J – Spec Edition (2023) 23:236. doi:10.1186/s12882-022-02853-0
14. Van Biesen, W, van der Veer, SN, Murphey, M, and Loblova, O. Patients' Perceptions of Information and Education for Renal Replacement Therapy: An Independent Survey by the European Kidney Patients' Federation on Information and Support on Renal Replacement Therapy. PLoS ONE (2014) 9:e103914. doi:10.1371/journal.pone.0103914
15. Combes, G, Sein, K, and Allen, K. How Does Pre-Dialysis Education Need to Change? Findings From a Qualitative Study With Staff and Patients. BMC Nephrol (2017) 18:334. doi:10.1186/s12882-017-0751-y
16. Bekker, HL, Winterbottom, A, Gavaruzzi, T, Mooney, A, Wilkie, M, Davies, S, et al. The Dialysis Decision Aid Booklet: Making the Right Choices for You. United Kingdom: Kidney Research UK (2015). Available at: https://kidneyresearchuk.org/wp-content/uploads/2019/05/KR-decision-Aid-DOWNLOAD.pdf (Accessed October, 2022).
17. Winterbottom, A, Bekker, HL, Russon, L, Hipkiss, V, Ziegler, L, Williams, R, et al. Dialysis vs Conservative Management Decision Aid: A Study Protocol. J Kidney Care (2018) 3:179–85. doi:10.12968/jokc.2018.3.3.179
18. Winterbottom, A, Mooney, A, Russon, L, Hipkiss, V, Ziegler, L, Williams, R, et al. Kidney Disease Pathways, Options and Decisions: An Environmental Scan of International Patient Decision Aids. Nephrol Dial Transplant (2020) 35(12):2072–82. doi:10.1093/ndt/gfaa102
19. Isaac, K, Maggiore, U, Knight, SR, Rana Magar, R, Pengel, LHM, and Dor, FJMF Pre-Emptive Living Donor Kidney Transplantation: A Public Health Justification to Change the Default. Front Sec Health Econ (2023) 11. doi:10.3389/fpubh.2023.1124453
20. Winterbottom, A, Conner, M, Mooney, A, and Bekker, HL. Evaluating the Quality of Patient Leaflets About Renal Replacement Therapy Across UK Renal Units. Nephrol Dial Transplant (2007) 22(8):2291–6. doi:10.1093/ndt/gfm095
21. Winterbottom, A, Stoves, J, Ahmed, S, Ahmed, A, and Daga, S. Patient Information About Living Donor Kidney Transplantation Across UK Renal Units: A Critical Review. J Ren Care (2021) 49(1):45–55. doi:10.1111/jorc.12404
22. Winterbottom, A, Mooney, A, Russon, L, Hipkiss, V, Williams, R, Ziegler, L, et al. Critical Review of Leaflets About Conservative Management Used in UK Renal Services. J Ren Care (2020) 46(1):250–7. doi:10.1111/jorc.12327
23. Liu, C, Wang, D, Liu, C, Jiang, J, Wang, X, Chen, H, et al. What Is the Meaning of Health Literacy? A Systematic Review and Qualitative Synthesis. Community Health(2020) 8(2):e000351. doi:10.1136/fmch-2020-000351
24. Fransen, MP, Harris, VC, and Essink-Bot, ML. Low Health Literacy in Ethnic Minority Patients: Understandable Language Is the Beginning of Good Healthcare. Ned Tijdschr Geneeskd (2013) 157(14):A5581.
25. Kranenburg, LW, Zuidema, WC, Weimar, W, Hilhorst, MT, Ijzermans, JNM, Passchier, J, et al. Psychological Barriers for Living Kidney Donation: How to Inform the Potential Donors? Plantation (2007) 84(8):965–71. doi:10.1097/01.tp.0000284981.83557.dc
26. Rodrigue, JR, Cornell, DL, Kaplan, B, and Howard, RJ. Patients' Willingness to Talk to Others About Living Kidney Donation. Transplant (2008) 18(1):25–31. doi:10.1177/152692480801800107
27. Boonstra, MD, Reijneveld, SA, Foitzik, EM, Westerhuis, R, Navis, G, and de Winter, AF. How to Tackle Health Literacy Problems in Chronic Kidney Disease Patients? A Systematic Review to Identify Promising Intervention Targets and Strategies. ant (2020) 36(7):1207–21. doi:10.1093/ndt/gfaa273
28. Patzer, RE, Basu, M, Larsen, CP, Pastan, SO, Mohan, S, Patzer, M, et al. iChoose Kidney: A Clinical Decision Aid for Kidney Transplantation Versus Dialysis Treatment. Transplantation (2016) 100(3):630–9. doi:10.1097/TP.0000000000001019
29. Waterman, AD, Robbins, ML, Paiva, AL, Peipert, JD, Kynard-Amerson, CS, Goalby, CJ, et al. Your Path to Transplant: A Randomized Controlled Trial of a Tailored Computer Education Intervention to Increase Living Donor Kidney Transplant. BMC Nephrol (2014) 15(1):166. doi:10.1186/1471-2369-15-166
30. Axelrod, DA, Kynard-Amerson, CS, Wojciechowski, D, Jacobs, M, Lentine, KL, Schnitzler, M, et al. Cultural Competency of a Mobile, Customized Patient Education Tool for Improving Potential Kidney Transplant Recipients' Knowledge and Decision-Making. Clin Transplant (2017) 31(5):e12944. doi:10.1111/ctr.12944
31. Garonzik-Wang, JM, Berger, JC, Ros, RL, Kucirka, LM, Deshpande, NA, Boyarsky, BJ, et al. Live Donor Champion: Finding Live Kidney Donors by Separating the Advocate From the Patient. Transplantation (2012) 93(11):1147–50. doi:10.1097/TP.0b013e31824e75a5
32. Waterman, AD, McSorley, AMM, Peipert, JD, Goalby, CJ, Peace, LJ, Lutz, PA, et al. Explore Transplant at Home: A Randomized Control Trial of an Educational Intervention to Increase Transplant Knowledge for Black and White Socioeconomically Disadvantaged Dialysis Patients. BMC Nephrol (2015) 16(1):150. doi:10.1186/s12882-015-0143-0
33. Foundation, NK. The Big Ask, the Big Give (2016). Available at: www.kidney.org/livingdonation (Accessed August 04, 2016).
