Abstract
Oral disease is linked with systemic inflammation and various systemic conditions, including chronic liver disease. Liver transplantation (LT) candidates often need dental infection focus eradication, and after LT, there is high risk of many inflammation-related complications. We studied whether pre-LT dental status is associated with the occurrence of post-LT complications. This study included 225 adult LT recipients whose teeth were examined and treated before LT, and 40 adult LT recipients who did not have pre-LT dental data available. Data on post-LT complications were collected from the national liver transplant registry and followed up until the end of July 2020. Worse pre-LT dental status was associated with a higher risk of acute rejection post-LT compared to patients with good dental status. Worse dental status was also associated with higher 1-year-post-LT ALT levels and lower albumin levels. In conclusion, poor pre-LT oral health seems to associate with an increased risk of post-LT acute rejection and with elevated ALT levels and decreased albumin levels, suggesting an effect on post-LT liver health. Therefore, prevention and treatment of oral and dental diseases should be promoted early in the course of liver disease.
Graphical Abstract
Introduction
A relationship between poor oral health and liver disease has been presented previously. The systemic inflammation caused by oral infections seems to accelerate the progression of chronic liver disease (CLD) [1–3], and CLD, in turn, seems to affect oral diseases [4, 5]. Oral infection foci need to be eliminated before liver transplantation (LT) to avoid severe systemic complications [6]. A significant link between a lack of pre-LT dental treatment and post-LT systemic infections has been suggested in patients with acute liver failure (ALF) [7]. In a study by Göbel et al. [8], dental infection foci was associated with a higher risk of pre- and post-LT bacterial infections. After transplantation, patients use immunosuppressants for the rest of their lives. During the first year post-LT in particular, but also later, patients are prone to severe, even fatal, infections [9, 10].
The need for dental and periodontal treatment has proved to be high among LT recipients, and poor oral hygiene [4, 11, 12]. Compared to healthy controls, LT candidates are shown to have a higher prevalence of apical periodontitis and other oral diseases (i.e., dental caries, periodontal and oral mucosal diseases) [13, 14]. Furthermore, the presence of oral diseases has been linked to a higher risk of mortality in liver cirrhosis patients [15, 16]. Although the connection between oral health and liver disease is increasingly being studied, studies about the connection between oral infection foci and post-LT complications remain scarce.
Common complications after LT include graft rejection, biliary strictures, and various infections [17]. LT recipients also have increased risks of many diseases, such as diabetes, hypertension, cardiovascular disease, and cancer [17]. The risk factors for these complications in LT recipients are only partly known.
The objective of this study was to examine the connection and impact of pre-LT oral health on post-LT complications, such as graft rejection, cardiovascular disease, infections, cancer, and mortality. We hypothesized that LT recipients with worse oral health have more post-LT complications.
Patients and Methods
This study was performed in accordance with the Declaration of Helsinki and has been approved by the HUS ethics committee (192/13/03/02/2008. 12 August 2008).
This study included all 265 adult LT recipients who received a liver graft during the years 2000–2006 at Helsinki University Hospital (HUS), which is the only LT center in Finland. Children under 15 years were excluded from this study. Of these patients, 225 (total 233 liver transplantations) underwent a dental evaluation prior to transplantation. Forty patients either lacked sufficient dental data or did not undergo a pre-LT dental evaluation. A flowchart of the patients included in the study is shown in Supplementary Figure S1. The underlying indications for transplantation are presented in Supplementary Table S1.
Complication Data and Laboratory Values
Outcome data until the end of July 2020 were obtained from the national LT registry. The national LT registry contains follow-up data on relevant complications following LT. These data are collected during annual follow-up visits at the transplantation center and local hospitals [10]. Complications were grouped into severe infections requiring hospital care, cardiovascular disease, cancer, acute or chronic rejection, death or re-transplantation, and incidental diabetes, and were considered outcomes. For the 225 patients with dental data available, we also registered the model for end-stage liver disease (MELD) scores at transplantation, and 1 year-post-LT laboratory values for alanine aminotransferase (ALT), alkaline phosphatase (ALP), albumin, total bilirubin, gamma-glutamyl transferase (GGT), and c-reactive protein (CRP).
Dental Examination and Parameters
Dental screening for infection foci was performed for 225 patients before transplantation, and 191 of these patients underwent a clinical and radiographic (panoramic tomography x-ray) dental examination. However, 32 patients were evaluated only based on the panoramic tomography x-ray and two did not undergo either a full clinical examination or panoramic tomography x-ray because they were edentulous. Furthermore, for 218 of the 225 patients, acute infection foci were eliminated prior to transplantation. The clinical examination consisted of examining the extraoral status, the oral mucosa, the dentition and occlusion, and the periodontium. The oral health of the patients was evaluated using the modified total dental index (MTDI) score [18]. The MTDI score, presented in Table 1, considers the amount of caries lesions, edentulous jaws, radiological alveolar bone loss, number of apical lesions, and pericoronitis. A total score was counted for each patient, with a maximum possible score of 10 points. The patients were further divided into equal tertiles based on their MTDI score: low MTDI (0–2), medium MTDI [3] and high MTDI [4–10]. The low MTDI group was considered to have a low number of dental infection foci, whilst the high MTDI group was considered to have a high number of dental infection foci. A DMFT (decayed, missing, filled teeth) score was also registered for the patients, along with the number of extracted teeth.
