Abstract
The coronavirus (COVID-19) pandemic has been associated with both increased and decreased alcohol use. Authors explored reasons for increased and decreased alcohol use since the COVID-19 lockdown (March 2020) in a sample of help-seeking adults (HSA) participating in a remote-based alcohol reduction text-messaging intervention in the USA. At the time of recruitment, the HSA in this study were interested in reducing rather than stopping their alcohol consumption. An optional self-report questionnaire was completed by 324 participants (mean age 41.6 ± 10.2 years; 71.5% female; 83.9% White) in February 2021. Survey questions assessed sociodemographic factors, social stressors (quarantine conditions, employment status, changes to daily routine), and drinking patterns. Authors fit two ordinal logistic regression models: one for increased drinking and one for decreased drinking, as functions of the potential predictors and control variables. Most participants (n = 281; 87.0%) reported drinking more than usual since COVID-19 lockdown began. The most common self-reported reasons for drinking more were increased stress/anxiety (74.7%), boredom (69.4%), and spending more time at home (65.5%) whereas reasons for drinking less were less socializing (33.7%) and worrying about how alcohol would impact the immune system (31.5%). Identifying as female, severity of changes to daily routine, and increased access to alcohol were significantly associated with drinking more than usual. These data suggest that the general consequences of the pandemic in the general population (e.g., boredom) led to greater alcohol use among help-seeking adults attempting to reduce their drinking. Identifying these factors may help create more targeted interventions during public health crises.
Introduction
Excessive alcohol consumption is associated with various health risks and societal challenges [1, 2]. The health and economic hardships of the COVID-19 pandemic are comparable to or perhaps greater than those of past natural or environmental disasters [3, 4]. Previous literature suggests when individuals experience periods of economic or psychological stress, they may consume more alcohol, resulting in increased symptoms of alcohol abuse and dependence [5–9]. In the winter and spring of 2020, governments across the world declared a state of emergency and took drastic measures (e.g., physical distancing, closing businesses, banning large gatherings, quarantining, etc.) to help mitigate the spread of COVID-19. Past literature would suggest that the contextual changes resulting from the measures taken would suggest an increase in harmful alcohol use. However, the current literature on COVID-19-related drinking patterns remains varied, indicating both increased and decreased alcohol consumption [10–13], or no changes at all [1, 14, 15].
Emerging evidence from national and global surveys conducted during the peak of the pandemic (March 2020) shows increased rates of substance use, specifically alcohol use [16]. Preliminary reports suggest, amid COVID-19, both alcohol sales and consumption have increased [17, 18], potentially in response to the use of alcohol as a coping mechanism for psychological distress [18]. For instance, a recently published study on alcohol consumption during the pandemic in the United States (US) showed that Americans drank about 14% more alcohol in 2020, and in a report of national sales of alcohol, online sales increased 262% in 2020, compared to 2019 [19]. Despite alcohol sales not remaining at these levels, overall data for the week ending on 21 March 2020 indicated that online alcohol sales increased by 234% in the US [19].
Several factors have been posited about the increase in alcohol volume sales. Specifically, individuals may have been stockpiling due to concern over inaccessibility during the pandemic’s early phases, which may have inflated these trends; it is likely that the increase in sales was at least partly related to an increase in consumption. Increased accessibility to alcohol is also a known risk factor for increased alcohol use [20, 21]. The negative impact of the COVID-19 pandemic on financial health and social functioning may have increased levels of psychological distress, social isolation, income insecurity, lack of work boundaries due to working from home, and job loss, contributing to increased alcohol consumption [12, 22–29]. Additional factors associated with increased alcohol consumption during the lockdown period included reduced healthcare access, increased access to alcohol delivery services, parental status (i.e., parent versus non-parent), less social connectedness, and increased levels of depression [28, 30, 31].
Conversely, reduced availability and affordability of alcoholic beverages, lack of social gatherings, whether alcohol was considered an essential item, financial distress, and closure of bars were associated with reduced alcohol consumption [12, 32–34]. These findings suggest that restrictions limiting access to alcohol, particularly outside the home (e.g., social gatherings, bars, happy hour, and pubs) might have led to lower alcohol use in certain populations. Additionally, one study suggests that alcohol consumption during COVID-19 decreased among men, while it remained steady among women [35]. This may have been due to broad gender differences in the relationship between loneliness and alcohol use: For instance, feelings of loneliness experienced early in the pandemic were associated with increased alcohol problems for women and a slow decline in alcohol use over time for men. The varying evidence suggests that the relationship between alcohol consumption and COVID-19 is more nuanced, possibly affecting distinct subpopulations in diverse ways. Some variables have been related to both increased and decreased use. For instance, a plausible rationale may be that some individuals were social drinkers, in which case they would decrease their use. On the other hand, some may prefer to drink alone and so their drinking increased.