34. Gupta, A, Chen, G, and Kaplan, B. KDPI and Donor Selection. Am J Transplant (2014) 14(11):2444–5. doi:10.1111/ajt.12930
35. Wong, K, Owen-Smith, A, Caskey, F, MacNeill, S, Tomson, CRV, Dor, FJMF, et al. Investigating Ethnic Disparity in Living-Donor Kidney Transplantation in the UK: Patient-Identified Reasons for Non-Donation Among Family Members. J Clin Med (2020) 9(11):3751. doi:10.3390/jcm9113751
36. Bailey, P, Ben-Shlomo, Y, Caskey, FJ, Al-Talib, M, Lyons, H, Babu, A, et al. Development of an Intervention to Improve Access to Living-Donor Kidney Transplantation (The ASK Study). PLoS One (2021) 16(6):e0253667. doi:10.1371/journal.pone.0253667
37. Ahmed, A, Winterbottom, A, Stoves, J, Ahmed, S, and Daga, S. Facilitators and Barriers to Living Donor Kidney Transplantation. J Kidney Care (2022) 6(6):276–84. doi:10.12968/jokc.2021.6.6.276
38. Schreuder, HT, Gregoire, TG, and Weyer, JP. For What Applications Can Probability and Non-Probability Sampling Be Used? Environ Monit Assess (2001) 66:281–91. doi:10.1023/A:1006316418865
39. Legard, R, Keegan, J, and Ward, K. In-depth Interviews. In: J Ritchie, and J Lewis, editors. Qualitative Research Practice: A Guide for Social Science Students and Researchers. London: Sage (2003). p. 139–69.
40. Braun, V, and Clarke, V. Using Thematic Analysis in Psychology. Qual Res Psychol (2008) 3(2):77–101. doi:10.1191/1478088706qp063oa
41. Bekker, HL. Representation of Making Health Decisions Individually, and Together (MIND-IT) (V1). In: K Breckenridge, HL Bekker, SN van der Veer, E Gibbons, D Abbott, and FJ Caskey, editors. NDT Perspectives. Oxford: Oxford University Press (2019).
42. Bomhof-Roordink, H, Gartner, FR, Stiggelbout, AM, and Pieterse, AH. Key Components of Shared Decision Making Models: A Systematic Review. BMJ Open (2019) 9:e031763. doi:10.1136/bmjopen-2019-031763
43. Shilling, , , Norman, ML, Chavin, KD, Hildebrand, LG, Lunsford, SL, Martin, MS, et al. Healthcare Professionals' Perceptions of the Barriers to Living Donor Kidney Transplantation Among African Americans. J Natl Med Assoc (2006) 98(6):834–40.
44. Sandal, S, Charlebois, K, Fiore, JF, Wright, DK, Fortin, MC, Feldman, LS, et al. Health Professional-Identified Barriers to Living Donor Kidney Transplantation: A Qualitative Study. Can J Kidney Health Dis (2019) 6:2054358119828389. doi:10.1177/2054358119828389
45. Bailey, PK, Ben-Shlomo, Y, Caskey, FJ, Al-Talib, M, Lyons, H, Babu, A, et al. Development of an Intervention to Improve Access to Living-Donor Kidney Transplantation (The Ask Study). PLOS ONE (2021) 16(6):e0253667. doi:10.1371/journal.pone.0253667
46. Ahmed, A, Winterbottom, A, Stoves, J, Ahmed, S, and Daga, S. Factors Impacting Conversations With Friends and Family About Living Kidney Donation. The Physician (2021) 7(1):1–7. doi:10.38192/1.7.1.3
47.Religious Beliefs and Attitudes to Organ Donation. Religious Beliefs and Attitudes to Organ Donation (2019). Available at: https://www.gov.wales/sites/default/files/statistics-and-research/2019-07/150730-religious-beliefs-attitudes-organ-donation-summary-en.pdf (Accessed October, 2022).
