Abstract
Death by suicide is a global epidemic with over 800 K suicidal deaths worlwide in 2012. Suicide is the 10th leading cause of death among Americans and more than 44 K people died by suicide in 2019 in the United States. Patients with chronic pain, including, but not limited to, those with substance use disorders, are particularly vulnerable. Chronic pain patients have twice the risk of death by suicide compared to those without pain, and 50% of chronic pain patients report that they have considered suicide at some point due to their pain. The kappa opioid system is implicated in negative mood states including dysphoria, depression, and anxiety, and recent evidence shows that chronic pain increases the function of this system in limbic brain regions important for affect and motivation. Additionally, dynorphin, the endogenous ligand that activates the kappa opioid receptor is increased in the caudate putamen of human suicide victims. A potential treatment for reducing suicidal ideation and suicidal attempts is buprenorphine. Buprenorphine, a partial mu opioid agonist with kappa opioid antagonist properties, reduced suicidal ideation in chronic pain patients with and without an opioid use disorder. This review will highlight the clinical and preclinical evidence to support the use of buprenorphine in mitigating pain-induced negative affective states and suicidal thoughts, where these effects are at least partially mediated via its kappa antagonist properties.
Introduction
Suicide is a pressing public health issue that accounts for more than 800,000 deaths per year globally [1]. In the United States, it is one of the 10 leading causes of death claiming more than 47,000 lives in 2019, and the second leading cause of death in people aged 10 to 34 [2]. The rates of suicide have risen more than 30% between 1999–2019. The United States Surgeon General and Department of Health and Human Services have recently issued a call to action to implement the National Strategy for Suicide Prevention that includes calls for treatment access to those that need it [3]. Important, for this review, is that chronic pain is second only to bipolar disorder as the major cause of suicide among all medical illnesses [4, 5]. Suicide is typically preceded by suicidal ideation–persistent thoughts about wanting to kill oneself. While suicidal ideation only rarely leads to the completion of suicide (death), it is an important clinical marker, and prior suicide attempt is the single strongest risk factor for future suicidal behaviors and death by suicide [6].
Recently, there has been a dramatic increase in the prevalence of suicidal ideation during the COVID-19 pandemic and subsequent mitigation activities, including social distancing and stay-at-home orders [7, 8]. In June 2020, 10.7% of adults reported thoughts of suicide compared to 4.3% of adults in 2018 [9]. Fortunately, suicide rates themselves have remained unchanged or declined early in the pandemic [10]. However, the management of patients suffering from suicidal ideation represents a rapidly growing clinical challenge. There are currently few pharmacological treatments available that specifically alleviate suicidal ideation; therefore, research into this clinical problem has the potential to save many lives.
Suicidal ideation occurs in a subset of individuals with major depressive disorder (MDD); however, emerging evidence suggests that suicidal ideation may also represent a distinct behavioral disorder [11]. For example, improvements in suicidal ideation following ketamine treatment cannot be entirely explained by improvements in depression or anxiety [12]. Suicidality also often presents with mental health disorders other than depression. Substance use is a risk factor for suicide attempts, and individuals with substance use disorders have a 10–14 times greater risk of death by suicide compared to the general population [13–15]. Many substance overdoses may also be unrecognized suicides [16]. Some studies have demonstrated that anxiety disorder comorbidity with other mood disorders is a risk factor for suicide attempts, though this finding has been inconsistent [17]. The comorbidity of borderline personality disorder and depression is associated with an increase in the number and seriousness of suicide attempts [18].
Acute and chronic alcohol use also play major roles in suicidal behavior. Approximately 26% of suicide decedents who were tested for alcohol had intoxicating blood alcohol levels (>0.08%) [19]. According to recent meta-analyses, which include case-control and cohort studies, individuals with alcohol use disorder (AUD) have three times greater odds of suicidal behavior compared to those without the disorder [20, 21]. Furthermore, AUD has been identified as the second most common mental disorder among suicide decedents [22].
Finally, suicidal ideation is highly prevalent in chronic pain patients [23–26], even when controlling for the subjective severity of pain symptoms [27–29] and the presence of other affective disorders [27, 30, 31]. For such patients, suicide is viewed as a means to alleviate overwhelming and intolerable painful internal states, and psychological and emotional pain have been considered essential for suicidal behavior [32, 33]. A recent metanalysis of 31 studies showed a significant link between physical pain and suicidal thoughts and behaviors, where physical pain was associated with lifetime death wish, current and lifetime suicidal ideation, suicide plan, and suicide attempts, as well as death [34]. Some of the predictors of suicidal ideation in chronic pain patients include mental defeat [35], insomnia [36], and pain catastrophizing [37], which are also risk factors for opioid use disorder. Suicidal ideation in chronic pain patients is associated with depression, anxiety and sleep disorders [38]. This review will highlight recent data that provides justification for further clinical trials to test the potential of buprenorphine as a treatment for suicidal ideation, particularly in chronic pain patients.
The Affective (Emotional) Dimension of Pain and Suicidal Ideation
Chronic pain has both sensory and emotional/affective components that, while distinct, share many of the same neurobiological substrates. Chronic pain often induces a persistent negative affective state, or “emotional pain,” likely as a result of neuroadaptations in the brain’s reward processing circuitry [39–41]. Chronic pain is also associated with the development of other disorders of impaired reward processing, including depression and substance use disorders [42]. The prevalence of suicidal ideation among pain patients suggests that it may be an expression of emotional pain. In fact, studies have found emotional pain to be the psychological variable most strongly associated with current suicidality, even more so than the presence of depressed mood or hopelessness [18, 43, 44].
The relationship between AUD and suicidality also suggests that suicidal ideation may be an expression of emotional pain. That AUD is often a key risk factor for suicidal behavior is likely due, at least in part, to alcohol-induced exacerbations in negative emotionality and alcohol-related negative consequences, particularly in interpersonal domains [45]. Hyper-negative emotional states and hyperalgesia are both consequences of repeated alcohol use [46] and may contribute to an increase in alcohol use as a compensatory mechanism [47]. Among heavy drinkers, the negative emotional components of pain (i.e., pain catastrophizing) can enhance alcohol craving more than physical pain [48].
The emotional pain caused by the disruption or loss of social attachments also plays an important role in suicidality. In particular, suicidal ideation shares neurobiological and psychological features with separation distress—the innate, emotionally painful, dysphoric response of animals and humans to social separation or rejection [49, 50]. Converging evidence from preclinical and clinical studies supports the link between suicidal ideation and separation distress. Opioids reduce separation distress behaviors in non-human mammals [51–53] and have recently shown promise for the treatment of suicidality [54, 55]. Suicidal acts are most common after interpersonal losses or rejections [56], and patients with borderline personality disorder are particularly susceptible to social rejection and often become suicidal after interpersonal rejections [57, 58].
An Affective Neuroscience Model Linking Pain, Suicidal Ideation, and Depression
Research in the field of affective neuroscience suggests that separation distress represents one of the ancestral primary-process emotional systems (referred to as PANIC/GRIEF) [49, 50, 59, 60]. Importantly, the PANIC/GRIEF system probably evolved from general pain mechanisms [59], and studies have found a link between separation distress and physical pain. Maternal separation in mouse neonates is capable of altering nociceptive behavior in adulthood [61, 62]. In humans, early life adversity in the form of both physical and psychological trauma (including familial separation) is associated with an increased risk of chronic pain in later life [63]. Studies show that parental bonding in adolescents is significantly associated with adolescent chronic pain and depression, where low maternal care contributes to increased pain via heightened depressive symptoms [64].
The neuroanatomy of the PANIC/GRIEF system overlaps with the brain’s system for processing physical pain [65], suggesting that both physically painful (e.g., injury) and emotionally painful (e.g., interpersonal rejection) stimuli may engage this shared neurocircuitry to produce distress and dysphoria (emotional pain), with separation distress representing a particular subtype of emotional pain. The PANIC/GRIEF system also represents a potential substrate linking emotional pain/distress with suicidal ideation. The similarities between suicidal ideation and separation distress discussed above suggest that suicidal ideation may result from increased activity in the brain’s PANIC/GRIEF network, whether initiated by social loss or physical injury. Thus, chronic pain patients may be particularly susceptible to suicidal ideation due to persistent activation of this system by painful sensory stimuli.
Sustained activation of the PANIC/GRIEF system can also lead to reduced activity in the brain reward SEEKING system (the system primarily responsible for motivation and arousal, particularly the mesolimbic dopamine pathway), perhaps as a means to protect against sustained emotional pain by reducing the overall arousal of emotions [49, 50, 59, 66]. Underactivity in the SEEKING system causes blunted reward processing, leading to an amotivational state characterized by the diminished experience of positive feelings (anhedonia). Thus, down-regulation of the SEEKING system in response to sustained emotional pain (dysphoria) may be one underlying cause of the anhedonia and blunted affect that is characteristic of depression.
This two-stage model then suggests that the anhedonia of depression may reflect, in part, an emotional shutdown that follows the behavioral agitation of separation distress or other emotional pain, with these behavioral states correlating with underactivity of the SEEKING network and overactivity of the separation distress PANIC/GRIEF network, respectively. Of course, depression is a complex disorder that likely has multiple etiologies involving changes in many neural substrates. However, this model suggests one possible framework for understanding the relationship between suicidal ideation and depression. Sustained activation of the PANIC/GRIEF network may produce both a state of dysphoria that leads to suicidal ideation as well as, indirectly, a reduction in motivation (anhedonia) through subsequent downregulation of the reward SEEKING system (Figure 1). In this way, suicidal ideation would often be comorbid with depression but could be the result of dysregulation of the PANIC/GRIEF circuitry independent of a disruption in reward processing. In support of this hypothesis, patients with borderline personality disorder, but not comorbid depression, typically experience brief durations of suicidality as a result of interpersonal stresses. In contrast, patients with comorbid borderline personality disorder and depression display more persistent symptoms of depression and suicidality, which also include a loss of interest in ordinarily pleasurable activities (anhedonia) [18].
FIGURE 1
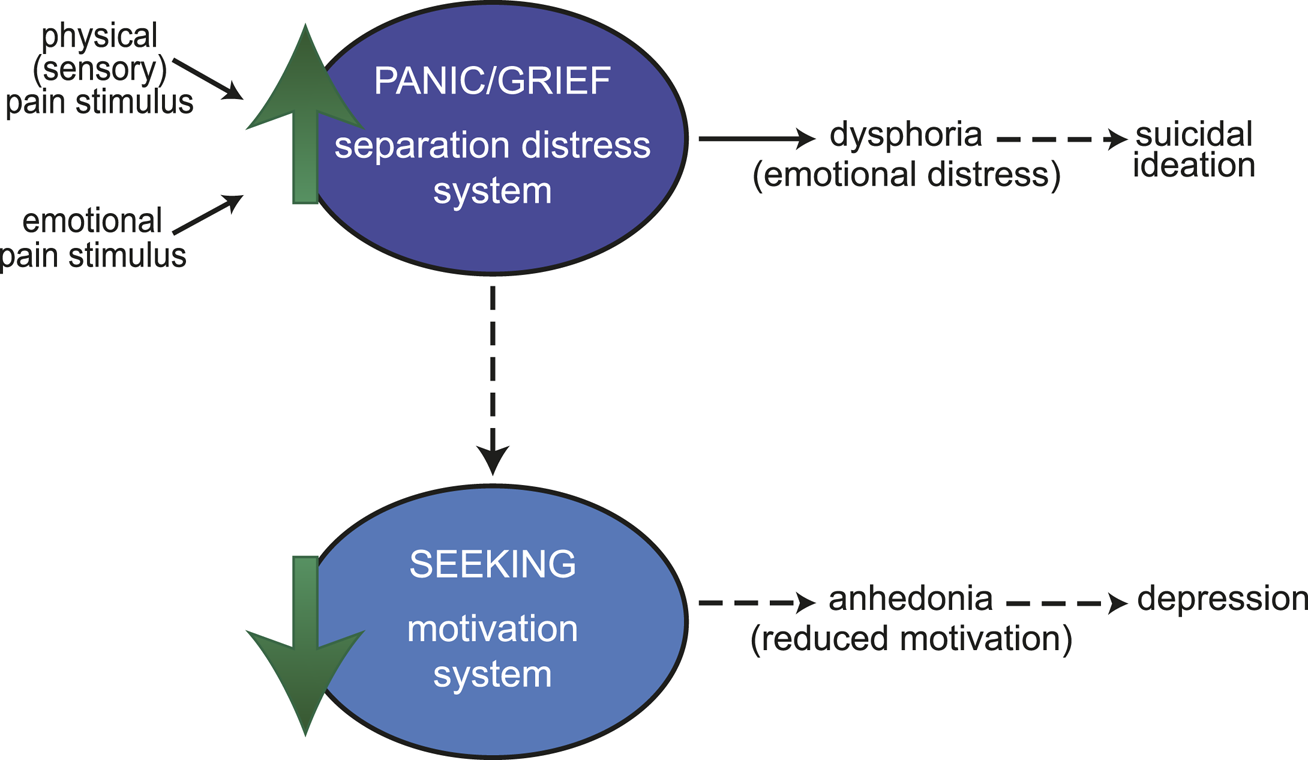
An affective neuroscience model linking pain, suicidal ideation, and depression. Both physical (sensory) pain (such as injury) and emotional pain (such as interpersonal rejection) stimuli can act on the PANIC/GRIEF (separation distress) system. An increase in activity in this system produces dysphoria (emotional distress). Sustained activation of the PANIC/GRIEF system (dotted lines) could lead to suicidal ideation and a reduction in downstream activity of the SEEKING (motivation) system. Reduced motivation (anhedonia) may then result in loss of interest in activities characteristic of depression. This model suggests that suicidal ideation would often be comorbid with depression but could also occur independently of a disruption in reward processing.