In the present study, we sought to examine increases and decreases in alcohol use in help-seeking adults (HSA) with at-risk drinking, who may have viewed the pandemic as an opportunity to reduce their drinking and meet their drinking goals. Specifically, the HAS in this study were looking to reduce their drinking via text messaging intervention, rather than through traditional treatment (i.e., Alcoholics Anonymous, in-patient, outpatient).
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) defines at-risk drinking as drinking above the recommended drinking guidelines (i.e., ≤3 standard drinks in one sitting or ≤7 per week for women, and ≤4 standard drinks in one sitting or ≤14 per week for men) without meeting criteria for more severe alcohol use disorders (AUD). At-risk drinkers are at a higher risk of experiencing negative consequences related to drinking along with the risk of progressing to an AUD [36, 37].
Although research finds that many individuals reported changing their drinking during the pandemic [33, 38, 39], there are currently no published data on the impacts of COVID-19 on alcohol consumption among individuals who were seeking to reduce their drinking prior to the pandemic. The present study explores potential predictors of changes in drinking among HSA participating in an alcohol reduction text-messaging intervention. As COVID-19 continues to evolve, understanding the immediate and long-term impacts of alcohol consumption among vulnerable populations can inform appropriate clinical and policy interventions.
Materials and methods
Procedure
Participants were recruited from our primary study (Muench et al., under revision), a randomized controlled trial of mobile messaging interventions for HSA with at-risk drinking, which recruited prospective participants primarily via social media outlets such as Facebook or online alcohol screening/help-seeking sources such as AlcoholScreening.org. This study was approved by both the Feinstein Institutes for Medical Research and Solutions IRB, and clinical investigations were conducted according to the principles expressed in the Declaration of Helsinki. All participants provided electronic informed consent. To meet the eligibility criteria, participants had to consume at least 13 and 15 standard drinks per week for women and men, respectively, which was later modified to include 9 and 11 standard drinks per week for women and men, respectively. Recruitment commenced in March 2019, prior to the pandemic; however, the vast majority of participants enrolled the following year in March 2020, during the pandemic (n = 671; 92%). For the present study, on 5 February 2021, study staff invited all 731 participants via text message to complete an optional cross-sectional questionnaire about their alcohol use since COVID-19 lockdown began. A total of 403 responses were received. Duplicate entries were discarded (n = 64; keeping the first or most complete response), as well as blank entries (n = 3), and data that could not be linked to a trial participant (n = 12), resulting in a final sample size of 324.
Measures
The questionnaire (11 questions) was administered via REDCap [40], a secure web-based application, and assessed lockdown-related effects and behaviors (compliance with social distancing and changes to employment status, fear of contracting COVID-19, and mental health implications, daily routine, and alcohol supply). We assessed changes in drinking since lockdown began through 4 questions in March of 2020. Sociodemographic data (age, sex, race, marital status, and education level) were collected previously when participants enrolled in the primary study. The questionnaire was open for 7 days, and a reminder text was sent to complete it on 12 February 2021. Participants did not receive compensation for completing the questionnaire.
Questions assessing the impacts of COVID-19 were adapted from The Pandemic Stress Index [41], Coronavirus Impact Scale [42], and COVID-19 Community Response Survey [43]. The Resource Portal created by NIH was utilized to find COVID-19-specific survey tools [44].
Compliance with social distancing was assessed by asking: 1) “Have you practiced social distancing? (i.e., reduced your physical contact with people outside of your home in social, work, or school settings by avoiding large groups and staying 3–6 feet away from other people when out in public)” and 2) “Do you regularly wear a mask when outside of your house or pod*? (*a group of people from different households who agree to social distance from other people but not each other).”
Self-reported changes in drinking since the COVID-19 lockdown began were assessed with the question: “Have you experienced any of the following because of COVID-19 (since COVID-19 lockdown began)?” Respondents selected the frequency at which they “drank more than usual” and “drank less than usual” (very frequently, frequently, occasionally, rarely, never, or prefer not to say). Responses were coded as ordinal variables ranging from 1 (never) to 5 (very frequently). Respondents who indicated they drank more or less than usual also reported their perceived reasons for doing so. Possible reasons for drinking more were: increased stress/anxiety, boredom, spending more time at home, easily becoming a part of the routine, worrying about COVID-19 and/or the future, enjoying drinking more, working additional hours, being dependent on alcohol, and other sources. Possible reasons for drinking less were: decreased stress/anxiety, less socializing, worrying about how alcohol would impact the immune system, worrying about becoming ill from COVID-19, having diagnosed or suspected COVID-19, working additional hours, having financial concerns, enjoying drinking less, and other. Participants could select multiple reasons and were prompted to “select more than one option if it applies.” Question and response options were adapted from the survey that Grossman et al. [24] used in their study. Frequency of alcohol use was also assessed by asking: “Since COVID-19 lockdown began, how often did you usually have any kind of drink containing alcohol? By a drink we mean half an ounce of absolute alcohol (e.g., a 12-ounce can or glass of beer or cooler, a 5-ounce glass of wine, or a drink containing 1 shot of liquor). Choose only one.” with the following answer choices: every day, 5 to 6 times a week, 3 to 4 times a week, twice a week, once a week, 2 to 3 times a month, once a month, 3 to 11 times in the past year, and 1 or 2 times in the past year.