TABLE 1
| Points | |
|---|---|
| Caries | |
| No caries lesions | 0 |
| 1–3 caries lesions | 1 |
| 4–7 caries lesions or no teeth in mandible or maxilla | 2 |
| ≥8 caries lesions or radix or no teeth | 3 |
| Periodontitis | |
| No alveolar bone loss | 0 |
| Alveolar bone loss in cervical third | 1 |
| Alveolar bone loss in middle third | 2 |
| Alveolar bone loss in apical third | 3 |
| Periapical lesions | |
| 1 periapical lesion or vertical bone pocket or both | 1 |
| 2 periapical lesions | 2 |
| ≥3 periapical lesions | 3 |
| Pericoronitis | |
| Absent | 0 |
| Present | 1 |
| Maximum score | 10 |
Definition and scoring of the Modified Total Dental Index (MTDI).
Data Analyses
The data analyses were performed using IBM SPSS Statistics software version 27.0 (SPSS, Inc., Armonk, NY, United States). Data are given as mean ± SD or count (%). Continuous variables were assessed for normality using the Shapiro–Wilk test and histograms. None of the continuous variables were normally distributed. Differences between groups were analyzed using the Fisher–Freeman–Halton exact test and, for nonparametric variables, using the Kruskal–Wallis test. For post hoc test Z-test for proportions and Dunn’s test, both Bonferroni corrected, were used as appropriate. The association between MTDI score and post-LT complications were first analyzed using univariate Cox regression analysis. Variables that were found to be significant in univariate analyses were further analyzed in multivariate analyses. Dental parameters and complications were adjusted for age, sex, indication for transplantation, smoking, pre-LT diabetes, MELD score at LT, and the number of LTs. Laboratory values were adjusted for sex, age at LT and MELD score at LT. We also analyzed whether there was a difference in the occurrence of complications between patients with or without pre-LT dental data with Cox regression models. Hazard ratios (HRs) with 95% confidence intervals (CIs) are reported. Linear regression analysis was used to assess the association between MTDI score and laboratory values, and p-values <0.05 were considered statistically significant.
Results
Basic Characteristics
Basic characteristics for patients with low, medium, and high MTDI scores are presented in Table 2. Patients in the high MTDI group were older compared to the low MTDI group (p = 0.027). The high MTDI group had a larger proportion of patients with acute rejection post-LT than the low MTDI group (p = 0.018). Analyses on dental parameters showed that patients in the low MTDI group had lower DMFT scores than patients in the medium MTDI group (p = 0.037) and the high MTDI group (p = 0.008). Patients in the low MTDI group also had more teeth before dental treatment compared to patients in the medium MTDI group (p = 0.005). Furthermore, patients in the high MTDI group had more teeth extracted pre-LT compared to the low MTDI group (p < 0.001). Moreover, patients in the low MTDI group had higher 1 year-post-LT albumin levels compared to patients in the medium MTDI group (p = 0.013) and the high MTDI group (p = 0.008).