Ultimately, painful experiences (whether the emotional pain of social rejection or the physical/sensory pain characteristic of chronic pain conditions) likely engage shared brain systems which produce negative affective states (distress/dysphoria–implicated in suicidal ideation) and may subsequently disrupt downstream reward processing (anhedonia–implicated in depression), leading to a complex relationship between pain, separation/social distress, and motivation [65, 67, 68]. The neurocircuitry and neurochemistry underlying each is discussed in more detail below.
Neurocircuitry of Pain, Separation/Social Distress, and Motivation
Acute and Chronic Pain
Pain is a multidimensional experience comprised of sensory, cognitive, and emotional components. The sensory aspects of pain are relayed from peripheral nociceptors, which detect noxious sensory stimuli, along primary afferent neurons that have central terminals in the spinal cord [69]. The second order neurons in the spinal cord ascend to various brain structures including the nucleus of the solitary tract, the medial brain stem reticular formation, the caudal ventrolateral medulla, the lateral parabrachial nucleus, the midbrain periaqueductal gray, and the thalamus and the hypothalamus [69, 70]. The classical pathways associated with ascending nociceptive information are the lateral and medial spinothalamic pathways, where the lateral is responsible for sharp, well-localized pain and the medial is for diffuse, poorly localized persistent pain. Sensory information such as pain intensity and location (discriminative aspects of pain) is then relayed along the lateral spinothalamic tract to the primary and secondary somatosensory cortices via the medial thalamic nuclei. A descending pain modulation system originating in the periaqueductal gray (PAG) also regulates pain signals at the level of the spinal cord before they are relayed to higher subcortical and cortical structures [71].
The emotional and motivational aspects of pain (e.g., subjective unpleasantness and salience) are carried to limbic structures such as the amygdala, hypothalamus, striatum, insula, and anterior cingulate cortex by the medial spinothalamic tract [72–74] (Figure 2). A key structure for encoding the affective component of pain is the parabrachial complex located in the pons, receiving dense inputs form lamina I nociceptive spinal neurons; a projection reportedly denser than the spinothalamic pathway [75, 76]. The parabrachial complex projects to several regions involved in pain and affect including the PAG, rostroventral medulla, thalamus, amygdala and zona incerta, making it a key structure for the affective emotional perception of pain.
FIGURE 2
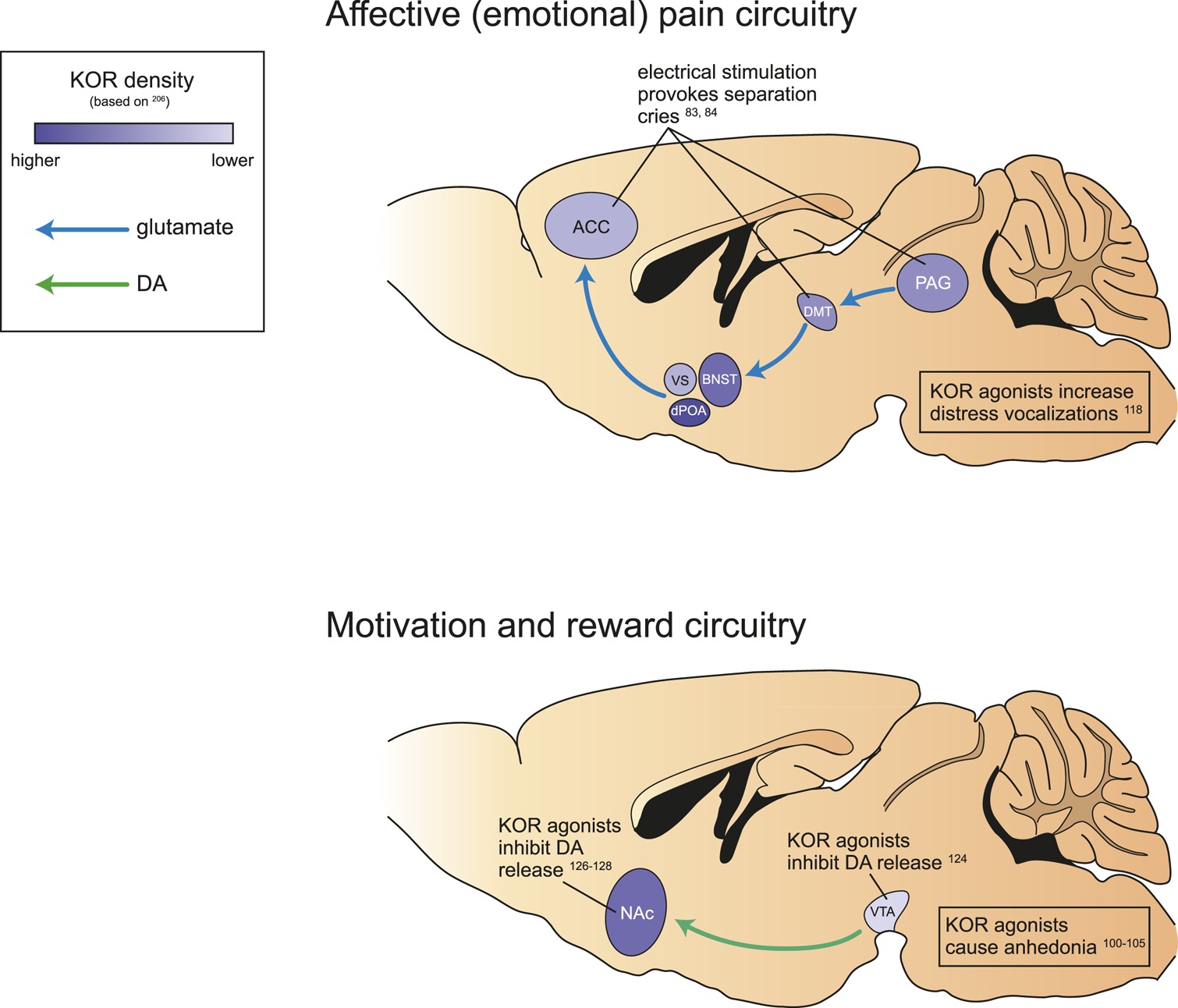
Neurocircuitry and kappa opioid signaling involved in affective (emotional) pain and motivation and reward. Schematic of brain areas implicated in affective (emotional) pain, particularly separation distress (top), and motivation and reward (bottom) in rodents. Both circuits are altered by activity at KOR (present to varying degrees in all relevant brain regions). KOR antagonism increases distress vocalizations, inhibits mesolimbic DA release, and causes associated dysphoria and anhedonia. anterior cingulate cortex, ACC; ventral septum, VS; dorsal preoptic area, dPOA; bed nucleus of the stria terminalis, BNST; dorsalmedial thalamus, DMT; periaqueductal gray, PAG; nucleus accumbens, NAc; ventral tegmental area, VTA.
The anterior cingulate has also been shown to be a critical brain region for the modulation of the subjective affective experience of pain [73]. Patients who have had a portion of the anterior cingulate surgically removed report that painful stimuli are no longer bothersome, even though they are able to localize pain sensations [77]. These findings support the idea that the distressing affective experience of a physically painful stimulus can be separated from its sensory properties.
Emotional pain also activates brain regions associated with physical pain including the PAG, insula, and anterior cingulate [78]; similarly, physical pain also activates limbic structures including the nucleus accumbens, ventral tegmental area (VTA), amygdala, and habenula [79–81]. Thus, the sensory and emotional components of pain are processed within discreet but interacting brain structures.
While a painful event serves an adaptive function and provides salience to a harmful stimulus that can support escape and avoidance learning, chronic pain can become pathological (serving no useful purpose). Although, it was recently proposed that this type of pain perhaps serves to provide hypervigilance [82]. Chronic pain involves neuroplasticity in the circuitry underlying both the sensory and affective components of pain. Patients with chronic pain suffer from sensory disturbances including allodynia (pain caused by a previously nonpainful stimulus) and hyperalgesia (exaggerated pain response to a previously painful stimulus). However, the negative affective component of chronic pain is argued to be a greater factor in quality of life measures [40].
Separation/Social Distress
Much of the same neurocircuitry described above is also engaged by separation distress, suggesting that the emotional pain elicited by separation distress is a result of the activation of circuits underlying physical pain. Specifically, the separation distress circuitry starts in the PAG and ascends through the dorsomedial thalamus, terminating in various basal forebrain regions including the anterior cingulate cortex [50, 59, 65] (Figure 2). Localized electrical stimulation of the anterior cingulate, dorsomedial thalamus, and PAG provoke separation cries in mammals [83, 84]. In humans, the experience of emotional distress induced by social rejection is associated with an increase in activity in the anterior cingulate cortex measured by fMRI [85]. Together, these studies suggest that psychological pain, particularly social rejection and intense loneliness, may share some of the same neural pathways that elaborate physical pain.
Motivation
Reward and motivation, while often considered opponent processes to pain, are also processed within many of the same brain structures, in particular the mesolimbic system, which includes the VTA and nucleus accumbens (Figure 2). In neuropathic pain animals, functional connectivity is altered within the limbic system (including the nucleus accumbens) as well as between the limbic and nociceptive systems (including the thalamus, primary sensory cortices, insula, and PAG) [86]. In human clinical pain cohorts, connectivity is altered between the mesolimbic system and cortical structures [87–89]. Given that the mesolimbic system is responsible for the modulation of motivated behaviors and reinforcement learning [90, 91], altered activity in this system likely contributes to the negative affective component of pain. Pain can also directly impair general reward processing, leading to an anhedonic state [42]. Dopamine is a critical neurotransmitter within the mesolimbic system, and dopamine signaling in the nucleus accumbens may modulate the salience of painful experiences. While acute pain activates dopaminergic transmission to the nucleus accumbens [81, 92], chronic pain produces the opposite effect [93–95].
Together, the circuitry underlying pain, separation distress, and motivation provides a neuroanatomical substrate for the transition from physical or emotional pain to suicidality and possibly depression. Activity in pain/nociceptive circuitry (including the anterior cingulate, dorsomedial thalamus, and PAG) is correlated with the distress PANIC/GRIEF system, while activity in the mesolimbic circuit, particularly dopamine transmission in the nucleus accumbens, is correlated with the SEEKING system [50, 60, 66]. Sustained activity in the pain circuitry can reduce activity in the motivational circuitry through modulation of mesolimbic dopamine signaling, such that the distress caused by prolonged pain (sensory or emotional) may ultimately lead to decreased processing of rewarding stimuli. These neural substrates are further linked through shared activation by the opioid system, discussed in more detail below.
The Opioid System
Receptors and Endogenous Ligands
The opioid system, which modulates pain, social distress, and reward circuitry, may be a promising target for the treatment of behavioral disorders caused by disruptions in this circuitry, including suicidal ideation. Opioid receptors belong to the G-protein coupled receptor family and are divided into four families: the mu (MOR), delta (DOR), kappa (KOR) and nociceptin (NOR). These receptors are activated by four classes of endogenous opioid peptides, beta-endorphin, dynorphin, enkephalin and nociceptin. MORs have a high affinity for beta-endorphin and enkephalins, but low affinity for dynorphin. Conversely, dynorphin primarily acts through the KOR. Here we focus on the role of the MOR and, particularly, the KOR, as both have been implicated in the mediation of suicidal ideation by opioid drugs.
Opioid receptors are distributed throughout the central and peripheral nervous system and are present in many of the major structures involved in the pain circuitry, including the peripheral nociceptors, spinal cord, PAG, thalamus, anterior cingulate cortex, and other limbic regions [96]. The MOR is widely distributed throughout the brainstem, midbrain, and forebrain structures, and mediates the analgesic effects of most clinically available opioid medications, such as morphine [97]. KORs are located throughout the neuroaxis as well, and their localization in the spinal cord and brain stem can produce analgesia through the direct inhibition of pain pathways [98, 99].
While KOR and MOR expression widely overlaps throughout the brain, their activation produces opposing effects on mood [100]. Activation of KORs primarily produces negative emotions and dysphoria [101, 102], including depressive-like and psychotomimetic effects in humans [103–105] and rodents [100, 106–109]. In contrast, activation of the MOR is reinforcing and associated with positive hedonic experiences, Thus, in general, KOR activity is involved in an anti-reward system opposing rewarding MOR activity [110].