Potential predictors of changes in drinking included lockdown-related (compliance with social distancing and changes to employment status, daily routine, and alcohol supply) and sociodemographic (age, sex, race, marital status, and education level) variables, all self-reported and categorized as shown in Table 1. Authors also included as control variables the number of days each participant had been in the intervention trial, calculated as the difference between their baseline and COVID-19 questionnaire dates, and the type of intervention received as part of the trial.
TABLE 1
| Characteristic | Mean (SD) | OR (95% CI), drank morea | OR (95% CI), drank lessa |
|---|---|---|---|
| Age (N = 308) | 41.6 (10.1) | 1.00 (0.97, 1.02) | 0.98 (0.95, 1.00) |
| N (%) | OR (95% CI), drank morea | OR (95% CI), drank lessa | |
| Sex | |||
| Male | 92 (28.4) | REF | REF |
| Female | 232 (71.6) | 1.21 (0.74, 1.98) | 0.87 (0.53, 1.43) |
| Race | |||
| White | 272 (84.0) | REF | REF |
| Non-whiteb | 52 (16.1) | 0.56 (0.31, 1.04) | 1.28 (0.68, 2.41) |
| Marital status | |||
| Single (never married) | 86 (26.5) | REF | REF |
| Married | 159 (49.1) | 0.64 (0.37, 1.12) | 0.88 (0.51, 1.52) |
| Separated, divorced, or widowed | 79 (24.4) | 0.89 (0.46, 1.73) | 0.93 (0.49, 1.79) |
| Education level | |||
| Associates degree or less | 87 (26.9) | REF | REF |
| Bachelor’s degree or more | 237 (73.2) | 1.24 (0.74, 2.10) | 0.61 (0.36, 1.03) |
| Have you practiced social distancing? | |||
| No, I do not social distance | 42 (13.2) | REF | REF |
| Yes, I have been completely quarantined (alone or with family) | 44 (13.6) | 0.33 (0.14, 0.82) | 1.22 (0.51, 2.91) |
| Yes, I have seen others indoors but not been within about six feet of individuals outside my household | 125 (38.6) | 0.38 (0.18, 0.79) | 1.44 (0.70, 2.94) |
| Yes, I have seen others outdoors but not been within about six feet of individuals outside my household | 112 (34.6) | 0.29 (0.14, 0.63) | 1.46 (0.69, 3.07) |
| Has your employment status been affected by COVID-19? | |||
| No, I am able to work from home | 117 (36.1) | REF | REF |
| No, I was not working before | 21 (6.5) | 1.02 (0.38, 2.76) | 0.62 (0.23, 1.67) |
| No, I am working same as before | 139 (42.9) | 0.76 (0.46, 1.25) | 0.97 (0.59, 1.59) |
| Yes, I am currently unemployed due to COVID | 47 (14.5) | 0.53 (0.26, 1.10) | 0.41 (0.20, 0.84) |
| Have your daily routines changed since COVID lockdown began? | |||
| No, I have had no changes to my routines | 11 (3.4) | REF | REF |
| Yes, I have had mild changes to a few of my routines | 60 (18.5) | 1.91 (0.60, 6.09) | 1.64 (0.50, 5.43) |
| Yes, I have had moderate changes across several of my routines | 123 (38.0) | 3.67 (1.18, 11.37) | 0.94 (0.30, 2.99) |
| Yes, I have had severe changes across most or all of my routines | 130 (40.1) | 7.29 (2.26, 23.50) | 0.88 (0.27, 2.88) |
| Has your access to alcohol been affected by COVID-19? | |||
| No | 166 (51.2) | REF | REF |
| Yes, my supply has increased (i.e., due to buying in bulk) | 126 (38.9) | 4.19 (2.54, 6.91) | 0.41 (0.25, 0.67) |
| Yes, my supply has decreased | 32 (10.0) | 0.15 (0.07, 0.33) | 11.00 (4.85, 25.00) |
Questionnaire responses and their associations with changes in drinking (N = 324).
Estimated using ordinal logistic regression models that included all variables in the table, plus the number of days each participant had been in an intervention trial and type of intervention received.
Includes participants who identified as Asian/Pacific Islander, Black/African American, Mixed, Native American, and Other race.
Bolded values are statistically significant at p < 0.05.
SD, standard deviation; OR, odds ratio; CI, confidence interval; REF, reference group.