TABLE 2
| Parameter | Low MTDI | Medium MTDI | High MTDI | p-value |
|---|---|---|---|---|
| Number of patients | 116 | 42 | 60 | |
| Agea (years) | 46.5 (±13.1) | 50.9 (±11.2) | 52.2 (±9.2) | 0.011 b |
| Sexc (male/female) | 58 (50%)/58 (50%) | 25 (60%)/17 (40%) | 40 (67%)/20 (33%) | 0.101 |
| Indication for transplantationc | ||||
| Chronic liver disease | 92 (79%) | 34 (81%) | 47 (78%) | |
| I) Primary sclerosing cholangitis | 30 (26%) | 9 (21%) | 10 (17%) | |
| II) Primary biliary cholangitis | 15 (13%) | 6 (14%) | 9 (15%) | |
| III) Alcohol cirrhosis | 15 (13%) | 9 (21%) | 17 (28%) | |
| IV) Cryptogenic cirrhosis/NASH | 12 (10%) | 4 (10%) | 7 (12%) | |
| V) Other cirrhosis | 12 (10%) | 8 (19.%) | 7 (12%) | |
| VI) Other CLDd | 16 (14%) | 3 (7%) | 2 (3%) | |
| Acute liver failure | 12 (10%) | 3 (7%) | 6 (10%) | |
| Tumor (all)e | 11 (10%) | 5 (12%) | 7 (12%) | |
| I) Tumor (no other CLD)f | 4 (3%) | 0 (0%) | 2 (3%) | |
| Metabolic disease | 1 (1%) | 0 (0%) | 0 (0%) | |
| Complication datac | ||||
| No of patients: ≥1 complication | 115 (99%) | 42 (100%) | 60 (100%) | 1.000 |
| No. of patients: no complications | 1 (1%) | 0 (0%) | 0 (0%) | |
| No. of patients: Survival | 0.133 | |||
| I) Retransplantation | 12 (10%) | 5 (12%) | 2 (3%) | |
| II) Death | 31 (27%) | 13 (31%) | 26 (43%) | |
| No. of patients: Infection | 77 (66%) | 31 (74%) | 39 (65%) | 0.601 |
| No. of patients: cardiovascular disease | 11 (10%) | 7 (17%) | 11 (18%) | 0.186 |
| No. of patients: Incident diabetes | 33 (28%) | 14 (33%) | 14 (23%) | 0.539 |
| No. of patients: Hypertension | 66 (57%) | 24 (57%) | 37 (62%) | 0.823 |
| No. of patients: Cancer | 31 (27%) | 10 (24%) | 18 (30%) | 0.878 |
| No. of patients: Acute rejection | 52 (45%) | 23 (55%) | 40 (67%) | 0.023 g |
| No. of patients: Chronic rejection | 3 (3%) | 0 (0%) | 1 (2%) | 0.816 |
| Dental parametersa | ||||
| DMFT score | 20.6 (±9.2) | 24.6 (±7.3) | 25.5 (±4.8) | 0.003h |
| Number of teeth pre dental treatment | 25.1 (±6.6) | 18.3 (±11.9) | 23.5 (±6.5) | 0.003i |
| Number of extracted teeth pre-LT | 1.4 (±2.2) | 2.4 (±3.5) | 7.4 (±5.1) | <0.001l |
| MELD score at LTa | 18.4 (±8.6) | 19.4 (±7.9) | 18.0 (±7.3) | 0.712 |
| Laboratory values at 1 year post-LTa | ||||
| P-ALT (U/L) | 32 (±23) | 34 (±33) | 55 (±59) | 0.102 |
| P-ALP (U/L) | 144 (±113) | 163 (±143) | 155 (±101) | 0.415 |
| P-Bilirubin (µmol/L) | 15 (±8) | 14 (±7) | 15 (±13) | 0.386 |
| P-Albumin (g/L) | 38 (±4) | 36 (±4) | 36 (±4) | 0.001k |
| P-GGT (U/L) | 89 (±188.03) | 88 (±140) | 131 (±212) | 0.117 |
| P-CRP (mg/L) | 3 (±14) | 3 (±10) | 4 (±15) | 0.582 |
Basic characteristics of the 218 LT patients who underwent elimination of dental infection foci pre-LT and the underlying indication for transplantation.
Patients with low (0–2), medium (3) and high (4–10) MTDI scores are compared.
Abbreviations: ALP, alkaline phosphatase; ALT, alanine aminotransferase; CLD, chronic liver disease, CRP, c-reactive protein; DMFT, decayed, missing, filled teeth; GGT, gamma-glutamyl transferase; LT, liver transplantation; MELD, model of end-stage liver disease; MTDI, modified total dental index; NASH, non-alcoholic steatohepatitis. Non-parametric variables were analyzed using Kruskal-Wallis test, and categorical variables using Fisher’s exact test. Post-hoc testing was done using, as appropriate, Dunn’s test and the Z-test for proportions, respectively, with both being Bonferroni corrected.
Data given as mean (SD).
In pairwise comparison, patients in the high MTDI group were significantly older than in the low MTDI group (p = 0.027).
Data given as n (%).
Other chronic liver diseases includes Budd–Chiari disease, polycystic disease, extrahepatic biliary atresia, congenital biliary fibrosis, alpha-1 antitrypsin deficiency, choledochal cyst, Caroli disease, and cystic fibrosis.
All patients with a tumor as the underlaying cause.
Patients with a tumor as the only underlaying cause.
The high MDTI group had a significantly larger proportion of patients with acute rejection compared to the low MTDI group (p = 0.018).
In pairwise comparison, patients in the low MTDI, group had significantly lower DMFT scores compared to patients in the medium MTDI group (p = 0.037) and the high MTDI group (p = 0.008).
In pairwise comparison, patients in the low MTDI group had significantly more teeth before dental treatment compared to patients in the medium MTDI group (p = 0.005).
In pairwise comparison, patients in the high MTDI group had significantly more teeth extracted compared to patients in the low MTDI group (p < 0.001) and medium MTDI, group (p < 0.001).
In pairwise comparison, patients in the medium MTDI group (p = 0.013) and high MTDI, group (p = 0.008) had significantly lower albumin values compared to patients in the low MTDI group.