Involvement in Pain, Separation/Social Distress, and Reward/Motivation
Opioids and their receptors can modulate both the sensory and emotional (bothersome) components of pain. For example, when injected into the dorsomedial thalamus (a key region for processing both the sensory and affective components of pain), the MOR agonist DAGO elevated rats’ sensory pain thresholds and induced a positive affective state, while the KOR agonist U50,488 reduced rats’ pain thresholds and induced a negative affective state [111]. However, studies have shown sex differences with respect to the functioning of the MOR and KOR systems, particularly with respect to pain and addiction. Several comprehensive reviews are available [112–114].
In addition to their role in the sensory/affective components of pain, it is hypothesized that opioids constitute a major neurochemical underpinning of social bonding and isolation distress [115, 116]. For example, opioid peptides are decreased in the midbrain of rat pups following social isolation [117], and endogenous opioid peptides acting at MORs have been shown in animal models to alleviate distress behaviors following social separation [115]. The MOR agonist morphine decreases distress vocalizations in rat pups isolated from their mother [118, 119], while the KOR agonist U50,488 increases isolation-induced ultrasonic vocalization [118]. Thus, it appears that dynorphins are responsible for mediating negative affect within the neurocircuitry underlying social distress, similar to their role in the modulation of physical pain (Figure 2).
High expression levels of KOR have been also detected in brain areas responsible for reward and motivation, including the VTA and nucleus accumbens [120, 121] (Figure 2). The ability of KOR agonists to negatively modulate mesolimbic dopamine has significant implications for motivated behavior. Since reduced nucleus accumbens dopamine signaling is associated with a loss of motivation, KOR modulation of dopamine circuitry may link the acute distress of physical or emotional pain with the subsequent onset of negative motivational states and affect.
Studies in rat brain slices show that KOR agonists (U69,593) are capable of suppressing mesolimbic dopamine release via receptors expressed on dopamine neuronal terminals as well as neuronal cell bodies [122–125], which may contribute to the dysphoric effects of KOR activation. KOR agonists (including U50,488, spiradoline, U69,593) also inhibit dopamine signaling when applied directly into the nucleus accumbens of rats, as measured by microdialysis in intact animals [126, 127] or by superfused brain slices [128]; however, changes in dopamine signaling in the nucleus accumbens did not correlate with KOR agonist (U50,488) induced conditioned place aversion (CPA) in mice [129]. Furthermore, morphine-evoked increases in extracellular dopamine within the nucleus accumbens were blocked by the administration of a KOR agonist (U50,488) into this brain region in mice [130]. Finally, the expression of KOR-mediated aversion (U69,593-induced CPA) requires the activity of medium spiny neurons expressing dopamine receptors within the nucleus accumbens of rats [131] and mice [132].
Activation of KORs also contributes to the dopamine hypofunction observed in chronic pain states. Given that hypo-dopaminergic states contribute to chronic pain [133, 134] and mood disorders comorbid with chronic pain [135], KOR antagonism to recover dopamine may hold promise as a novel therapeutic for treating chronic pain and associated mood disorders. Indeed, reduced motivation for food (sucrose) reward induced by inflammatory pain was recovered by KOR antagonism (with norBNI) or silencing of dynorphin neurons within the ventral striatum of rats [136]. A comprehensive review of KOR function in chronic pain and its relationship with drug-seeking behavior is available [137].
The role of KORs in dysfunctions of reward and motivation is particularly well-characterized with respect to AUD. KOR-mediated reductions in dopamine release in the nucleus accumbens have been hypothesized to mediate negative emotional states associated with alcohol withdrawal, particularly pain associated with acute alcohol withdrawal [138]. At the preclinical level, alcohol-preferring rats show increased dynorphin mRNA expression in the central amygdala and hypothalamus compared to non-preferring rats after voluntary drinking [139]. The KOR antagonist norBNI also attenuates withdrawal-related anxiety-like behaviors in alcohol-dependent mice [140]. In addition to alleviating alcohol-induced negative affective states, pharmacotherapies with KOR antagonist properties, including buprenorphine, reduce binge-like alcohol drinking [141, 142], alcohol self-administration [143, 144], and block escalation of compulsive-like drinking after dependence induction [145, 146] and stress exposure [147] in rodent.
The ability of opioids to modulate both sensory/affective pain circuits as well as reward/motivation circuits suggests these compounds have the capability to counteract multiple features of suicidality and depression. Opioids are able to produce dopamine-independent positive affective states through their influence on pain and social distress circuits, including areas such as the anterior cingulate cortex, PAG, and dorsomedial thalamus. Opioids can also counteract negative affective states by promoting increased motivational drive through their downstream influence on dopaminergic reward circuits, especially in the nucleus accumbens. Thus, since opioids can restore deficits in both pain and reward circuits, they may be particularly useful in treating suicidal ideation, as they would be able to blunt suicidality whether it was caused primarily by a disruption in dopaminergic motivational circuity or a disruption in non-dopaminergic pain/social distress circuits. Other treatments which primarily target reduced motivation (anhedonia) may not be effective in treating the subset of individuals experiencing suicidal ideation without a concomitant reduction in motivation (i.e., patients with or without comorbid depression).
Buprenorphine Attenuates Suicidal Ideation
Given the above understanding of the opioid system, there has been a renewed interest in the use of opioid analgesics, particularly buprenorphine, for the treatment of suicidality. A retrospective 24-months study reported buprenorphine had the lowest incidence of suicide intent and deaths compared to other opioid analgesics [148]. Buprenorphine has demonstrated rapid antidepressant effects in humans [149–152], including those with treatment-resistant depression, and has shown particular promise in reducing suicidal ideation [153].
Buprenorphine Mechanism
Buprenorphine is an analgesic derived from oripavine that acts as a partial MOR agonist and KOR antagonist, as well as an antagonist at the DOR and an agonist at the NOR [154]. Buprenorphine has similar affinities for the MOR and KOR, but a 10-fold lower affinity for the DOR [154]. For the purposes of this review, we have largely limited our discussion to the MOR agonist and KOR antagonist effects as these are well-characterized, although note that some work has shown that buprenorphine may have partial agonist activity at KORs [155–157]. Importantly, due to its partial MOR agonist properties, buprenorphine has a lower overdose risk compared to full MOR agonists such as morphine [158].
Clinical Studies Demonstrating the Effects of Buprenorphine on Behavior
The potential anti-suicidal effects of buprenorphine were first described in a case report of a 61-year-old woman suffering from treatment-resistant depression, chronic back pain, severe opioid use disorder, and ongoing suicidal ideation [159]. While treatment with buprenorphine (16 mg/4 mg buprenorphine/naloxone) was prescribed to treat the patient’s opioid use disorder, she reported that her suicidal ideation completely disappeared after 1 week of treatment, and suicidal ideation remained absent up to 3 months after the initial treatment. In another case report, a patient with cannabis-induced psychotic disorder and opioid depressive disorder with severe suicidal thoughts was treated successfully with a single high dose (96 mg) of buprenorphine [160]. Another case report showed that buprenorphine/naloxone (8 mg/2 mg) was effective in reducing pain and suicidal ideation in a 39-year-old male with a history of bipolar disorder, multiple suicide attempts, and polysubstance abuse [161]. Chart reviews of suicidal adult depressed patients with comorbid chronic pain and opioid use disorder who received off-label buprenorphine also found some support for the anti-suicidal properties of buprenorphine [162]. The presence of chronic pain, depression, and substance use in these case reports and studies suggests that buprenorphine may effectively mitigate suicidal ideation by targeting multiple overlapping neurocircuits, which underlie these often-comorbid disorders.
Based on these case reports and anecdotal findings, clinical trials have begun to explore the anti-suicidal potential of buprenorphine. A multisite randomized double-blind placebo-controlled trial of ultra-low-dose (initial dosage, 0.1 mg once or twice daily; mean final dosage, 0.44 mg/day) buprenorphine found that severely suicidal patients showed a reduction in Beck Scale for Suicidal Ideation (BSSI) scores after 2 and 4 weeks of treatment compared to patients that received placebo [54]. Another randomized clinical trial tested the efficacy of one of three single high doses of buprenorphine (32, 64, 96 mg) in suicidal opioid-dependent patients [163]. The researchers found that BSSI scores were significantly reduced in patients across all three buprenorphine doses. While these findings suggest that buprenorphine has particular promise as an anti-suicide treatment option, more research is needed to determine the conditions under which buprenorphine treatment is most effective and tolerable, including whether low or high doses are more successful (the wide range of effective doses in these clinical trials - from 0.44 to 96 mg - is interesting and will be an important area for future studies) and whether treatment is affected by comorbidities including substance use disorder or chronic pain.
Other studies have examined the effects of buprenorphine in combination with other drugs. A randomized double-blind placebo-controlled trial in adults with treatment-resistant depression showed that treatment with 2 mg/2 mg buprenorphine/samidorphan significantly improved scores on multiple depression measures compared to placebo controls [164]. Antidepressant activity was also demonstrated in another study using a 1:1 ratio of buprenorphine:samidorphan [165]. Samidorphan is a MOR antagonist, thus this combined treatment leaves the KOR antagonist activity of buprenorphine intact while blocking the MOR agonist activity of buprenorphine. Blocking the subjective and objective MOR effects likely mitigates the potential addictive properties of buprenorphine in opioid-naïve individuals. While these studies did not directly measure suicidal ideation independent of depression, they provide important insight into the potential mechanisms of buprenorphine’s behavioral effects. In both cases, the effects of buprenorphine were not blocked by a MOR antagonist, suggesting that activity at this receptor may not be required for the anti-suicidal effects of buprenorphine.
Preclinical Studies Demonstrating the Effects of Buprenorphine on Behavior
In addition to the clinical findings described above, pre-clinical studies also support the potential anti-suicidal treatment effects of buprenorphine. While no behavioral assays for suicidal ideation exist for rodents, several behavioral assays have been validated to screen for depressive-like behaviors, including the forced swim test and the novelty-induced hypophagia test. The forced swim test is considered a measurement of behavioral despair [166] and is one of the gold-standard screens for depressive behavior as it is reliably reversed by antidepressants [167]. The novelty-induced hypophagia test is a conflict-based behavioral task that assesses the impact of an environmental stressor on animals’ conditioned approach toward a palatable food reward, with longer approach latencies indicating greater depressive or anxious behavior [168]. Treatment with antidepressants or benzodiazepines reduces approach latencies in the novelty-induced hypophagia test [168–170].
In mice, administration of buprenorphine produced significant reductions in forced swim test immobility (at doses ranging from 0.065–2 mg/kg) and reduced approach latencies in the novel environment of the novelty-induced hypophagia test (at a dose of 0.25 mg/kg) [171]. In Wistar Kyoto (WKY) rats, a strain which has an exaggerated depressive phenotype and is resistant to certain antidepressants, buprenorphine (2.25 mg/kg) significantly reduced immobility in the forced swim test [172]. This effect was specific to the WKY strain, suggesting that buprenorphine may be more effective in individuals with certain treatment-resistant depressions. In general, the doses which produced behavioral effects in these preclinical studies were lower than those used in clinical trials; however, one trial showed that an ultra-low dose of buprenorphine (0.44 mg/day, comparable to the preclinical doses) significantly reduced suicidal ideation [54].
The Contribution of Kappa Versus Mu Activity in the Anti-Suicidal Effects of Buprenorphine
A better understanding of the specific pharmacological underpinnings of the anti-suicidal and anti-depressive effects of buprenorphine would be valuable as it could inform the development of even more targeted therapeutics which might avoid side effects, including abuse potential. As discussed previously, buprenorphine is both a partial agonist at the MOR and an antagonist at the KOR, but which receptor type is primarily responsible for the anti-suicidal and anti-depressive effects of the drug is uncertain. A review of preclinical studies can help to shed light on this question. In general, the data are conflicting, and both MOR partial agonist and KOR antagonist activity likely play a role in the anti-suicidal effects of buprenorphine. However, the data supporting the importance of KOR antagonism appear slightly more consistent (discussed in more detail below).
Studies With Buprenorphine
Studies combining buprenorphine with opioid antagonists suggest that the MOR is not necessary for the behavioral effects of buprenorphine. In mice, the anti-depressive effects of buprenorphine described above (reduction in forced swim test immobility and reduced approach latency in the novelty-induced hypophagia test) were maintained when buprenorphine (1 mg/kg) was co-administered with the opioid antagonist naltrexone (1 mg/kg), suggesting that activation of MORs is not necessary for the expression of buprenorphine’s anti-depressive effects [173]. Co-administration of buprenorphine (0.1 mg/kg) with the MOR antagonist samidorphan (0.3 mg/kg) in Wistar Kyoto rats did not alter the drug’s efficacy in the forced swim test [174], again suggesting that activation of MOR is not necessary for the anti-depressive effects of buprenorphine.