48.NBTA. Living Transplant Initiative by National Health Service Blood and National Black, Asian and Minority Ethnicities Transplant Alliance Report (2019). Available at: https://www.nbta-uk.org.uk/living-transplant-initiative/ (Accessed October, 2022).
49.NBTA. Living Transplant Initiative by National Health Service Blood and National Black, Asian and Minority Ethnicities Transplant Alliance Report (2019). Available at: https://www.nbta-uk.org.uk/wp-content/uploads/2019/11/LTI-FINAL-REPORT-Nov-2019.pdf (Accessed October, 2022).
50. Bezrukova, K, Spell, CS, Perry, JL, and Jehn, KA. A Meta-Analytical Integration of Over 40 Years of Research on Diversity Training Evaluation. Psychol Bull(2016) 142(11):1227–74. doi:10.1037/bul0000067
51. Anand, R, and Winters, MF. A Retrospective View of Corporate Diversity Training From 1964 to the Present. Acad Manage Learn Educ (2008) 7:356–72. doi:10.5465/AMLE.2008.34251673
52. Akhtar, T, Hipkiss, V, and Stoves, J. Improving the Quality of Communication and Service Provision for Renal Patients of South Asian Origin: The Contribution of a Cultural and Health Improvement Officer. J Ren Care (2014) 40:41–6. doi:10.1111/jorc.12086
53.National Health Service. Improving Diversity in Recruitment Practices in the National Health Service (2021). Available at: https://www.nhsemployers.org/articles/improving-diversity-recruitment-practices-nhs (Accessed January, 2023).
54. Alsuliman, T, Alasadi, L, Mouki, A, and Alsaid, B. Language of Written Medical Educational Materials for Non-English Speaking Populations: An Evaluation of a Simplified Bi-Lingual Approach. BMC Med Educ (2019) 19(1):418. doi:10.1186/s12909-019-1846-x
55.Transplant TV. The Institute of Transplantation (2023). Available at: https://transplant.tv/themes/lets-talk-about/ (Accessed January, 2023).
56. David, L, Iraheta, YA, Ho, EW, Murillo, AL, Feinsinger, A, and Waterman, AD. Living Kidney Donation Stories and Advice Shared Through a Digital Storytelling Library: A Qualitative Thematic Analysis. Kidney Med (2022) 4:100486. doi:10.1016/j.xkme.2022.100486
57. Waterman, A, Wood, EH, Ranasinghe, ON, Faye Lipsey, A, Anderson, C, Balliet, W, et al. A Digital Library for Increasing Awareness About Living Donor Kidney Transplants: Formative Study. JMIR Form Res (2020) 4(7):e17441. doi:10.2196/17441
58. Winterbottom, A, Bekker, HL, Conner, M, and Mooney, A. Does Narrative Information Bias Individual's Decision Making? A Systematic Review. Oc Sci Med (2008) 67(12):2079–88. doi:10.1016/j.socscimed.2008.09.037
59.The Supporting Living Donor Workshop. Uk Living Kidney Donor Network Newsletter (2022). Available at: https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/26748/quarterly-uk-living-donor-network-newsletter-edition-may-22.pdf (Accessed January, 2023).
60. Khalil, K, Brotherton, A, Moore, S, Evison, F, Gallier, S, Hodson, J, et al. Interaction Between Socioeconomic Deprivation and Ethnicity for Likelihood of Receiving Living-Donor Kidney Transplantation. BMC Nephrol (2022) 23:113. doi:10.1186/s12882-022-02742-6
61. Ismail, SY, Claassens, L, Luchtenburg, AE, Roodnat, JI, Zuidema, WC, Weimar, W, et al. Living Donor Kidney Transplantation Among Ethnic Minorities in the Netherlands: A Model for Breaking the Hurdles. Patient Educ Couns (2013) 90:118–24. doi:10.1016/j.pec.2012.08.004
62. Redeker, S, Ismail, SY, Busschbach, JJ, Weimar, W, and Massey, E. National Implementation of the Kidney Team at Home Educational Intervention. Transplantation (2020) 104(S3):S291. doi:10.1097/01.tp.0000699960.37154.4d
63.Living Transplant Initiative. NBTA. Available from: https://www.nbta-uk.org.uk/living-transplant-initiative/ (Accessed January 2023).
Keywords: transplantation, living donor, advanced kidney disease, ethnic minorities, decision making
Citation: Ahmed A, Winterbottom A, Ahmed S, Stoves J and Daga S (2023) Decisional Needs of People From Minority Ethnic Groups Around Living Donor Kidney Transplantation: A UK Healthcare Professionals’ Perspective. Transpl Int 36:11357. doi: 10.3389/ti.2023.11357
Received: 13 March 2023; Accepted: 04 July 2023;
Published: 24 July 2023.
Copyright © 2023 Ahmed, Winterbottom, Ahmed, Stoves and Daga. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahmed Ahmed, YWhtZWQuYWhtZWQzMEBuaHMubmV0
 Ahmed Ahmed
Ahmed Ahmed Anna Winterbottom1,2
Anna Winterbottom1,2 Sunil Daga
Sunil Daga