Basic characteristics, including background, dental and outcome parameters, for patients with and without dental data are presented in Supplementary Table S1. The ratio between men and women differed significantly (p < 0.001) between the two groups; otherwise, no significant differences were observed.
Association Between Pre-LT MTDI Score and Post-LT Complications
The correlation between pre-LT MTDI score and post-LT complications was analyzed with a Cox regression. The results are shown in Supplementary Table S2. In univariate analysis with MTDI group (low, medium, high) as the independent variable, patients with high MTDI had a significantly higher risk of acute rejection compared to patients in the low MTDI group (HR 1.7, CI 95% 1.1–2.6, p = 0.012). No other significant findings between MTDI score and other complications were seen. When investigating the correlation between MTDI score and acute rejection further, we found that the results also remained significant after adjusting for age, sex, smoking, indication for LT, pre-LT diabetes, MELD score at transplantation, and re-transplant status (HR 1.9, CI 95% 1.2–3.0, p = 0.004). Furthermore, when adjusting for the time between dental evaluation and LT or the interaction variable between MTDI groups and the time between dental evaluation and LT, the results remained significant. Results are presented in Figure 1.
FIGURE 1
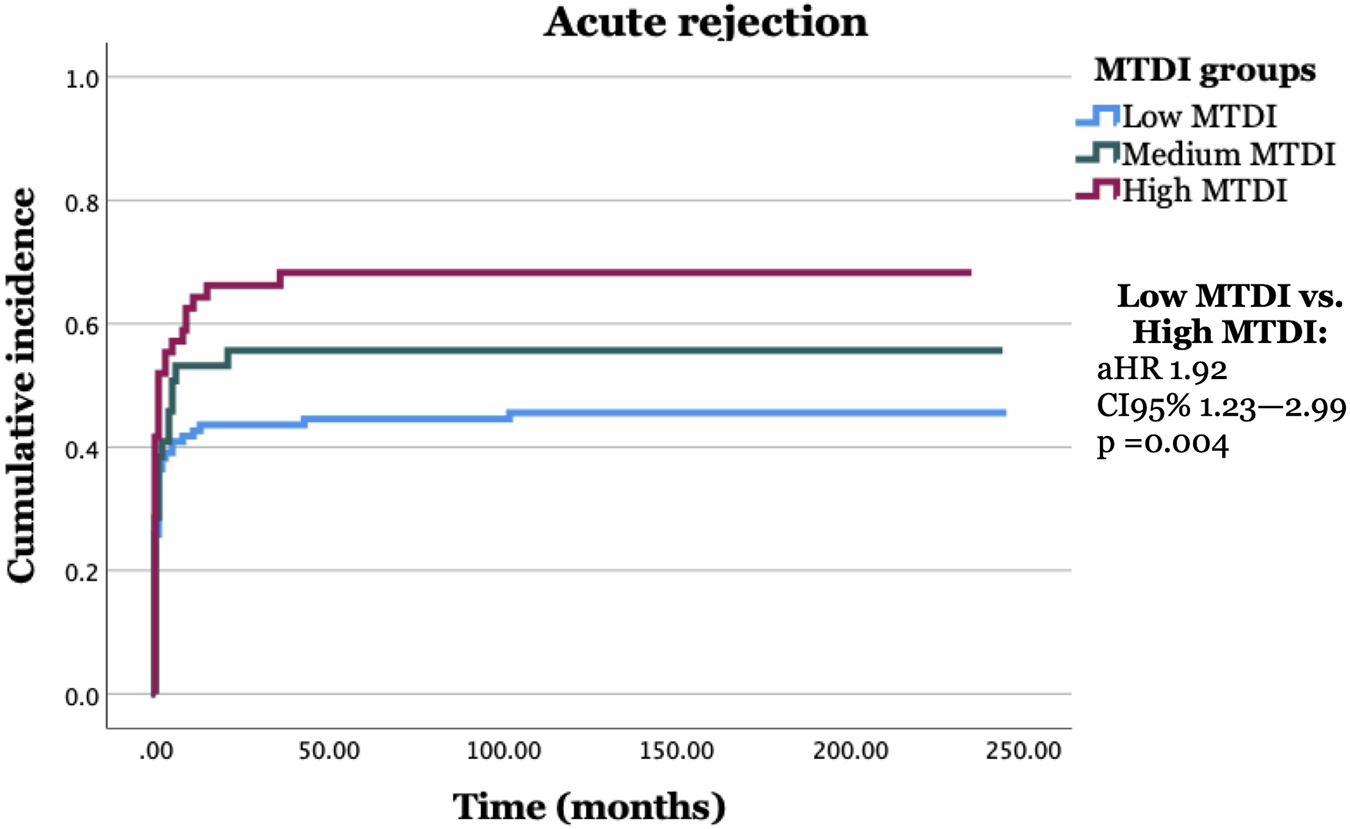
Liver transplant (LT) recipients with a high need for dental treatment (high MTDI) and multiple infection foci pre-LT expressed significantly more acute rejection post-LT compared to LT recipients with a low or no need for dental treatment (low MTDI) pre-LT.