The use of selective knockout mice provides evidence that the behavioral effects of buprenorphine may be mediated by both MOR and KOR. In mice with genetic deletion of the MOR (Oprm1−/−) or KOR (Oprk1−/−), buprenorphine (0.25 mg/kg)-induced decreases in latency in the novelty-induced hypophagia test were blocked in Oprm1−/− but not Oprk1−/− mice [175], suggesting that buprenorphine’s activity at MOR, but not KOR, is required for its anti-depressive effects. Consistent with this idea, a mouse model of the A118G polymorphism (associated with less opioid receptor expression and lower signaling efficiency) in the MOR gene (OPRM1) also disrupted the effects of buprenorphine on this behavior [176]. These data are further supported by human studies which have found that the A118G polymorphism was associated with treatment onset suicidal ideation [177] and more severe depression following a recent targeted rejection major life event [178].
In contrast, knockout of the KOR in mice blocked buprenorphine’s reduction of immobility in the forced swim test while knockout of the MOR did not disrupt the behavioral effects of buprenorphine (0.25–0.5 mg/kg) [179], suggesting that buprenorphine’s activity at KOR, but not MOR, is required for its anti-depressive effects. Together, these studies indicate that the role of different opioid receptor types in buprenorphine’s anti-suicidal and anti-depressive effects are likely mediated by multiple factors including behavioral assay, genetic background, and drug dose.
Studies With Other Drugs That Have Kappa and Mu Activity
We can also examine the behavioral effects of other KOR and MOR drugs to further explore the potential role of opioid receptor subtype in the behavioral effects of buprenorphine. Since buprenorphine is an antagonist at the KOR, if activity at this receptor is primarily responsible for the anti-suicidal effects of buprenorphine, we would expect manipulations that increase activity at KOR to be pro-depressive while manipulations that decrease activity at KOR to be anti-depressive (Table 1, dark blue cells). Conversely, buprenorphine is a partial agonist of the MOR, so if activity at this receptor is primarily responsible for the anti-suicidal effects of buprenorphine, we would expect manipulations that increase activity at MOR to be anti-depressive while manipulations that decrease activity at MOR to be pro-depressive (Table 2, yellow cells).
TABLE 1
| Opioid receptor subtype | Experimental manipulation | Behavioral effect | |
|---|---|---|---|
| KOR | ↑,(Up-regulated) | + (pro-depressant) | • U69,593 exacerbated pain-depressed ICSS (r) [106], elevated ICSS threshold (r) [108], depressed nesting behavior (m) [191], and produced place aversion (m, r) [131, 132, 181] • Salvinorin A increased immobility on forced swim (r) [107], elevated ICSS threshold (r) [107], and produced psychomimetic effects (r, h) [195, 196] • Cyclazocine produced dysphoria & psychomimetic effects (h) [197] • U50,488 produced conditioned place aversion (CPA) (m) [109, 129] and CPA was exacerbated in chronic pain animals (m) [182] |
| 0 (no effect) | • Nalfurafine did not alter pain-depressed ICSS (r) [180] | ||
| -(anti-depressant) | • Salvinorin A reduced anhedonia caused by chronic mild stress (CMS) (r) [198] | ||
| ↓,(Down-regulated) | + | ||
| 0 | • norBNI did not alter pain-depressed ICSS (r) [106] or approach latency in the NIH test (m) [175] • JDTic did not alter pain-related depression of nesting behavior (m) [191] |
||
| - | • norBNI reduced immobility on forced swim (m, r) [109, 171, 179, 183–187], reduced aversive behaviors produced by inescapable footshock (m) [109], reduced expression of learned helplessness (r) [199], prevented CPP to gabapentin in a spinal nerve ligation (SNL) injury (r) [200], reduced social impairment produced by heroin abstinence (m) [201], and attenuated cocaine-withdrawal induced increase in ICSS threshold (r) [186]•JDTic reduced immobility on forced swim (r) [187], blocked depression of nesting behavior by KOR agonist (m) [191], and reduced footshock-induced reinstatement of cocaine seeking (r) [187] • MCL-144B reduced immobility on forced swim (m) [188] • KOR knockout mice had disrupted BPN-induced reduction in forced swim immobility (m) [179] and reduced social aversion following heroin abstinence (m) [202] |
Review of evidence supporting the role of KOR in the anti-suicidal effects of buprenorphine. Letters indicate experimental model: (m), mouse; (r), rat; (h), human.
TABLE 2
| Opioid receptor subtype | Experimental manipulation | Behavioral effect | |
|---|---|---|---|
| MOR | ↑ | + | |
| 0 | • Morphine did not alter behavior on forced swim (m) [171], approach latency in NIH test (m) [175], nor the depression of nesting behavior by a KOR agonist (m) [191] | ||
| - | • Morphine reduced learned helplessness (r) [189], decreased immobility on the tail suspension test (m) [190], blocked pain-depressed ICSS (r) [106], and alleviated pain-related depression of nesting behavior (m) [191] • Codeine decreased immobility on tail suspension test (m) [190, 203] • Methadone reduced learned helplessness (r) [204] and decreased immobility on tail suspension test (m) [190] • Tramadol reduced learned helplessness (r) [204] and decreased immobility on tail suspension test (m) [190] • Opiorphin reduced immobility in forced swim (m) [205] |
||
| ↓ | + | • MOR knockout mice had disrupted BPN-induced reduction in latency in the NIH test (m) [175] • Mouse model of the OPRM1 A118G polymorphism had disrupted BPN-induced reduction in latency in NIH test (m) [176] • OPRM1 A118G polymorphism associated with suicidal ideation (h) [177] and more severe depression (h) [178] |
|
| 0 | |||
| - | • Cyprodime reduced approach latency in NIH test (m) [175] • MOR knockout mice had reduced immobility in forced swim (m) [192] and showed reduced anxiogenic and depressive-like responses (m) [193] |
Review of evidence supporting the role of MOR in the anti-suicidal effects of buprenorphine. Letters indicate experimental model: (m), mouse; (r), rat; (h), human.
Kappa Agonists
In general, KOR agonists produce behaviors indicative of depressed mood or dysphoria. An increase in intra-cranial self-stimulation (ICSS) threshold is a commonly used measure of dysphoria in rodents, and the KOR agonists U69,593 108 and salvinorin A [107] have been shown to increase ICSS thresholds in rats; however, another KOR agonist nalfurafine had no effect on this behavior [180]. Note that this effect could be due to the sedative effects of U69,593; however, U69,593 also produced a conditioned place aversion (CPA) in mice [132] and rats [131, 181], an effect consistent with the induction of a negative affective state. The KOR agonist U50,488 also induced a CPA [109], a behavior that we recently showed was exacerbated in chronic pain animals [182]. Given that the vast majority of preclinical studies find that KOR agonism produces depressive-like behaviors (see Table 1), there is strong support for the hypothesis that decreased activity at this receptor underlies the anti-depressant and anti-suicidal properties of buprenorphine.
Kappa Antagonists
Conversely, KOR antagonists tend to have the opposite effect, producing antidepressant effects in multiple behavioral assays. In particular, a number of studies indicate that KOR antagonists, including norBNI [109, 171, 179, 183–187], JDTic [187], and MCL-144B [188], reduce immobility on the forced swim test in rats and mice. Numerous studies support the anti-depressive effects of KOR anatgonists, particularly norBNI and JDTic (see Table 1), further supporting the role of KOR antagonism in the behavioral effects of buprenorphine.
Mu Agonists
MOR agonists have been shown to produce antidepressant-like effects, though their efficacy depends on the particular behavioral assay employed (see Table 2). For example, the MOR agonist morphine produced antidepressant-like effects in the learned helplessness model [189] and the tail suspension test [190], but did not have an effect in the forced swim test [171] or in the novelty-induced hypophagia test [175]. Morphine was effective at recovering pain-reduced behaviors including a pain-induced reduction in ICSS responding (increased ICSS threshold) [106] and pain-reduced nesting behavior [191] (although it did not block reduced nesting behavior caused by the KOR agonist U69,593) [191].
Mu Antagonists
The effects of MOR antagonism on depressive-like behaviors are less conclusive (see Table 2). The selective MOR antagonist cyprodime reduced approach latencies in the novelty induced hypophagia test in mice [175], an antidepressant-like effect which is inconsistent with the hypothesis that a decrease in activity at the MOR should promote depressive behaviors. Furthermore, MOR knockout mice have shown reduced immobility in the forced swim test [192] and reduced anxiogenic and depressive-like responses [193]. These data suggest that activity specifically at the MOR is less likely to underlie the anti-suicidal and antidepressant properties of buprenorphine, since either increases or decreases in activity at the MOR are capable of producing antidepressant behaviors.
Overall, it appears that the evidence for MOR activation underlying buprenorphine’s anti-suicidal effects is less convincing than the evidence for KOR antagonism underlying these effects. This conclusion is based primarily on: 1) the inability of MOR antagonists to block the anti-depressive and anti-suicidal effects of buprenorphine in humans [159, 164, 165] and 2) rodents [173, 174], and 3) the anti-depressive effects of some manipulations which decrease MOR activity [175, 192, 193].
Conclusion
This review has summarized the human and preclinical studies that support further investigation of the potential of buprenorphine treatment for reducing suicidal ideation. The unique pharmacology of buprenorphine that includes partial MOR agonism and KOR antagonism likely contributes to its potential therapeutic effects, where there is strong support for KOR antagonism in alleviating anhedonia and depression. Given the high rate of suicidal ideation and death by suicide in both chronic pain and substance use disorder patients, further research should focus on the development of novel KOR antagonists that do not possess the potential for abuse. Buprenorphine is a potent opioid analgesic (more potent than morphine), and while it is an effective treatment for opioid use disorder, it can be used illicitly where there is evidence of misuse, abuse and diversion [194]. Thus, it is important to understand if drugs which combine buprenorphine with a MOR antagonist (such as naloxone; including drugs like Suboxone®) have anti-suicide properties similar to buprenorphine itself. Overall, buprenorphine and KOR drugs have great potential for the treatment of suicidal behavior and future study may lead to safer and more effective pharmacotherapies.
Statements
Author contributions
All authors contributed to various aspects of the writing of the paper. CoMC edited and finalized the paper.
Funding
The Shirley Hatos Foundation supported CaMC and CoMC. NIH Grant numbers R01DA041781 (CaMC), 1UG3TR003148-01 (CaMC) and 2P50 DA005010 (CaMC), and the Department of Defense Grant number W81XWH-15-1-0435 (CaMC).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Hawton K van Heeringen K Suicide. The Lancet373, 1372–81. (2009). 10.1016/s0140-6736(09)60372-x
2.
National Institutes of Health, N. I. of M. H. U. S. D. of H. HS Suicide . Available at: https://www.nimh.nih.gov/health/statistics/suicide.shtml.
3.
The Surgeon General’s Call to Action to Implement the National Strategy for Suicide Prevention . Available at: https://www.hhs.gov/sites/default/files/sprc-call-to-action.pdf (2021).
4.
Asmundson GJG Katz J . Understanding the Co‐occurrence of Anxiety Disorders and Chronic Pain: State‐of‐the‐art. Depress Anxiety26, 888–901. (2009). 10.1002/da.20600
5.
Elman I Borsook D Volkow ND . Pain and Suicidality: Insights from Reward and Addiction Neuroscience. Prog Neurobiol109, 1–27. (2013). 10.1016/j.pneurobio.2013.06.003
6.
Parra-Uribe I Blasco-Fontecilla H Garcia-Parés G Martínez-Naval L Valero-Coppin O Cebrià-Meca A et al Risk of Re-attempts and Suicide Death after a Suicide Attempt: A Survival Analysis. BMC Psychiatry17, 163 (2017). 10.1186/s12888-017-1317-z
7.
Niederkrotenthaler T Gunnell D Arensman E Pirkis J Appleby L Hawton K et al Suicide Research, Prevention, and COVID-19. Crisis vol. 41, 321–30. (2020). 10.1027/0227-5910/a000731
8.
Gunnell D Appleby L Arensman E Hawton K John A Kapur N et al Suicide Risk and Prevention during the COVID-19 Pandemic. Lancet Psychiatry7, 468–71. (2020). 10.1016/S2215-0366(20)30171-1
9.
Czeisler MÉ Lane RI Petrosky E Wiley JF Christensen A Njai R et al Mental Health, Substance Use, and Suicidal Ideation during the COVID-19 Pandemic - United States, June 24-30, 2020, MMWR Morb Mortal Wkly Rep69, 1049–57. (2020). 10.15585/mmwr.mm6932a1
10.
Pirkis J John A Shin S DelPozo-Banos M Arya V Analuisa-Aguilar P et al Suicide Trends in the Early Months of the COVID-19 Pandemic: an Interrupted Time-Series Analysis of Preliminary Data from 21 Countries. The Lancet Psychiatry8(7):579–88.(2021) 10.1016/S2215-0366(21)00091-2
11.
Mann JJ Currier D in Suicide Prevention Insights from Neurobiology of Suicidal Behavior. in The Neurobiological Basis of Suicide (In: D Y., editor) (CRC Press/Taylor & Francis, 2012).
12.