Statistical analysis
Questionnaire results were reported using frequencies and percentages for categorical variables and means and standard deviations for continuous variables. To explore independent predictors of changes in drinking since COVID-19 lockdown, authors fit two ordinal logistic regression models: one for increased drinking and one for decreased drinking, as functions of the potential predictors and control variables. Regression coefficients for each potential predictor were exponentiated and presented as odds ratios. Each odds ratio represents the proportional increase in odds of indicating a higher frequency of drinking more or less than usually associated with a one-unit change in the predictor, holding other model variables constant. Missing data was handled using listwise deletion. REDCap version 12.2.10,40) was used for data management and SAS version 9.4 [45] and Stata version 15 [46] for data cleaning and analyses.
Results
Sociodemographic variables
The sample was predominantly female-identifying (71.6%), White (84.0%), and had bachelor’s degrees or higher (some graduate school or a graduate degree; 73.2%). Participants’ average age was 41.6 years (SD = 10.2; range = 21–75). Roughly half (49.1%) of participants were currently married, and the remaining reported being single and never married (25.5%), or divorced, separated, or widowed (24.4%).
COVID-19-related variables
Most participants practiced social distancing (86.8%), remained employed (79.0%, including 36.1% working from home), and experienced changes to their routines (96.6%). Approximately half of the participants (n = 158) reported changes in their supply of alcohol, with 38.9% having increased access and 10.0% having decreased access (Table 1).
Most participants (n = 281) reported drinking more than usual since the COVID-19 lockdown began (22.2% very frequently, 35.8% frequently, 26.9% occasionally, 10.5% rarely, and 4.6% never). The most common self-reported reasons for drinking more were increased stress/anxiety (74.7%), boredom (69.4%), and spending more time at home (65.5%) (Figure 1). Statistically significant predictors of drinking more than usual were not social distancing, experiencing more severe changes to daily routines, and increased access to alcohol (Table 1).
FIGURE 1
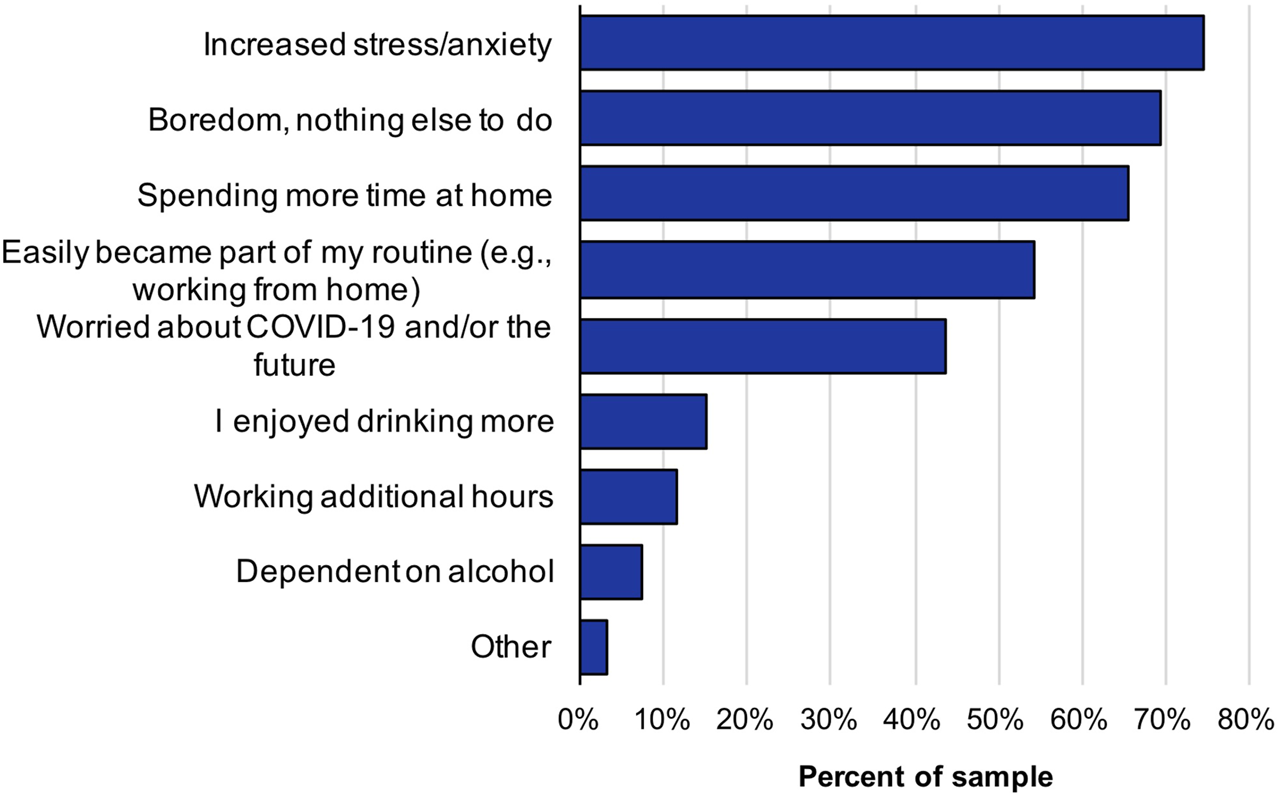
Reasons participants drank more than usual during the COVID-19 pandemic (N = 281).