Moreover, the proportion of LT recipients with more than one acute rejection episode was significantly higher (p = 0.014) in the high MTDI group (20%) compared to the low MTDI group (6%). No significant difference was found when analyzing the correlation between MTDI group and early (<3 months post-LT) or late (>3 months post-LT) acute rejection.
Association of Pre-LT MTDI Score and Dental Data With 1 year-post-LT Laboratory Values
In Table 3, the results of the linear regression analysis of the correlation between MTDI score as a continuous variable and 1 year-post-LT laboratory values for ALT, ALP, bilirubin, albumin, GGT and CRP are shown. There was a significant association between a higher MTDI score and higher ALT values (β = 4.0, CI 95% 1.2–6.7, R2 = 0.039, p = 0.005) and with lower albumin values (β = −0.5, CI 95% −0.8 to −0.2, R2 = 0.052, p = 0.001). The results remained significant after adjusting for sex, age at LT, and MELD score at LT (β = 4.2, CI 95% 1.3–7.1, R2 = 0.04, p = 0.005 and β = −0.5, CI 95% −0.8–0.2 R2 = 0.1, p = 0.002, respectively).
TABLE 3
| Laboratory value | β | CI 95% for B | R 2 | p-value |
|---|---|---|---|---|
| P-ALT (U/L) | 3.97 | 1.20–6.74 | 0.038 | 0.005 |
| P-ALP (U/L) | 3.44 | −4.87–11.75 | 0.415 | |
| P-Bilirubin (µmol/L) | 0.09 | −0.58–0.76 | 0.782 | |
| P-Albumin (g/L) | −0.48 | −0.77 to −0.19 | 0.052 | 0.001 |
| P-GGT (U/L) | 12.44 | −0.93–25.82 | 0.068 | |
| P-CRP (mg/L) | 0.78 | −0.20–1.75 | 0.119 |
Univariate linear regression analysis of the connection between MTDI score and laboratory values 1 year post-transplantation.
Abbreviations: ALP, alkaline phosphatase; ALT, alanine aminotransferase, CRP, c-reactive protein, GGT, gamma-glutamyl transferase.
β = regression coefficient.
These results concern 218 patients whose teeth were examined and treated pre-transplantation.
MTDI score (0–10) analyzed as a continuous variable.
When further analyzing whether the pre-LT number of teeth correlates with 1 year-post-LT ALT and albumin values in separate linear regression analysis, we found that fewer teeth associated with lower albumin values (β = 0.2, CI 95% 0.04–0.2, R2 = 0.05, p = 0.002).
Discussion
The main finding in our study was that patients with high pre-LT MTDI scores, indicating a worse dental status, seemed to have a higher risk of acute post-LT rejection compared to patients with low pre-LT MTDI scores. Furthermore, a higher MTDI score seems to associate with higher 1 year-post-LT ALT levels and lower albumin levels.
To the best of the authors’ knowledge, the association between poor dental status and acute rejection post-LT has not been reported in LT recipients previously. In our study, we found that a higher MTDI score (worse oral health) independently predicts acute rejection. The correlation remained significant even when adjusted for confounders. Previous studies on kidney transplant recipients show contradictory results on the matter. Zweich et al. [19] showed that poor oral hygiene was an indicator for increased risk of hospitalization and acute rejection, and found that the Community Periodontal Index of Treatment Needs correlated with acute rejections in kidney transplant recipients. However, other studies have demonstrated no correlation between pre-transplant oral health and graft rejection [20, 21]. One study showed that severe periodontitis in kidney transplant recipients was independently associated with a lower incidence of acute T-cell-mediated rejection, which was hypothesized to depend on the immunomodulatory effect of periodontitis [22].
In this study, all acute odontogenic infection foci were treated pre-LT. However, not all patients underwent periodontal treatment systematically. A potential link between periodontitis/gingivitis and graft rejection could be a periodontitis-related, IL-6-modulated, pro-inflammatory state. IL-6 production can be induced by both pathogen-associated molecular patterns and pro-inflammatory cytokines, and it seems to have a pro-inflammatory effect on the adaptive immune response [23]. In the solid organ transplantation context, IL-6 has been shown to promote acute allograft rejection [24–26]. Periodontitis has been shown to increase levels of proinflammatory cytokines such as TNF-alfa, IL-1 and IL-6 [27]. In particular, patients with chronic periodontitis have elevated levels of proinflammatory cytokines, including IL-6, in the gingival crevicular fluid and serum compared to healthy controls [28, 29]. Periodontal treatment, in turn, is shown to lower the levels of these proinflammatory cytokines [29, 30]. Thus, we hypothesize that untreated periodontal inflammation plays a role in the development of acute rejection.