Ballard ED Ionescu DF Vande Voort JL Niciu MJ Richards EM Luckenbaugh DA et al Improvement in Suicidal Ideation after Ketamine Infusion: Relationship to Reductions in Depression and Anxiety. J Psychiatr Res58, 161–6. (2014). 10.1016/j.jpsychires.2014.07.027
13.
Bohnert KM Ilgen MA Louzon S McCarthy JF Katz IR . Substance Use Disorders and the Risk of Suicide Mortality Among Men and Women in the US Veterans Health Administration. Addiction112, 1193–201. (2017). 10.1111/add.13774
14.
Czeisler MÉ Lane RI Petrosky E Wiley JF Christensen A Njai R et al Mental Health, Substance Use, and Suicidal Ideation during the COVID-19 Pandemic - United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep vol. 69, 1049, 57. (2020). 10.15585/mmwr.mm6932a1
15.
Wilcox HC Conner KR Caine ED . Association of Alcohol and Drug Use Disorders and Completed Suicide: an Empirical Review of Cohort Studies. Drug Alcohol Depend76 Suppl, S11, 9. (2004). 10.1016/j.drugalcdep.2004.08.003
16.
Oquendo MA Volkow ND . Suicide: A Silent Contributor to Opioid-Overdose Deaths. N Engl J Med378, 1567–9. (2018). 10.1056/nejmp1801417
17.
Abreu LN Oquendo MA Galfavy H Burke A Grunebaum MF Sher L et al Are Comorbid Anxiety Disorders a Risk Factor for Suicide Attempts in Patients with Mood Disorders? A Two-Year Prospective Study. Eur Psychiatry47, 19, 24., (2017). 10.1016/j.eurpsy.2017.09.005
18.
Soloff PH Lynch KG Kelly TM Malone KM Mann JJ . Characteristics of Suicide Attempts of Patients with Major Depressive Episode and Borderline Personality Disorder: a Comparative Study. Am J Psychiatry157, 601–8. (2000). 10.1176/appi.ajp.157.4.601
19.
Ertl A Sheats KJ Petrosky E Betz CJ Yuan K Fowler KA . Surveillance for Violent Deaths - National Violent Death Reporting System, 32 States, 2016, MMWR Surveill Summ. 68, 1–36. (2019). 10.15585/mmwr.ss.6809a1
20.
Conner A Azrael D Miller M . Suicide Case-Fatality Rates in the United States, 2007 to 2014. Ann Intern Med171, 885–95. (2019). 10.7326/m19-1324
21.
Darvishi N Farhadi M Haghtalab T Poorolajal J . Alcohol-related Risk of Suicidal Ideation, Suicide Attempt, and Completed Suicide: a Meta-Analysis. PloS one10, e0126870 (2015). 10.1371/journal.pone.0126870
22.
Cavanagh JTO Carson AJ Sharpe M Lawrie SM . Psychological Autopsy Studies of Suicide: a Systematic Review. Psychol Med33, 395–405. (2003). 10.1017/s0033291702006943
23.
Fishbain DA . The Association of Chronic Pain and Suicide. in Seminars in Clinical Neuropsychiatry vol. 4 221–7. (1999).
24.
Ilgen MA Zivin K Austin KL Bohnert AS Czyz EK Valenstein M et al Severe Pain Predicts Greater Likelihood of Subsequent Suicide. Suicide Life-Threatening Behav40, 597–608. (2010). 10.1521/suli.2010.40.6.597
25.
Ratcliffe GE Enns MW Belik S-L Sareen J . Chronic Pain Conditions and Suicidal Ideation and Suicide Attempts: an Epidemiologic Perspective. The Clin J pain24, 204–10. (2008). 10.1097/ajp.0b013e31815ca2a3
26.
Tang NKY Crane C . Suicidality in Chronic Pain: a Review of the Prevalence, Risk Factors and Psychological Links. Psychol Med36, 575 (2006). 10.1017/s0033291705006859
27.
Edwards RR Smith MT Kudel I Haythornthwaite J . Pain-related Catastrophizing as a Risk Factor for Suicidal Ideation in Chronic Pain. Pain126, 272–9. (2006). 10.1016/j.pain.2006.07.004
28.
Fisher BJ Haythornthwaite JA Heinberg LJ Clark M Reed J . Suicidal Intent in Patients with Chronic Pain. Pain89, 199–206. (2001). 10.1016/s0304-3959(00)00363-8
29.
Smith MT Edwards RR Robinson RC Dworkin RH . Suicidal Ideation, Plans, and Attempts in Chronic Pain Patients: Factors Associated with Increased Risk. Pain111, 201–8. (2004). 10.1016/j.pain.2004.06.016
30.
Blackburn‐Munro G Blackburn‐Munro RE . Chronic Pain, Chronic Stress and Depression: Coincidence or Consequence?J neuroendocrinology13, 1009–23. (2001). 10.1046/j.0007-1331.2001.00727.x
31.
Fishbain DA Cutler R Rosomoff HL Rosomoff RS . Chronic Pain-Associated Depression: Antecedent or Consequence of Chronic Pain? A Review. Clin J pain13, 116–37. (1997). 10.1097/00002508-199706000-00006
32.
Conejero I Olié E Calati R Ducasse D Courtet P . Psychological Pain, Depression, and Suicide: Recent Evidences and Future Directions. Curr Psychiatry Rep20, 33 (2018). 10.1007/s11920-018-0893-z
33.
Meerwijk EL Weiss SJ . Tolerance for Psychological Pain and Capability for Suicide: Contributions to Suicidal Ideation and Behavior. Psychiatry Res262, 203–8. (2018). 10.1016/j.psychres.2018.02.005
34.
Calati R Laglaoui Bakhiyi C Artero S Ilgen M Courtet P . The Impact of Physical Pain on Suicidal Thoughts and Behaviors: Meta-Analyses. J Psychiatr Res71, 16–32. (2015). 10.1016/j.jpsychires.2015.09.004
35.
Tang NKY Beckwith P Ashworth P . Mental Defeat Is Associated with Suicide Intent in Patients with Chronic Pain. Clin J pain32, 411–9. (2016). 10.1097/ajp.0000000000000276
36.
Winsper C Tang NKY . Linkages between Insomnia and Suicidality: Prospective Associations, High-Risk Subgroups and Possible Psychological Mechanisms. Int Rev Psychiatry26, 189–204. (2014). 10.3109/09540261.2014.881330
37.
Brown LA Lynch KG Cheatle M . Pain Catastrophizing as a Predictor of Suicidal Ideation in Chronic Pain Patients with an Opiate Prescription. Psychiatry Res286, 112893 (2020). 10.1016/j.psychres.2020.112893
38.
Calandre EP Navajas-Rojas MA Ballesteros J Garcia-Carrillo J Garcia-Leiva JM Rico-Villademoros F . Suicidal Ideation in Patients with Fibromyalgia: a Cross-Sectional Study. Pain Pract15, 168–74. (2015). 10.1111/papr.12164
39.
Cahill CM Taylor AMW Cook C Ong E Morón JA Evans CJ . Does the Kappa Opioid Receptor System Contribute to Pain Aversion?Front Pharmacol5, 253 (2014). 10.3389/fphar.2014.00253
40.
Cahill CM Taylor AM . Neuroinflammation-a Co-occurring Phenomenon Linking Chronic Pain and Opioid Dependence. Curr Opin Behav Sci13, 171–7. (2017). 10.1016/j.cobeha.2016.12.003
41.
Elman I Borsook D Volkow ND . Pain and Suicidality: Insights from Reward and Addiction Neuroscience. Prog Neurobiol109, 1–27. (2013). 10.1016/j.pneurobio.2013.06.003
42.
Nicholson B Verma S . Comorbidities in Chronic Neuropathic Pain. Pain Med5 Suppl 1, S9 (2004). 10.1111/j.1526-4637.2004.04019.x
43.
Mee S Bunney BG Reist C Potkin SG Bunney WE . Psychological Pain: a Review of Evidence. J Psychiatr Res40, 680–90. (2006). 10.1016/j.jpsychires.2006.03.003
44.
Troister T Holden RR . Comparing Psychache, Depression, and Hopelessness in Their Associations with Suicidality: A Test of Shneidman's Theory of Suicide. Personal Individual Differences49, 689–93. (2010). 10.1016/j.paid.2010.06.006
45.
Conner KR Ilgen MA . Substance Use Disorders and Suicidal Behavior. Int Handbook Suicide Prev in editors O’Connor R, Platt S, Gordon J, 110–23. (2016) 10.1002/9781118903223.ch6
46.
Edwards S Vendruscolo LF Gilpin NW Wojnar M Witkiewitz K . Alcohol and Pain: A Translational Review of Preclinical and Clinical Findings to Inform Future Treatment Strategies. Alcohol Clin Exp Res44, 368–83. (2020). 10.1111/acer.14260
47.
Zale EL Maisto SA Ditre JW . Interrelations between Pain and Alcohol: An Integrative Review. Clin Psychol Rev37, 57–71. (2015). 10.1016/j.cpr.2015.02.005
48.
Nieto SJ Green R Grodin EN Cahill CM Ray LA . Pain Catastrophizing Predicts Alcohol Craving in Heavy Drinkers Independent of Pain Intensity. Drug and Alcohol Dependence218, 108368 (2021). 10.1016/j.drugalcdep.2020.108368
49.
Panksepp J Biven L The Archaeology of Mind: Neuroevolutionary Origins of Human Emotions (Norton Series on Interpersonal Neurobiology). (WW Norton & Company, 2012).
50.
Panksepp J Watt D . Why Does Depression Hurt? Ancestral Primary-Process Separation-Distress (PANIC/GRIEF) and Diminished Brain Reward (SEEKING) Processes in the Genesis of Depressive Affect. Psychiatry Interpersonal Biol Process74, 5–13. (2011). 10.1521/psyc.2011.74.1.5
51.
Panksepp J Herman B Conner R Bishop P Scott JP . The Biology of Social Attachments: Opiates Alleviate Separation Distress. Biol Psychiatry13, 607–18. (1978).
52.
Herman BH Panksepp J . Effects of Morphine and Naloxone on Separation Distress and Approach Attachment: Evidence for Opiate Mediation of Social Affect. Pharmacol Biochem Behav9, 213–20. (1978). 10.1016/0091-3057(78)90167-3
53.
Kalin NH Shelton SE Barksdale CM . Opiate Modulation of Separation-Induced Distress in Non-human Primates. Brain Res440, 285–92. (1988). 10.1016/0006-8993(88)90997-3
54.
Yovell Y Bar G Mashiah M Baruch Y Briskman I Asherov J et al Ultra-Low-Dose Buprenorphine as a Time-Limited Treatment for Severe Suicidal Ideation: A Randomized Controlled Trial. Am J Psychiatry. 173, 491–8. (2015). 10.1176/appi.ajp.2015.15040535
55.
Karp JF Butters MA Begley AE et al Safety, Tolerability, and Clinical Effect of Low-Dose Buprenorphine for Treatment-Resistant Depression in Midlife and Older Adults. J Clin Psychiatry75, e785–e793. (2014). 10.4088/jcp.13m08725
56.
Richards BM . Suicide and Internalised Relationships: A Study from the Perspective of Psychotherapists Working with Suicidal Patients. Br J Guidance Counselling27, 85–98. (1999). 10.1080/03069889908259717
57.
Gunderson JG . Borderline Patient’s Intolerance of Aloneness: Insecure Attachments and Therapist Availability. Am J Psychiatry (1996).
58.
Cardish RJ . Psychopharmacologic Management of Suicidality in Personality Disorders. Can J Psychiatry52, 115S (2007).
59.
Panksepp J . Feeling the Pain of Social Loss. Science302, 237–9. (2003). 10.1126/science.1091062
60.
Zellner MR Watt DF Solms M Panksepp J . Affective Neuroscientific and Neuropsychoanalytic Approaches to Two Intractable Psychiatric Problems: Why Depression Feels So Bad and what Addicts Really Want. Neurosci Biobehavioral Rev35, 2000–8 (2011). 10.1016/j.neubiorev.2011.01.003
61.
Amini-Khoei H Amiri S Mohammadi-Asl S Alijanpour S Poursaman S Haj-Mirzaian A et al Experiencing Neonatal Maternal Separation Increased Pain Sensitivity in Adult Male Mice: Involvement of Oxytocinergic System. Neuropeptides61, 77–85. (2017). 10.1016/j.npep.2016.11.005
62.
Mizoguchi H Fukumoto K Sakamoto G Jin S Toyama A Wang T et al Maternal Separation as a Risk Factor for Aggravation of Neuropathic Pain in Later Life in Mice. Behav Brain Res359, 942–9. (2019). 10.1016/j.bbr.2018.06.015
63.
Burke NN Finn DP McGuire BE Roche M . Psychological Stress in Early Life as a Predisposing Factor for the Development of Chronic Pain: Clinical and Preclinical Evidence and Neurobiological Mechanisms. J Neurosci Res95, 1257–70. (2017). 10.1002/jnr.23802
64.
Evans S Moloney C Seidman LC Zeltzer LK Tsao JCI . Parental Bonding in Adolescents with and without Chronic Pain. J Pediatr Psychol43, 276–84. (2018). 10.1093/jpepsy/jsx110
65.