Fewer participants (n = 89) reported drinking less than usual since COVID-19 lockdown began (3.7% very frequently, 6.5% frequently, 22.8% occasionally, 45.1% rarely, and 21.9% never). The most common self-reported reasons for drinking less were less socializing (33.7%) and worrying about how alcohol would impact the immune system (31.5%) (Figure 2). Additionally, among those who reported drinking less, very few selected working additional hours (3%) and financial concerns (6%) as reasons for lowering their alcohol consumption during COVID-19. Statistically significant predictors of drinking less were continued employment and decreased access to alcohol (Table 1).
FIGURE 2
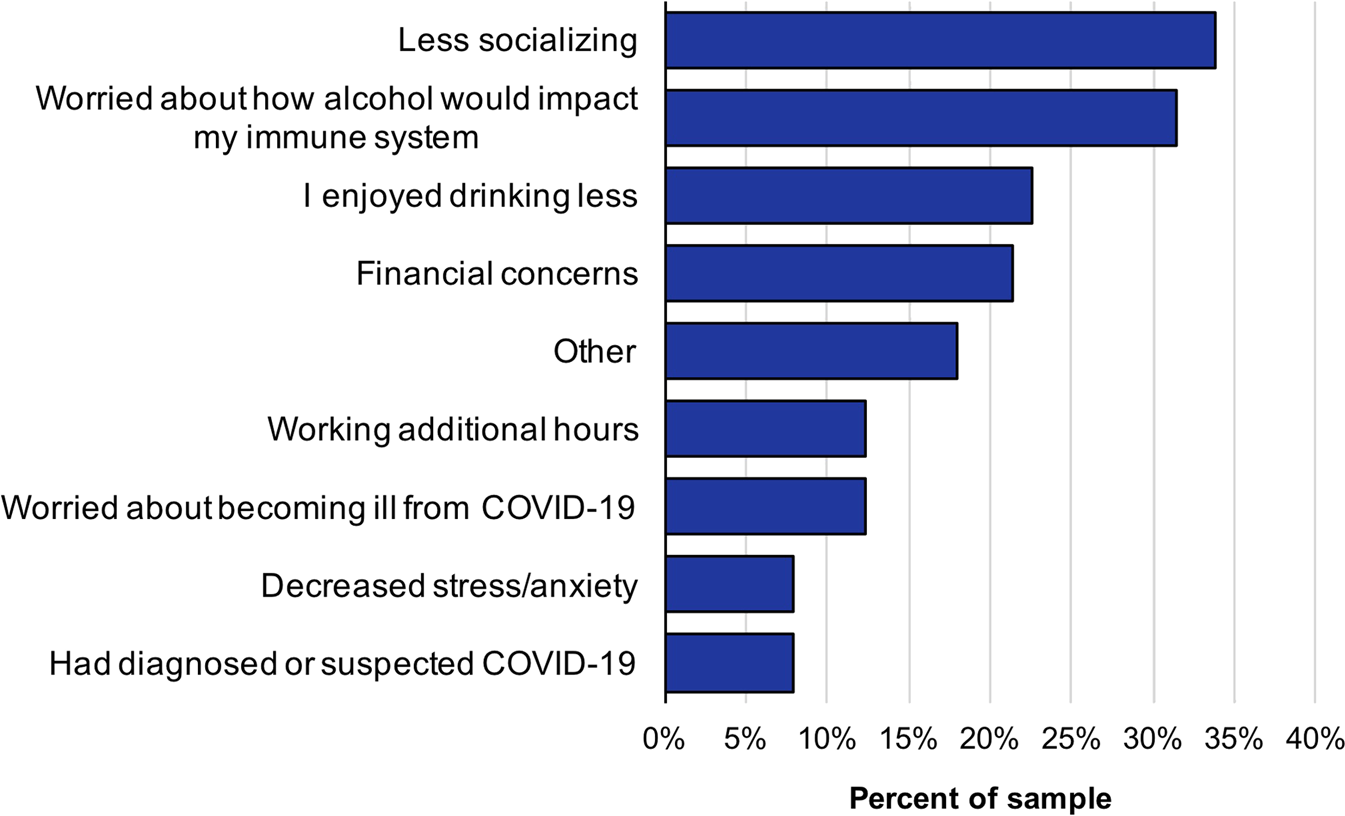
Reasons participants drank less than usual during the COVID-19 pandemic (N = 89).