Previous publications on the association between liver enzymes and oral health are contradictory and are mainly focused on periodontitis. Some studies show no association between liver enzyme values and alveolar bone loss in patients without liver disease [31, 32], while other studies show higher liver enzyme levels in patients with periodontitis [33, 34]. Some studies hypothesize that periodontal disease might be a risk factor for the development of non-alcoholic steatohepatitis [35–37] and chronic liver disease [38]. Our results showed significantly higher ALT levels and significantly lower albumin levels in patients with worse dental health. ALT is a highly liver-specific enzyme, and it being elevated in patients with worse oral health supports our hypothesis that untreated oral or dental inflammation might also influence the liver post-LT. Poor nutrition is shown to reduce albumin production [39]. In our study, worse oral health and fewer teeth were associated with lower albumin values. Hence, worse oral health and fewer teeth may contribute to malnutrition by negatively affecting chewing capacity and mastication; this connection has previously been discussed in patients with chronic kidney disease [40].
Our study reports novel findings on the connection between oral health and post-LT complications. Strengths of our study include the long follow-up time, the utilization of data from the national LT registry, and using both clinical and laboratory data. Despite the novel findings, our study has limitations. In this study setting we could not collect detailed data on the patients’ periodontal status and periodontal treatment. Furthermore, our study analyzed oral health as a whole, and we were not able to exam different oral diseases separately, due to our retrospective study setting not allowing this. Moreover, two of the patients did not undergo a clinical or radiological examination because they were edentulous, which increases the risk for error in our analyses. However, we chose to include these patients, since the examinations would not have changed their MTDI scores. Another limitation is the relatively small sample size. However, we included all eligible patients in Finland, and this country-wide setting is a strength of our study. Despite its limitations, our study provides novel results on the possible connection between poor oral health and post-LT acute rejection, and the results remain indicative despite these limitations. However, despite the link, common confounders might affect both poor oral health and acute rejection post-LT. Therefore, further studies examining confounders affecting this relationship are needed. A possible area of further research based on this study would be the impact of oral diseases on post-LT complications, especially acute rejection. Another interesting topic for further study would be to assess the impact of receiving periodontal treatment prior to transplantation, while adjusting for the stage of periodontal disease.
Conclusion
In conclusion, poor pre-LT oral health seems to be associated with an increased risk of post-LT acute rejection. Poor oral health is also associated with elevated ALT levels and decreased albumin levels, suggesting an effect on post-LT liver health. Therefore, attention should be given to treating oral and dental issues early in the course of liver disease and to highlighting the importance of maintaining good oral hygiene.
Statements
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Helsinki University Hospital Ethics committee. The studies were conducted in accordance with the local legislation and institutional requirements. The human samples used in this study were acquired from a by-product of routine care or industry. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
AO: contributed to conception and design of the study, organized the database, preformed the statistical analysis and wrote the manuscript. FÅ contributed to conception and design of the study, contributed to the statistical analysis and wrote sections of the manuscript. JH-H, AN, JS, and HR: contributed to conception and design of the study and wrote sections of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was financially supported by Helsinki University Hospital Research Funding: EVO grant Y1014SUU002 and a grant from The Finnish Dental Society Apollonia and Odontologiska Samfundet i Finland.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontierspartnerships.org/articles/10.3389/ti.2023.11534/full#supplementary-material
References
1.
Tomofuji T Ekuni D Yamanaka R Kusano H Azuma T Sanbe T et al Chronic Administration of Lipopolysaccharide and Proteases Induces Periodontal Inflammation and Hepatic Steatosis in Rats. J Periodontol (2007) 78(10):1999–2006. 10.1902/jop.2007.070056
2.
Yoneda M Naka S Nakano K Wada K Endo H Mawatari H et al Involvement of A Periodontal Pathogen, Porphyromonas Gingivalis on the Pathogenesis of Non-Alcoholic Fatty Liver Disease. BMC Gastroenterol (2012) 12:16. 10.1186/1471-230x-12-16
3.
Aberg F Helenius-Hietala J Meurman J Isoniemi H . Association Between Dental Infections and the Clinical Course of Chronic Liver Disease. Hepatol Res (2014) 44(3):349–53. 10.1111/hepr.12126
4.
Gronkjaer LL Holmstrup P Schou S Kongstad J Jepsen P Vilstrup H . Periodontitis in Patients With Cirrhosis: A Cross-Sectional Study. BMC Oral Health (2018) 18(1):22. 10.1186/s12903-018-0487-5
5.
Gronkjaer LL Vilstrup H . Oral Health and Liver Disease. Liver Int (2019) 39(5):995. 10.1111/liv.14033
6.
Rustemeyer J Bremerich A . Necessity of Surgical Dental Foci Treatment Prior to Organ Transplantation and Heart Valve Replacement. Clin Oral Investig (2007) 11(2):171–4. 10.1007/s00784-007-0101-8
7.