Eisenberger N . The Pain of Social Disconnection: Examining the Shared Neural Underpinnings of Physical and Social Pain. Nat Rev Neurosci13, 421–34. (2012). 10.1038/nrn3231
66.
Watt DF Panksepp J . Depression: An Evolutionarily Conserved Mechanism to Terminate Separation Distress? A Review of Aminergic, Peptidergic, and Neural Network Perspectives. Neuropsychoanalysis11, 7–51. (2009). 10.1080/15294145.2009.10773593
67.
Eisenberger NI . The Neural Bases of Social Pain: Evidence for Shared Representations with Physical Pain. Psychosomatic Med74, 126 (2012). 10.1097/psy.0b013e3182464dd1
68.
Kross E Berman MG Mischel W Smith EE Wager TD . Social Rejection Shares Somatosensory Representations with Physical Pain. Proc Natl Acad Sci108, 6270–5. (2011). 10.1073/pnas.1102693108
69.
Todd AJ . Neuronal Circuitry for Pain Processing in the Dorsal Horn. Nat Rev Neurosci11, 823–36. (2010). 10.1038/nrn2947
70.
Wercberger R Basbaum AI . Spinal Cord Projection Neurons: a Superficial, and Also Deep, Analysis. Curr Opin Physiol11, 109–15. (2019). 10.1016/j.cophys.2019.10.002
71.
Millan MJ . Descending Control of Pain. Prog Neurobiol66, 355–474. (2002). 10.1016/s0301-0082(02)00009-6
72.
Treede R-D Kenshalo DR Gracely RH Jones AKP . The Cortical Representation of Pain. PAIN79, (1999). 10.1016/s0304-3959(98)00184-5
73.
Price DD . Psychological and Neural Mechanisms of the Affective Dimension of Pain. Science288, 1769–72. (2000). 10.1126/science.288.5472.1769
74.
Lumley MA Cohen JL Borszcz GS Cano A Radcliffe AA Porter LS et al Pain and Emotion: a Biopsychosocial Review of Recent Research. J Clin Psychol67, 942–68. (2011). 10.1002/jclp.20816
75.
Spike RC Puskár Z Andrew D Todd AJ . A Quantitative and Morphological Study of Projection Neurons in Lamina I of the Rat Lumbar Spinal Cord. Eur J Neurosci18, 2433–48. (2003). 10.1046/j.1460-9568.2003.02981.x
76.
Polgár E Wright LL Todd AJ . A Quantitative Study of Brainstem Projections from Lamina I Neurons in the Cervical and Lumbar Enlargement of the Rat. Brain Res1308, 58–67. (2010). 10.1016/j.brainres.2009.10.041
77.
Sharim J Pouratian N . Anterior Cingulotomy for the Treatment of Chronic Intractable Pain: A Systematic Review. Pain physician19, 537–50. (2016).
78.
O’Connor M-F Wellisch DK Stanton AL Eisenberger NI Irwin MR Lieberman MD et al Craving Love? Enduring Grief Activates Brain’s Reward center. Neuroimage42, 969–72. (2008). 10.1016/s0750-7658(08)00619-9
79.
Berridge KC. Pleasures of the Brain. Brain Cogn52, 106–28. (2003). 10.1016/s0278-2626(03)00014-9
80.
Borsook D Becerra L Carlezon WA Shaw M Renshaw P Elman I et al Reward-aversion Circuitry in Analgesia and Pain: Implications for Psychiatric Disorders. Eur J pain11, 7–20. (2007). 10.1016/j.ejpain.2005.12.005
81.
Scott DJ Heitzeg MM Koeppe RA Stohler CS Zubieta J-K . Variations in the Human Pain Stress Experience Mediated by Ventral and Dorsal Basal Ganglia Dopamine Activity. J neuroscience : official J Soc Neurosci26, 10789–95. (2006). 10.1523/jneurosci.2577-06.2006
82.
Lister KC Bouchard SM Markova T Aternali A Denecli P Pimentel SD et al Chronic Pain Produces Hypervigilance to Predator Odor in Mice. Curr Biology : CB vol. 30 R866–R867. (2020). 10.1016/j.cub.2020.06.025
83.
Herman BH Panksepp J . Ascending Endorphin Inhibition of Distress Vocalization. Science211, 1060–2. (1981). 10.1126/science.7466377
84.
Panksepp J Normansell L Herman B Bishop P Loring C . Neural and Neurochemical Control of the Separation Distress Call. in The Physiological Control of Mammalian Vocalization (ed. JDNewman,) (Springer, 1988). 10.1007/978-1-4613-1051-8_15
85.
Eisenberger NI Lieberman MD Williams KD . Does Rejection Hurt? an fMRI Study of Social Exclusion. Science302, 290–2. (2003). 10.1126/science.1089134
86.
Baliki MN Petre B Torbey S Herrmann KM Huang L Schnitzer TJ et al Corticostriatal Functional Connectivity Predicts Transition to Chronic Back Pain. Nat Neurosci15, 1117–9. (2012). 10.1038/nn.3153
87.
Apkarian AV Bushnell MC Treede R-D Zubieta J-K . Human Brain Mechanisms of Pain Perception and Regulation in Health and Disease. Eur J Pain9, 463 (2005). 10.1016/j.ejpain.2004.11.001
88.
Jensen KB Srinivasan P Spaeth R Tan Y Kosek E Petzke F et al Overlapping Structural and Functional Brain Changes in Patients with Long-Term Exposure to Fibromyalgia Pain. Arthritis Rheum65, 3293–303. (2013). 10.1002/art.38170
89.
Ichesco E Schmidt-Wilcke T Bhavsar R Clauw DJ Peltier SJ Kim J et al Altered Resting State Connectivity of the Insular Cortex in Individuals with Fibromyalgia. J pain : official J Am Pain Soc15, 815–26.(2014). 10.1016/j.jpain.2014.04.007
90.
Fields HL Hjelmstad GO Margolis EB Nicola SM . Ventral Tegmental Area Neurons in Learned Appetitive Behavior and Positive Reinforcement. Annu Rev Neurosci30, 289–316. (2007). 10.1146/annurev.neuro.30.051606.094341
91.
Sun W . Dopamine Neurons in the Ventral Tegmental Area: Drug-Induced Synaptic Plasticity and its Role in Relapse to Drug-Seeking Behavior. Curr Drug Abuse Rev vol. 4 270–85. (2011). 10.2174/1874473711104040270
92.
Boutelle MG Zetterström T Pei Q Svensson L Fillenz M . In Vivo neurochemical Effects of Tail Pinch. J Neurosci Methods34, 151–7. (1990). 10.1016/0165-0270(90)90053-i
93.
Wood PB Schweinhardt P Jaeger E Dagher A Hakyemez A Rabiner EA et al Fibromyalgia Patients Show an Abnormal Dopamine Response to Pain. Eur J Neurosci25, 3576–82. (2007). 10.1111/j.1460-9568.2007.05623.x
94.
Geha PY Baliki MN Wang X Harden RN Paice JA Apkarian AV et al Brain Dynamics for Perception of Tactile Allodynia (Touch-induced Pain) in Postherpetic Neuralgia. Pain138, 641–56. (2008). 10.1016/j.pain.2008.02.021
95.
Pais-Vieira M Mendes-Pinto MM Lima D Galhardo V . Cognitive Impairment of Prefrontal-dependent Decision-Making in Rats after the Onset of Chronic Pain. Neuroscience161, 671–9. (2009). 10.1016/j.neuroscience.2009.04.011
96.
Mansour A Khachaturian H Lewis ME Akil H Watson SJ . Anatomy of CNS Opioid Receptors. Trends Neurosciences11, 308–14. (1988). 10.1016/0166-2236(88)90093-8
97.
Kieffer BL Gavériaux-Ruff C . Exploring the Opioid System by Gene Knockout. Prog Neurobiol66, 285–306. (2002). 10.1016/s0301-0082(02)00008-4
98.
Simonin F Gavériaux-Ruff C Befort K Matthes H Lannes B Micheletti G et al Kappa-Opioid Receptor in Humans: cDNA and Genomic Cloning, Chromosomal Assignment, Functional Expression, Pharmacology, and Expression Pattern in the central Nervous System. Proc Natl Acad Sci United States America92, 7006–10. (1995). 10.1073/pnas.92.15.7006
99.
Kolesnikov Y Jain S Wilson R Pasternak GW . Peripheral κ1-opioid Receptor-Mediated Analgesia in Mice. Eur J Pharmacol310, 141–3. (1996). 10.1016/0014-2999(96)00520-1
100.
Lutz P-E Kieffer BL . Opioid Receptors: Distinct Roles in Mood Disorders. Trends Neurosciences36, 195–206. (2013). 10.1016/j.tins.2012.11.002
101.
Darcq E Kieffer BL . Opioid Receptors: Drivers to Addiction?Nat Rev Neurosci19, 499–514. (2018). 10.1038/s41583-018-0028-x
102.
Chavkin C Koob GF . Dynorphin, Dysphoria, and Dependence: the Stress of Addiction. Neuropsychopharmacology : official publication of the American College of Neuropsychopharmacology41, 373–4. (2016). 10.1038/npp.2015.258
103.
Kumor KM Haertzen CA Johnson RE Kocher T Jasinski D . Human Psychopharmacology of Ketocyclazocine as Compared with Cyclazocine, Morphine and Placebo. J Pharmacol Exp Ther238, 960–8. (1986).
104.
Pfeiffer A Brantl V Herz A Emrich HM . Psychotomimesis Mediated by Kappa Opiate Receptors. Science233, 774–6. (1986). 10.1126/science.3016896
105.
Wadenberg M-LG . A Review of the Properties of Spiradoline: a Potent and Selective Kappa-Opioid Receptor Agonist. CNS Drug Rev9, 187–98. (2003). 10.1111/j.1527-3458.2003.tb00248.x
106.
Negus SS Morrissey EM Rosenberg M Cheng K Rice KC . Effects of Kappa Opioids in an Assay of Pain-Depressed Intracranial Self-Stimulation in Rats. Psychopharmacology210, 149–59. (2010). 10.1007/s00213-009-1770-6
107.
Carlezon WA Béguin C DiNieri JA Baumann MA Richards MR Todtenkopf MS et al Depressive-Like Effects of the κ-Opioid Receptor Agonist Salvinorin A on Behavior and Neurochemistry in Rats. J Pharmacol Exp Ther316, 440–7.(2006). 10.1124/jpet.105.092304
108.
Todtenkopf MS Marcus JF Portoghese PS Carlezon WA . Effects of κ-opioid Receptor Ligands on Intracranial Self-Stimulation in Rats. Psychopharmacology172, 463–70. (2004). 10.1007/s00213-003-1680-y
109.
Land BB Bruchas MR Lemos JC Xu M Melief EJ Chavkin C et al The Dysphoric Component of Stress Is Encoded by Activation of the Dynorphin Kappa-Opioid System. J neuroscience : official J Soc Neurosci28, 407–14. (2008). 10.1523/jneurosci.4458-07.2008
110.
Wee S Koob GF . The Role of the Dynorphin–κ Opioid System in the Reinforcing Effects of Drugs of Abuse. Psychopharmacology210, 121–35. (2010). 10.1007/s00213-010-1825-8
111.
Carr KD Bak TH . Medial Thalamic Injection of Opioid Agonists: Mu-Agonist Increases while Kappa-Agonist Decreases Stimulus Thresholds for Pain and Reward. Brain Res441, 173–84. (1988). 10.1016/0006-8993(88)91396-0
112.
Rasakham K Liu-Chen L-Y . Sex Differences in Kappa Opioid Pharmacology. Life Sci88, 2–16. (2011). 10.1016/j.lfs.2010.10.007
113.
Chartoff EH Mavrikaki M . Sex Differences in Kappa Opioid Receptor Function and Their Potential Impact on Addiction. Front Neurosci9, 466 (2015). 10.3389/fnins.2015.00466
114.
Fullerton EF Doyle HH Murphy AZ . Impact of Sex on Pain and Opioid Analgesia: a Review. Curr Opin Behav Sci23, 183–90. (2018). 10.1016/j.cobeha.2018.08.001
115.
Panksepp J Herman BH Vilberg T Bishop P DeEskinazi FG . Endogenous Opioids and Social Behavior. Neurosci Biobehavioral Rev4, 473–87. (1980). 10.1016/0149-7634(80)90036-6
116.
Nelson EE Panksepp J . Brain Substrates of Infant–Mother Attachment: Contributions of Opioids, Oxytocin, and Norepinephrine. Neurosci Biobehavioral Rev22, 437–52. (1998). 10.1016/s0149-7634(97)00052-3
117.
Shoemaker WJ Kehoe P . Effect of Isolation Conditions on Brain Regional Enkephalin And !b-Endorphin Levels and Vocalizations in 10-Day-Old Rat Pups. Behav Neurosci vol. 109117–22. (1995). 10.1037/0735-7044.109.1.117
118.