Discussion
To our knowledge, this study is the first to assess the impacts of COVID-19 on alcohol consumption in a nationally representative sample of HSA with at-risk drinking. The current study highlighted that female gender, increased self-reported stress, boredom, access to alcohol, and disruption to daily routines may particularly increase susceptibility to elevated alcohol use during a pandemic. Although these factors may heighten the susceptibility to increased alcohol use during social distancing measures (or policies) implemented during a pandemic, these effects are not exclusively the result of a pandemic, these effects are not exclusively the result of a pandemic. These data provide evidence of changes in alcohol use and associated consequences during the COVID-19 pandemic, and suggest that the pandemic has led to greater alcohol use among help-seeking adults attempting to reduce their drinking.
Disasters (i.e., traumatic, natural, or environmental) have often been associated with increases in psychiatric symptoms such as depression and anxiety, and increases in substance use [47]. These conditions were mirrored during COVID-19, particularly during lockdowns throughout the world, where isolation potentially led to alcohol use and misuse in vulnerable individuals [48]. Variations in physiological stress and impaired decision-making increase risk of stress-induced alcohol consumption [48]. The literature on substance use emphasizes the importance of controlling the escalation of alcohol consumption during a crisis and notes two possible scenarios: an increase in consumption due to distress or a decrease in consumption due to the lower accessibility of the substance [26].
Kilian et al. [49] meta-analytical findings suggest that alcohol use declined during COVID-19 in the general population but revealed an increase in alcohol use among those with higher drinking levels prior to COVID-19, confirming the results of the current study. Emerging data during the pandemic has shown associations between anxiety, depression, and psychological distress with drinking among college students [50, 51] and adults globally [13, 52, 53]. Social isolation, boredom, increased availability, and reduced social support may lead to increased drinking [24, 28, 51]. Carlyle et al. [54] findings suggest that certain associates of chance (e.g., anxiety, depression, and resilience) and contextual factors (e.g., loneliness and boredom) contributed to changes in the frequency of use among treatment-seeking individuals during the pandemic. Similarly, among participants who reported drinking more in the present study, some reasons provided by participants were: increased stress/anxiety (65%), boredom, nothing to do at home (60%), spending more time at home (57%), easily became part of my routine’ (47%) and worried about COVID-19 and/or the future (38%). Efforts to overcome boredom, isolation, and psychological distress during a pandemic (e.g., digital interventions, virtual social events, public health education) may be helpful in reducing alcohol consumption.
Past literature suggests two possible mechanisms to explain changes in alcohol consumption in response to economic and employment factors: the first mechanism suggests any increase in alcohol consumption is related to increased situational or psychological distress (i.e., unemployment or loss of salary) and the second mechanism suggests that any decrease in alcohol consumption may be related to decreases in physical and financial availability of alcohol [55]. When asked about how their employment status has been affected by COVID-19, the majority of the participants were either working the same as before (43%) or were able to work from home’ (36%) and only a few were unemployed due to COVID-19 (15%). Further, roughly half (51.2%; 166/324) of the participants reported that their access to alcohol was affected by COVID-19 and 39% reported that their alcohol supply has increased (126/324). Nielsen et al. [56] suggest two possible causal explanations for higher alcohol consumption among those working from home. First, individuals with higher alcohol consumption may choose to work from home to conceal their alcohol use. Second, working from home may facilitate alcohol use that may otherwise not occur [56]. This may be attributed to the relatively high socioeconomic status (SES) of our sample (earned a bachelor’s degree or higher) and a relatively small sample of those who experienced job loss. The findings suggest that any job loss did not occur, or more specifically, to the extent to which it may have influenced a decrease in alcohol consumption.
Emerging literature suggests that women experienced an increase in drinking during the pandemic [24, 57, 58]. During the pandemic, high increases were observed among women when compared to men in terms of frequency (17% versus 11%, respectively), days of heavy drinking (41% versus 7% among men), and alcohol-related consequences [59]. Another study observed increases in heavy-drinking episodes by 41% in women since the COVID-19 lockdown [60]. Our results suggest that Female identifying individuals (p = 0.002) were significantly more likely to report drinking more than usual. It is possible that because women are more likely to drink as a result of stress and anxiety than men [61], the consequences of the pandemic put women at greater risk for increased consumption.
To our knowledge, this is the first study to show that the COVID-19 pandemic led to greater alcohol use among HSA attempting to reduce their drinking versus the general population. More research is needed to examine the contexts of drinking during COVID-19 among problem drinkers. Pandemic-like events are expected to increase in the coming decades [62]. The implementation of alcohol prevention strategies in the context of health crises, paying particular attention to individuals working from home and focusing on their reasons and motivations in this specific stress-induced alcohol use context, can help to mitigate the harmful effects of excessive alcohol consumption during challenging times. Identifying and addressing these contextual factors can inform alcohol prevention and control strategies during the current pandemic and may also inform risk and prevention strategies in future pandemics.