Helenius-Hietala J Aberg F Meurman JH Isoniemi H . Increased Infection Risk Postliver Transplant Without Pretransplant Dental Treatment. Oral Dis (2013) 19(3):271–8. 10.1111/j.1601-0825.2012.01974.x
8.
Göbel P Forsting C Klüners A Knipper P Manekeller S Nattermann J et al Persisting Dental Foci Increase the Risk for Bacterial Infections Before and After Liver Transplant. Clin Transpl (2022) 2022:e14857. 10.1111/ctr.14857
9.
Fishman JA . Infection in Solid-Organ Transplant Recipients. N Engl J Med (2007) 357(25):2601–14. 10.1056/NEJMra064928
10.
Aberg F Mäkisalo H Höckerstedt K Isoniemi H . Infectious Complications More Than 1 Year After Liver Transplantation: A 3-Decade Nationwide Experience. Am J Transpl (2011) 11(2):287–95. 10.1111/j.1600-6143.2010.03384.x
11.
Kauffels ASG Kollmar O Slotta JE Weig M Groß U Bader O et al Oral Findings and Dental Behaviour Before and After Liver Transplantation - A Single-Centre Cross-Sectional Study. Int J Dentistry (2017) 67(4):244–51. 10.1111/idj.12290
12.
Grønkjær LL . Periodontal Disease and Liver Cirrhosis: A Systematic Review. SAGE Open Med (2015) 3:2050312115601122. 10.1177/2050312115601122
13.
Castellanos-Cosano L Machuca-Portillo G Segura-Sampedro JJ Torres-Lagares D López-López J Velasco-Ortega E et al Prevalence of Apical Periodontitis and Frequency of Root Canal Treatments in Liver Transplant Candidates. Med Oral Patol Oral Cir Bucal (2013) 18(5):e773–9. 10.4317/medoral.19148
14.
Silva Santos PS Fernandes KS Gallottini MH . Assessment and Management of Oral Health in Liver Transplant Candidates. J Appl Oral Sci (2012) 20(2):241–5. 10.1590/s1678-77572012000200020
15.
Grønkjær LL Holmstrup P Jepsen P Vilstrup H . The Impact of Oral Diseases in Cirrhosis on Complications and Mortality. JGH Open (2021) 5(2):294–300. 10.1002/jgh3.12489
16.
Grønkjær LL Holmstrup P Schou S Jepsen P Vilstrup H . Severe Periodontitis and Higher Cirrhosis Mortality. United Eur Gastroenterol J (2018) 6(1):73–80. 10.1177/2050640617715846
17.
Åberg F Isoniemi H Höckerstedt K . Long-Term Results of Liver Transplantation. Scand J Surg (2011) 100(1):14–21. 10.1177/145749691110000104
18.
Mattila KJ Nieminen MS Valtonen VV Rasi VP Kesäniemi YA Syrjälä SL et al Association Between Dental Health and Acute Myocardial Infarction. Bmj (1989) 298(6676):779–81. 10.1136/bmj.298.6676.779
19.
Zwiech R Bruzda-Zwiech A . Does Oral Health Contribute to Post-Transplant Complications in Kidney Allograft Recipients?Acta Odontol Scand (2013) 71(3-4):756–63. 10.3109/00016357.2012.715203
20.
Schander K Jontell M Johansson P Nordén G Hakeberg M Bratel J . Oral Infections and Their Influence on Medical Rehabilitation in Kidney Transplant Patients. Swed Dent J (2009) 33(3):97–103.
21.
Sarmento DJS Caliento R Maciel RF Braz-Silva PH Pestana J Lockhart PB et al Poor Oral Health Status and Short-Term Outcome of Kidney Transplantation. Spec Care Dentist (2020) 40(6):549–54. 10.1111/scd.12512
22.
Min HJ Park JS Yang J Yang J Oh SW Jo SK et al The Effect of Periodontitis on Recipient Outcomes After Kidney Transplantation. Kidney Res Clin Pract (2022) 41(1):114–23. 10.23876/j.krcp.21.097
23.
Pan W Wang Q Chen Q . The Cytokine Network Involved in the Host Immune Response to Periodontitis. Int J Oral Sci (2019) 11(3):30. 10.1038/s41368-019-0064-z
24.
Booth AJ Grabauskiene S Wood SC Lu G Burrell BE Bishop DK . IL-6 Promotes Cardiac Graft Rejection Mediated by CD4+ Cells. J Immunol (2011) 187(11):5764–71. 10.4049/jimmunol.1100766
25.
Poppelaars F Gaya da Costa M Eskandari SK Damman J Seelen MA . Donor Genetic Variants in Interleukin-6 and Interleukin-6 Receptor Associate With Biopsy-Proven Rejection Following Kidney Transplantation. Sci Rep (2021) 11(1):16483. 10.1038/s41598-021-95714-z
26.