Kehoe P Boylan CB . Behavioral Effects of Kappa-Opioid-Receptor Stimulation on Neonatal Rats. Behav Neurosci vol. 108418–23. (1994). 10.1037/0735-7044.108.2.418
119.
Kehoe P Blass EM . Opioid-mediation of Separation Distress in 10-Day-Old Rats: Reversal of Stress with Maternal Stimuli. Developmental Psychobiology19, 385–98. (1986). 10.1002/dev.420190410
120.
Peckys D Landwehrmeyer GB . Expression of Mu, Kappa, and delta Opioid Receptor Messenger RNA in the Human CNS: a 33P In Situ Hybridization Study. Neuroscience88, 1093–135. (1999). 10.1016/s0306-4522(98)00251-6
121.
Mansour A Burke S Pavlic RJ Akil H Watson SJ . Immunohistochemical Localization of the Cloned κ1 Receptor in the Rat CNS and Pituitary. Neuroscience71, 671–90. (1996). 10.1016/0306-4522(95)00464-5
122.
Margolis EB Lock H Chefer VI Shippenberg TS Hjelmstad GO Fields HL et al Kappa Opioids Selectively Control Dopaminergic Neurons Projecting to the Prefrontal Cortex. J Neurosci103, 2938–42. (2006). 10.1073/pnas.0511159103
123.
Margolis EB Hjelmstad GO Bonci A Fields HL . Both Kappa and Mu Opioid Agonists Inhibit Glutamatergic Input to Ventral Tegmental Area Neurons. J Neurophysiol93, 3086–93. (2005). 10.1152/jn.00855.2004
124.
Margolis EB Hjelmstad GO Bonci A Fields HL Kappa-opioid Agonists Directly Inhibit Midbrain Dopaminergic Neurons. J neuroscience : official J Soc Neurosci23, 9981–6. (2003). 10.1523/jneurosci.23-31-09981.2003
125.
Ford CP Beckstead MJ Williams JT . Kappa Opioid Inhibition of Somatodendritic Dopamine Inhibitory Postsynaptic Currents. J Neurophysiol97, 883–91. (2007). 10.1152/jn.00963.2006
126.
Donzanti BA Althaus JS Payson MM Von Voigtlander PF . Kappa Agonist-Induced Reduction in Dopamine Release: Site of Action and Tolerance. Res Commun Chem Pathol Pharmacol78, 193–210. (1992).
127.
Spanagel R Herz A Shippenberg TS . Opposing Tonically Active Endogenous Opioid Systems Modulate the Mesolimbic Dopaminergic Pathway. Proc Natl Acad Sci United States America89, 2046–50. (1992). 10.1073/pnas.89.6.2046
128.
Heijna MH Padt M Hogenboom F Portoghese PS Mulder AH Schoffelmeer AN et al Opioid Receptor-Mediated Inhibition of Dopamine and Acetylcholine Release from Slices of Rat Nucleus Accumbens, Olfactory Tubercle and Frontal Cortex. Eur J Pharmacol181, 267–78. (1990). 10.1016/0014-2999(90)90088-n
129.
Ehrich JM Turncliff R Du Y Leigh-Pemberton R Fernandez E Jones R et al Kappa Opioid Receptor-Induced Aversion Requires P38 MAPK Activation in VTA Dopamine Neurons. J neuroscience : official J Soc Neurosci35, 12917–31. (2015). 10.1523/jneurosci.2444-15.2015
130.
Narita M Suzuki T Funada M Misawa M Nagase H . Blockade of the Morphine-Induced Increase in Turnover of Dopamine on the Mesolimbic Dopaminergic System by Kappa-Opioid Receptor Activation in Mice. Life Sci52, 397–404. (1993). 10.1016/0024-3205(93)90153-t
131.
Shippenberg TS Bals-Kubik R Herz A . Examination of the Neurochemical Substrates Mediating the Motivational Effects of Opioids: Role of the Mesolimbic Dopamine System and D-1 vs. D-2 Dopamine Receptors. J Pharmacol Exp Ther265, 53–9. (1993).
132.
Chefer VI Bäckman CM Gigante ED Shippenberg TS . Kappa Opioid Receptors on Dopaminergic Neurons Are Necessary for Kappa-Mediated Place Aversion. Neuropsychopharmacology38, 2623–31. (2013). 10.1038/npp.2013.171
133.
Elman I Borsook D . Common Brain Mechanisms of Chronic Pain and Addiction. Neuron89, 11–36. (2016). 10.1016/j.neuron.2015.11.027
134.
Taylor AMW Becker S Schweinhardt P Cahill C . Mesolimbic Dopamine Signaling in Acute and Chronic Pain: Implications for Motivation, Analgesia, and Addiction. Pain157, 1194–8. (2016). 10.1097/j.pain.0000000000000494
135.
Elman I Borsook D Volkow ND . Pain and Suicidality: Insights from Reward and Addiction Neuroscience. Prog Neurobiol109, 1–27. (2013). 10.1016/j.pneurobio.2013.06.003
136.
Massaly N Copits BA Wilson-Poe AR Hipólito L Markovic T Yoon HJ et al Pain-Induced Negative Affect Is Mediated via Recruitment of the Nucleus Accumbens Kappa Opioid System. Neuron102, 564–73.e6 (2019). 10.1016/j.neuron.2019.02.029
137.
Cahill CM Lueptow L Kim H Shusharla R Bishop A et al Kappa Opioid Signaling at the Crossroads of Chronic Pain and Opioid Addiction. Handbook of Experimental Pharmacology (2021) 10.1007/164_2021_434
138.
Koob GF . Drug Addiction: Hyperkatifeia/Negative Reinforcement as a Framework for Medications Development. Pharmacol Rev73, 163–201. (2021). 10.1124/pharmrev.120.000083
139.
Zhou Y Colombo G Gessa GL Kreek MJ . Effects of Voluntary Alcohol Drinking on Corticotropin-Releasing Factor and Preprodynorphin mRNA Levels in the central Amygdala of Sardinian Alcohol-Preferring Rats. Neurosci Lett554, 110–4. (2013). 10.1016/j.neulet.2013.08.071
140.
Rose JH Karkhanis AN Chen R Gioia D Lopez MF Becker HC et al Supersensitive Kappa Opioid Receptors Promotes Ethanol Withdrawal-Related Behaviors and Reduce Dopamine Signaling in the Nucleus Accumbens. Int J Neuropsychopharmacol19, (2016). 10.1093/ijnp/pyv127
141.
Anderson RI Lopez MF Griffin WC Haun HL Bloodgood DW Pati D et al Dynorphin-kappa Opioid Receptor Activity in the central Amygdala Modulates Binge-like Alcohol Drinking in Mice. Neuropsychopharmacology44, 1084–92. (2019). 10.1038/s41386-018-0294-3
142.
Ciccocioppo R Economidou D Rimondini R Sommer W Massi M Heilig M et al Buprenorphine Reduces Alcohol Drinking through Activation of the Nociceptin/Orphanin FQ-NOP Receptor System. Biol Psychiatry61, 4–12. (2007). 10.1016/j.biopsych.2006.01.006
143.
Schank JR Goldstein AL Rowe KE King CE Marusich JA Wiley JL et al The Kappa Opioid Receptor Antagonist JDTic Attenuates Alcohol Seeking and Withdrawal Anxiety. Addict Biol17, 634–47. (2012). 10.1111/j.1369-1600.2012.00455.x
144.
Walker BM Zorrilla EP Koob GF . Systemic κ-opioid Receptor Antagonism by Nor-Binaltorphimine Reduces Dependence-Induced Excessive Alcohol Self-Administration in Rats. Addict Biol16, 116–9. (2011). 10.1111/j.1369-1600.2010.00226.x
145.
Walker BM Rasmussen DD Raskind MA Koob GF . α1-noradrenergic Receptor Antagonism Blocks Dependence-Induced Increases in Responding for Ethanol. Alcohol42, 91–7. (2008). 10.1016/j.alcohol.2007.12.002
146.
Nealey KA Smith AW Davis SM Smith DG Walker BM . κ-Opioid Receptors Are Implicated in the Increased Potency of Intra-accumbens Nalmefene in Ethanol-dependent Rats. Neuropharmacology61, 35–42. (2011). 10.1016/j.neuropharm.2011.02.012
147.
Domi E Barbier E Augier E Augier G Gehlert D Barchiesi R et al Preclinical Evaluation of the Kappa-Opioid Receptor Antagonist CERC-501 as a Candidate Therapeutic for Alcohol Use Disorders. Neuropsychopharmacology43, 1805–12. (2018). 10.1038/s41386-018-0015-y
148.
Coplan PM Sessler NE Harikrishnan V Singh R Perkel C . Comparison of Abuse, Suspected Suicidal Intent, and Fatalities Related to the 7-day Buprenorphine Transdermal Patch versus Other Opioid Analgesics in the National Poison Data System. Postgrad Med129, 55–61. (2017). 10.1080/00325481.2017.1269596
149.
Bodkin JA Zornberg GL Lukas SE Cole JO . Buprenorphine Treatment of Refractory Depression. J Clin Psychopharmacol15, (1995). 10.1097/00004714-199502000-00008
150.
Emrich HM Vogt P Herz A Kissling W . Antidepressant Effects of Buprenorphine. Lancet2, 709 (1982). 10.1016/s0140-6736(82)90727-9
151.
Thomas R Kosten M Charles Morgan M Therese A Kosten P . Depressive Symptoms during Buprenorphine Treatment of Opioid Abusers. J Substance Abuse Treat7, 51–4. (1990). 10.1016/0740-5472(90)90035-o
152.
Nyhuis PW Gastpar M Norbert S . Opiate Treatment in Depression Refractory to Antidepressants and Electroconvulsive Therapy. J Clin Psychopharmacol28, 593–5. (2008). 10.1097/jcp.0b013e31818638a4
153.
Serafini G Adavastro G Canepa G De Berardis D Valchera A Pompili M et al The Efficacy of Buprenorphine in Major Depression, Treatment-Resistant Depression and Suicidal Behavior: A Systematic Review. Int J Mol Sci19, 2410 (2018). 10.3390/ijms19082410
154.
Lutfy K Cowan A . Buprenorphine: a Unique Drug with Complex Pharmacology. Curr neuropharmacology2, 395–402. (2004). 10.2174/1570159043359477
155.
Huang P Kehner GB Cowan A Liu-Chen LY . Comparison of Pharmacological Activities of Buprenorphine and Norbuprenorphine: Norbuprenorphine Is a Potent Opioid Agonist. J Pharmacol Exp Ther297, 688–95. (2001).
156.
Wentland MP Lou R Lu Q Bu Y VanAlstine MA et al Syntheses and Opioid Receptor Binding Properties of Carboxamido-Substituted Opioids. Bioorg Med Chem Lett19, 203–8. (2009). 10.1016/j.bmcl.2008.10.134
157.
Dunn AD Reed B Erazo J Ben-Ezra A Kreek MJ . Signaling Properties of Structurally Diverse Kappa Opioid Receptor Ligands: Toward In Vitro Models of In Vivo Responses. ACS Chem Neurosci10, 3590–600. (2019). 10.1021/acschemneuro.9b00195
158.
Robinson SE . Buprenorphine: An Analgesic with an Expanding Role in the Treatment of Opioid Addiction. CNS Drug Rev8, 377–90. (2002). 10.1111/j.1527-3458.2002.tb00235.x
159.
Striebel JM Kalapatapu RK . The Anti-suicidal Potential of Buprenorphine: A Case Report. Int J Psychiatry Med47, 169–74. (2014). 10.2190/pm.47.2.g
160.
Ahmadi J . The Effect of Buprenorphine on the Reduction of Cannabis and Heroin Craving and Suicidal Thoughts: a New Finding. Insights Biomed1, 2 (2016).
161.
Benhamou O-M Lynch S Klepacz L . Case Report: Buprenorphine-A Treatment for Psychological Pain and Suicidal Ideation?Am J Addict vol. 30 80–2. (2021). 10.1111/ajad.13063
162.
Gibbs HM Price D Delgado PL Clothier JL Cáceda R . Buprenorphine Use for Pain and Suicidal Ideation in Severely Suicidal Patients. Int J Psychiatry Med (2020) 10.1177/0091217420913396
163.
Ahmadi J Jahromi MS Ehsaei Z . The Effectiveness of Different Singly Administered High Doses of Buprenorphine in Reducing Suicidal Ideation in Acutely Depressed People with Co-morbid Opiate Dependence: a Randomized, Double-Blind, Clinical Trial. Trials19, 462 (2018). 10.1186/s13063-018-2843-9
164.
Fava M Memisoglu A Thase ME Bodkin JA Trivedi MH de Somer M et al Opioid Modulation with Buprenorphine/Samidorphan as Adjunctive Treatment for Inadequate Response to Antidepressants: A Randomized Double-Blind Placebo-Controlled Trial. Am J Psychiatry173, 499–508. (2016). 10.1176/appi.ajp.2015.15070921
165.