Limitations
This study has several limitations. These findings may not be generalizable to the general population of drinkers due to participants being predominantly female-identifying, White, having bachelor’s degrees or higher (some graduate school or a graduate degree) and being help-seeking for alcohol misuse. Considering that the majority of the participants held a bachelor’s degree or higher may allow increased flexibility in work arrangements, which may have impacted the differences in alcohol consumption [63]. Only self-report questions were used to collect drinking and impacts of drinking data, so the data may be under- or over-reported and subjected to social desirability bias. However, self-report of alcohol use and alcohol use-related behaviors is considered to be relatively valid [64]. Given the cross-sectional design and novelty of the COVID-19 pandemic, the current study limits our ability to make any causal inferences about changes in alcohol consumption prior to and during the pandemic beyond our self-reported question stem “since the pandemic began” anchoring people. Participants were also enrolled in an alcohol intervention study with different treatment groups that received varying levels of intervention. While no differences existed based on treatment conditions, findings may differ in a sample of individuals who were not participating in a treatment study. Lastly, participants’ geographic locations were not accounted for, so the differences in COVID-19 lockdown policies and alcohol sale policies (i.e., to-go alcohol, alcohol delivery services, and liquor stores deemed as essential services) may have influenced alcohol consumption. Despite the highlighted limitations, a novel contribution of the findings distinguishes the impacts of COVID-19 on alcohol consumption among individuals seeking to change their drinking prior to the pandemic.
Statements
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by both the Feinstein Institutes for Medical Research and Solutions IRB and all clinical investigations were conducted according to the principles expressed in the Declaration of Helsinki. The patients/participants provided their written informed consent to participate in this study.
Author contributions
AS: Conceptualized and designed survey, collected data, drafted outline, and edited paper. SF: Conducted data analysis, drafted sections of the paper, and edited paper. SM: Helped collect data and provided critical revision of paper. LS: Provided critical revision of paper. FM: Supervised data collection, provided critical revision of paper. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Institute on Alcohol Abuse and Alcoholism under grant number R01AA025058 (PI: Muench).
Acknowledgments
Authors wish to acknowledge Cameron Haslip and Sherry Oommen for their support of the project. Authors also thank Dr. Amy L. Stamates for helpful feedback on previous versions of this manuscript and Dawa Sherpa and Harold D. Montilla for editorial assistance. Most importantly, authors would like to gratefully acknowledge the study participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Manthey J Kilian C Carr S Barták M Bloomfield K Braddick F et al Use of Alcohol, Tobacco, Cannabis, and Other Substances during the First Wave of the SARS-CoV-2 Pandemic in Europe: A Survey on 36,000 European Substance Users. Subst Abuse Treat Prev Pol (2021) 16:36. 10.1186/s13011-021-00373-y
2.
Murray CJ Aravkin AY Zheng P Abbafati C Abbas KM Abbasi-Kangevari M et al Global burden of 87 Risk Factors in 204 Countries and Territories, 1990–2019: a Systematic Analysis for the Global Burden of Disease Study 2019. The Lancet (2020) 396(10258):1223–49. 10.1016/S0140-6736(20)30752-2
3.
Mofijur M Fattah IMR Alam MA Islam ABMS Ong HC Rahman SMA et al Impact of COVID-19 on the Social, Economic, Environmental and Energy Domains: Lessons Learnt from a Global Pandemic. Sustain Prod Consum (2021) 26:343–59. 10.1016/j.spc.2020.10.016
4.
Shang Y Li H Zhang R . Effects of Pandemic Outbreak on Economies: Evidence from Business History Context. Front Public Health (2021) 9:632043. 10.3389/fpubh.2021.632043
5.
Boscarino JA Kirchner HL Hoffman SN Sarorius J Adams RE . PTSD and Alcohol Use after the World Trade Center Attacks: A Longitudinal Study. J Trauma Stress (2011) 24:515–25. 10.1002/jts.20673
6.
Clay JM Parker MO . The Role of Stress-Reactivity, Stress-Recovery and Risky Decision-Making in Psychosocial Stress-Induced Alcohol Consumption in Social Drinkers. Psychopharmacology (2018) 235(11):3243–57. 10.1007/s00213-018-5027-0
7.
Hasin DS Sarvet AL Meyers JL Saha TD Ruan WJ Stohl M et al Epidemiology of Adult DSM-5 Major Depressive Disorder and its Specifiers in the United States. JAMA Psychiatry (2018) 75(4):336–46. 10.1001/jamapsychiatry.2017.4602
8.
Keyes KM Hatzenbuehler ML Grant BF Hasin DS . Stress and Alcohol: Epidemiologic Evidence. Alcohol Res (2012) 34(4):391–400.
9.
Wu P Liu X Fang Y Fan B Fuller CJ Guan Z et al Alcohol Abuse/dependence Symptoms Among Hospital Employees Exposed to a SARS Outbreak. Alcohol Alcohol (2008) 43(6):706–12. 10.1093/alcalc/agn073
10.