Yao J Feng XW Yu XB Xie HY Zhu LX Yang Z et al Recipient Il-6-572c/G Genotype Is Associated With Reduced Incidence of Acute Rejection Following Liver Transplantation. J Int Med Res (2013) 41(2):356–64. 10.1177/0300060513477264
27.
Cardoso EM Reis C Manzanares-Céspedes MC . Chronic Periodontitis, Inflammatory Cytokines, and Interrelationship With Other Chronic Diseases. Postgrad Med (2018) 130(1):98–104. 10.1080/00325481.2018.1396876
28.
Stadler AF Angst PD Arce RM Gomes SC Oppermann RV Susin C . Gingival Crevicular Fluid Levels of Cytokines/Chemokines in Chronic Periodontitis: A Meta-Analysis. J Clin Periodontol (2016) 43(9):727–45. 10.1111/jcpe.12557
29.
Shimada Y Komatsu Y Ikezawa-Suzuki I Tai H Sugita N Yoshie H . The Effect of Periodontal Treatment on Serum Leptin, Interleukin-6, and C-Reactive Protein. J Periodontol (2010) 81(8):1118–23. 10.1902/jop.2010.090741
30.
Teeuw WJ Slot DE Susanto H Gerdes VE Abbas F D'Aiuto F et al Treatment of Periodontitis Improves the Atherosclerotic Profile: A Systematic Review and Meta-Analysis. J Clin Periodontol (2014) 41(1):70–9. 10.1111/jcpe.12171
31.
Kuroki A Sugita N Komatsu S Yokoseki A Yoshihara A Kobayashi T et al Association of Liver Enzyme Levels and Alveolar Bone Loss: A Cross-Sectional Clinical Study in Sado Island. J Clin Exp Dent (2018) 10(2):e100–6. 10.4317/jced.54555
32.
Wiener RC Sambamoorthi U Jurevic RJ . Association of Alanine Aminotransferase and Periodontitis: A Cross-Sectional Analysis-NHANES 2009-2012. Int J Inflam (2016) 2016:3901402. 10.1155/2016/3901402
33.
Saito T Shimazaki Y Koga T Tsuzuki M Ohshima A . Relationship Between Periodontitis and Hepatic Condition in Japanese Women. J Int Acad Periodontol (2006) 8(3):89–95.
34.
Furuta M Ekuni D Yamamoto T Irie K Koyama R Sanbe T et al Relationship Between Periodontitis and Hepatic Abnormalities in Young Adults. Acta Odontol Scand (2010) 68(1):27–33. 10.3109/00016350903291913
35.
Kuraji R Sekino S Kapila Y Numabe Y . Periodontal Disease-Related Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis: An Emerging Concept of Oral-Liver axis. Periodontol 2000 (2021) 87(1):204–40. 10.1111/prd.12387
36.
Akinkugbe AA Slade GD Barritt AS Cole SR Offenbacher S Petersmann A et al Periodontitis and Non-Alcoholic Fatty Liver Disease, A Population-Based Cohort Investigation in the Study of Health in Pomerania. J Clin Periodontol (2017) 44(11):1077–87. 10.1111/jcpe.12800
37.
Widita E Yoshihara A Hanindriyo L Miyazaki H . Relationship Between Clinical Periodontal Parameters and Changes in Liver Enzymes Levels Over an 8-Year Period in an Elderly Japanese Population. J Clin Periodontol (2018) 45(3):311–21. 10.1111/jcpe.12861
38.
Helenius-Hietala J Suominen AL Ruokonen H Knuuttila M Puukka P Jula A et al Periodontitis Is Associated With Incident Chronic Liver Disease-A Population-Based Cohort Study. Liver Int (2019) 39(3):583–91. 10.1111/liv.13985
39.
Aller de la Fuente R . Nutrition and Chronic Liver Disease. Clin Drug Investig (2022) 42(1):55–61. 10.1007/s40261-022-01141-x
40.
Ioannidou E Swede H Fares G Himmelfarb J . Tooth Loss Strongly Associates With Malnutrition in Chronic Kidney Disease. J Periodontol (2014) 85(7):899–907. 10.1902/jop.2013.130347
Summary
Keywords
oral health, liver transplantation, acute rejection, infection foci, oral disease
Citation
Olander AE, Helenius-Hietala J, Nordin A, Savikko J, Ruokonen H and Åberg F (2023) Association Between Pre-Transplant Oral Health and Post-Liver Transplant Complications. Transpl Int 36:11534. doi: 10.3389/ti.2023.11534
Received
02 May 2023
Accepted
30 August 2023
Published
12 September 2023
Volume
36 - 2023
Updates
Copyright
© 2023 Olander, Helenius-Hietala, Nordin, Savikko, Ruokonen and Åberg.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Annika Emilia Olander, annika.norrman@helsinki.fi
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.