Ehrich E Turncliff R Du Y Leigh-Pemberton R Fernandez E Jones R et al Evaluation of Opioid Modulation in Major Depressive Disorder. Neuropsychopharmacology40, 1448–55. (2015). 10.1038/npp.2014.330
166.
Castagné V Moser P Roux S Porsolt RD . Rodent Models of Depression: Forced Swim and Tail Suspension Behavioral Despair Tests in Rats and Mice. Curr Protoc Neurosci55, 8–10. (2011). 10.1002/0471142301.ns0810as55
167.
Porsolt RD le Pichon M Jalfre M . Depression: a New Animal Model Sensitive to Antidepressant Treatments. Nature266, 730–2. (1977). 10.1038/266730a0
168.
Dulawa SC Hen R . Recent Advances in Animal Models of Chronic Antidepressant Effects: the novelty-induced Hypophagia Test. Neurosci Biobehavioral Rev29, 771–83. (2005). 10.1016/j.neubiorev.2005.03.017
169.
Bodnoff SR Suranyi-Cadotte B Quirion R Meaney MJ . A Comparison of the Effects of Diazepam versus Several Typical and Atypical Anti-depressant Drugs in an Animal Model of Anxiety. Psychopharmacology97, 277–9. (1989). 10.1007/bf00442264
170.
Bodnoff SR Suranyi-Cadotte B Aitken DH Quirion R Meaney MJ . The Effects of Chronic Antidepressant Treatment in an Animal Model of Anxiety. Psychopharmacology95, 298–302. (1988). 10.1007/BF00181937
171.
Falcon E Maier K Robinson SA Hill-Smith TE Lucki I . Effects of Buprenorphine on Behavioral Tests for Antidepressant and Anxiolytic Drugs in Mice. Psychopharmacology232, 907–15. (2015). 10.1007/s00213-014-3723-y
172.
Browne CA van Nest DS Lucki I . Antidepressant-like Effects of Buprenorphine in Rats Are Strain Dependent. Behav Brain Res278, 385–92. (2015). 10.1016/j.bbr.2014.10.014
173.
Almatroudi A Husbands SM Bailey CP Bailey SJ . Combined Administration of Buprenorphine and Naltrexone Produces Antidepressant-like Effects in Mice. J Psychopharmacol29, 812–21. (2015). 10.1177/0269881115586937
174.
Smith KL Cunningham JL Eyerman DJ Dean RL Deaver DR Sanchez C et al Opioid System Modulators Buprenorphine and Samidorphan Alter Behavior and Extracellular Neurotransmitter Concentrations in the Wistar Kyoto Rat. Neuropharmacology146, 316–26. (2019). 10.1016/j.neuropharm.2018.11.015
175.
Robinson SA Erickson RL Browne CA Lucki I . A Role for the Mu Opioid Receptor in the Antidepressant Effects of Buprenorphine. Behav Brain Res319, 96–103. (2017). 10.1016/j.bbr.2016.10.050
176.
Browne CA Erickson RL Blendy JA Lucki I . Genetic Variation in the Behavioral Effects of Buprenorphine in Female Mice Derived from a Murine Model of the OPRM1 A118G Polymorphism. Neuropharmacology117, 401–7. (2017). 10.1016/j.neuropharm.2017.02.005
177.
Nobile B Ramoz N Jaussent I Gorwood P Olié E Castroman JL et al Polymorphism A118G of Opioid Receptor Mu 1 (OPRM1) Is Associated with Emergence of Suicidal Ideation at Antidepressant Onset in a Large Naturalistic Cohort of Depressed Outpatients. Scientific Rep9, 2569 (2019). 10.1038/s41598-019-39622-3
178.
Slavich GM Tartter MA Brennan PA Hammen C . Endogenous Opioid System Influences Depressive Reactions to Socially Painful Targeted Rejection Life Events. Psychoneuroendocrinology49, 141–9. (2014). 10.1016/j.psyneuen.2014.07.009
179.
Falcon E Browne CA Leon RM Fleites VC Sweeney R Kirby LG et al Antidepressant-like Effects of Buprenorphine Are Mediated by Kappa Opioid Receptors. Neuropsychopharmacology41, 2344–51. (2016). 10.1038/npp.2016.38
180.
Lazenka ML Moerke MJ Townsend EA Freeman KB Carrol FI Negus SS et al Dissociable Effects of the Kappa Opioid Receptor Agonist Nalfurafine on Pain/itch-Stimulated and Pain/itch-Depressed Behaviors in Male Rats. Psychopharmacology235, 203–13. (2018). 10.1007/s00213-017-4758-7
181.
Tejeda HA Counotte DS Oh E E Ramamoorthy S Schultz-Kuszak KN Bäckman CM et al Prefrontal Cortical Kappa-Opioid Receptor Modulation of Local Neurotransmission and Conditioned Place Aversion. Neuropsychopharmacology38, 1770–9. (2013). 10.1038/npp.2013.76
182.
Liu SS Pickens S Burma NE Ibarra-Lecue I Yang H Xue L et al Kappa Opioid Receptors Drive a Tonic Aversive Component of Chronic Pain. J neuroscience : official J Soc Neurosci39, 4162–78. (2019). 10.1523/jneurosci.0274-19.2019
183.
McLaughlin JP Marton-Popovici M Chavkin C . κ Opioid Receptor Antagonism and Prodynorphin Gene Disruption Block Stress-Induced Behavioral Responses. J Neurosci23, 5674 LP – 5683 (2003). 10.1523/jneurosci.23-13-05674.2003
184.
Mague SD Pliakas AM Tomasiewicz HC Zhang Y Stevens WC Jr Jones RM et al Antidepressant-like Effects of κ-opioid Receptor Antagonists in the Forced Swim Test in Rats. J Pharmacol Exp Ther305, 323–30. (2003). 10.1124/jpet.102.046433
185.
Carr GV Bangasser DA Bethea T Young M Valentino RJ Lucki I et al Antidepressant-like Effects of κ-opioid Receptor Antagonists in Wistar Kyoto Rats. Neuropsychopharmacology35, 752–63. (2010). 10.1038/npp.2009.183
186.
Chartoff E Sawyer A Rachlin A Potter D Pliakas A Carlezon WA et al Blockade of Kappa Opioid Receptors Attenuates the Development of Depressive-like Behaviors Induced by Cocaine Withdrawal in Rats. Neuropharmacology62, 167–76. (2012). 10.1016/j.neuropharm.2011.06.014
187.
Beardsley PM Howard JL Shelton KL Carroll FI . Differential Effects of the Novel Kappa Opioid Receptor Antagonist, JDTic, on Reinstatement of Cocaine-Seeking Induced by Footshock Stressors vs Cocaine Primes and its Antidepressant-like Effects in Rats. Psychopharmacology183, 118 (2005). 10.1007/s00213-005-0167-4
188.
Reindl JD Rowan K Carey AN Peng X Neumeyer JL McLaughlin JP et al Antidepressant-Like Effects of the Novel Kappa Opioid Antagonist MCL-144B in the Forced-Swim Test. Pharmacology81, 229–35. (2008). 10.1159/000112867
189.
Tejedor-Real P Mico JA Maldonado R Roques BP Gibert-Rahola J , J. Implication of Endogenous Opioid System in the Learned Helplessness Model of Depression. Pharmacol Biochem Behav52, 145–52. (1995). 10.1016/0091-3057(95)00067-7
190.
Berrocoso E Ikeda K Sora I Uhl GR Sánchez-Blázquez P Mico JA et al Active Behaviours Produced by Antidepressants and Opioids in the Mouse Tail Suspension Test. Int J Neuropsychopharmacol16, 151–62. (2013). 10.1017/s1461145711001842
191.
Negus SS Neddenriep B Altarifi AA Carroll FI Leitl MD Miller LL et al Effects of Ketoprofen, Morphine, and Kappa Opioids on Pain-Related Depression of Nesting in Mice. Pain156, 1153–60. (2015). 10.1097/j.pain.0000000000000171
192.
Yoo J-H Lee S-Y Loh HH Ho IK Jang C-G . Altered Emotional Behaviors and the Expression of 5-HT1A and M1 Muscarinic Receptors in μ-opioid Receptor Knockout Mice. Synapse54, 72–82. (2004). 10.1002/syn.20067
193.
Filliol D Ghozland S Chluba J Martin M Matthes HW Simonin F et al Mice Deficient for δ- and μ-opioid Receptors Exhibit Opposing Alterations of Emotional Responses. Nat Genet25, 195–200. (2000). 10.1038/76061
194.
Chilcoat HD Amick HR Sherwood MR Dunn KE . Buprenorphine in the United States: Motives for Abuse, Misuse, and Diversion. J substance abuse Treat104, 148–57. (2019). 10.1016/j.jsat.2019.07.005
195.
Taylor GT Manzella F . Kappa Opioids, Salvinorin A and Major Depressive Disorder. Curr Neuropharmacol14, 165–76. (2016). 10.2174/1570159x13666150727220944
196.
Ranganathan M Schnakenberg A Skosnik PD Cohen BM Pittman B Sewell RA et al Dose-related Behavioral, Subjective, Endocrine, and Psychophysiological Effects of Theκopioid Agonist Salvinorin A in Humans. Biol Psychiatry72, 871–9. (2012). 10.1016/j.biopsych.2012.06.012
197.
Pfeiffer A Brantl V Herz A Emrich HM . Psychotomimesis Mediated by Kappa Opiate Receptors. Science233, 774 LP – 776 (1986). 10.1126/science.3016896
198.
Harden MT Smith SE Niehoff JA McCurdy CR Taylor GT . Antidepressive Effects of the κ-opioid Receptor Agonist Salvinorin A in a Rat Model of Anhedonia. Behav Pharmacol23, 710–5. (2012). 10.1097/fbp.0b013e3283586189
199.
Shirayama Y Ishida A Iwata M Hazama GI Kawahara R Duman RS et al Stress Increases Dynorphin Immunoreactivity in Limbic Brain Regions and Dynorphin Antagonism Produces Antidepressant-like Effects. J Neurochem90, 1258–68. (2004). 10.1111/j.1471-4159.2004.02589.x
200.
Navratilova E Ji G Phelps C Qu C Hein M Yakhnitsa V et al Kappa Opioid Signaling in the central Nucleus of the Amygdala Promotes Disinhibition and Aversiveness of Chronic Neuropathic Pain. Pain160, 824–32. (2019). 10.1097/j.pain.0000000000001458
201.
Lalanne L Ayranci G Filliol D Gavériaux-Ruff C Befort K Kieffer BL et al Kappa Opioid Receptor Antagonism and Chronic Antidepressant Treatment Have Beneficial Activities on Social Interactions and Grooming Deficits during Heroin Abstinence. Addict Biol22, 1010–21. (2017). 10.1111/adb.12392
202.
Lutz P-E Ayranci G Chu-Sin-Chung P Matifas A Koebel P Filliol D et al Distinct Mu, Delta, and Kappa Opioid Receptor Mechanisms Underlie Low Sociability and Depressive-laike Behaviors during Heroin Abstinence. Neuropsychopharmacology39, 2694–705. (2014). 10.1038/npp.2014.126
203.
Berrocoso E Mico J-A . Cooperative Opioid and Serotonergic Mechanisms Generate superior Antidepressant-like Effects in a Mice Model of Depression. Int J Neuropsychopharmacol12, 1033–44. (2009). 10.1017/s1461145709000236
204.
Rojas-Corrales MO Berrocoso E Gibert-Rahola J Micó JA . Antidepressant-like Effects of Tramadol and Other central Analgesics with Activity on Monoamines Reuptake, in Helpless Rats. Life Sci72, 143–52. (2002). 10.1016/s0024-3205(02)02220-8
205.
Yang Q-Z Lu SS Tian XZ Yang AM Ge WW Chen Q et al The Antidepressant-like Effect of Human Opiorphin via Opioid-dependent Pathways in Mice. Neurosci Lett489, 131–5. (2011). 10.1016/j.neulet.2010.12.002
206.
Mansour A Khachaturian H Lewis ME Akil H Watson SJ . Autoradiographic Differentiation of Mu, delta, and Kappa Opioid Receptors in the Rat Forebrain and Midbrain. J neuroscience : official J Soc Neurosci7, 2445–64. (1987).
Summary
Keywords
suicide, suicidal ideation, kappa opioid, addiction, pain, opioid use disorder, anhedonia, dysphoria
Citation
Cameron CM, Nieto S, Bosler L, Wong M, Bishop I, Mooney L and Cahill CM (2021) Mechanisms Underlying the Anti-Suicidal Treatment Potential of Buprenorphine. Adv. Drug. Alco. Res. 1:10009. doi: 10.3389/adar.2021.10009
Received
10 May 2021
Accepted
30 June 2021
Published
03 August 2021
Volume
1 - 2021
Edited by
Emmanuel Onaivi, William Paterson University, United States
Reviewed by
Chloe Jordan, McLean Hospital, United States
Lawrence Toll, Florida Atlantic University, United States
Updates
Copyright
© 2021 Cameron, Nieto, Bosler, Wong, Bishop, Mooney and Cahill.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Catherine M. Cahill, cmcahill@ucla.edu
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.