Avery AR Tsang S Seto EY Duncan GE . Stress, Anxiety, and Change in Alcohol Use during the COVID-19 Pandemic: Findings Among Adult Twin Pairs. Front Psychiatry (2020) 11:571084. 10.3389/fpsyt.2020.571084
11.
Holmes EA O'Connor RC Perry VH Tracey I Wessely S Arseneault L et al Multidisciplinary Research Priorities for the COVID-19 Pandemic: a Call for Action for Mental Health Science. The Lancet Psychiatry (2020) 7(6):547–60. 10.1016/S2215-0366(20)30168-1
12.
Jackson KM Merrill JE Stevens AK Hayes KL White HR . Changes in Alcohol Use and Drinking Context Due to the COVID‐19 Pandemic: a Multimethod Study of College Student Drinkers. Alcohol Clin Exp Res (2021) 45(4):752–64. 10.1111/acer.14574
13.
Rolland B Haesebaert F Zante E Benyamina A Haesebaert J Franck N . Global Changes and Factors of Increase in Caloric/salty Food Intake, Screen Use, and Substance Use during the Early COVID-19 Containment Phase in the General Population in France: Survey Study. JMIR Public Health Surveill (2020) 6(3):e19630. 10.2196/19630
14.
Gavurova B Khouri S Ivankova V Kubak M . Changes in Alcohol Consumption and Determinants of Excessive Drinking during the COVID-19 Lockdown in the Slovak Republic. Front Public Health (2022) 9:791077. 10.3389/fpubh.2021.791077
15.
Sidor A Rzymski P . Dietary Choices and Habits during COVID-19 Lockdown: Experience from Poland. Nutrients (2020) 12:1657. 10.3390/nu12061657
16.
Schmidt RA Genois R Jin J Vigo D Rehm J Rush B . The Early Impact of COVID-19 on the Incidence, Prevalence, and Severity of Alcohol Use and Other Drugs: A Systematic Review. Drug Alcohol Depend (2021) 228:109065. 10.1016/j.drugalcdep.2021.109065
17.
Koopmann A Georgiadou E Kiefer F Hillemacher T . Did the General Population in Germany Drink More Alcohol during the COVID-19 Pandemic Lockdown?Alcohol Alcohol (2020) 55(6):698–9. 10.1093/alcalc/agaa058
18.
Chick J . Alcohol and COVID-19. Alcohol Alcohol (2020) 55(4):341–2. 10.1093/alcalc/agaa039
19.
The Nielsen Company. Rebalancing the ‘COVID-19 Effect’ on Alcohol Sales (2020). Available at: https://www.nielsen.com/us/en/insights/article/2020/rebalancing-the-covid-19-effect-on-alcohol-sales/(Accessed October 21, 2022).
20.
Gruenewald PJ Johnson FW Treno AJ . Outlets, Drinking and Driving: a Multilevel Analysis of Availability. J Stud Alcohol (2002) 63(4):460–8. 10.15288/jsa.2002.63.460
21.
van Oers JA Garretsen HF . The Geographic Relationship between Alcohol Use, Bars, Liquor Shops and Traffic Injuries in Rotterdam. J Stud Alcohol (1993) 54(6):739–44. 10.15288/jsa.1993.54.739
22.
Biddle N Edwards B Gray M Sollis K . Alcohol Consumption during the COVID-19 Period: May 2020 (2020). Available at: https://csrm.cass.anu.edu.au/research/publications/alcohol-consumption-during-covid-19-period-may-2020 (Accessed October 21, 2022).
23.
Campbell AM . An Increasing Risk of Family Violence during the Covid-19 Pandemic: Strengthening Community Collaborations to Save Lives. Forensic Sci Int Rep (2020) 2:100089. 10.1016/j.fsir.2020.100089
24.
Grossman ER Benjamin-Neelon SE Sonnenschein S . Alcohol Consumption during the COVID-19 Pandemic: A Cross-Sectional Survey of US Adults. Int J Environ Res Public Health (2020) 17(24):9189. 10.3390/ijerph17249189
25.
Killgore WD Cloonan SA Taylor EC Lucas DA Dailey NS . Alcohol Dependence during COVID-19 Lockdowns. Psychiatry Res (2021) 296:113676. 10.1016/j.psychres.2020.113676
26.
Rehm J Kilian C Ferreira-Borges C Jernigan D Monteiro M Parry CDH et al Alcohol Use in Times of the COVID 19: Implications for Monitoring and Policy. Drug Alcohol Rev (2020) 39(4):301–4. 10.1111/dar.13074
27.
Vanderbruggen N Matthys F Van Laere S Zeeuws D Santermans L Van den Ameele S et al Self-reported Alcohol, Tobacco, and Cannabis Use during COVID-19 Lockdown Measures: Results from a Web-Based Survey. Eur Addict Res (2020) 26:309–15. 10.1159/000510822
28.
Wardell JD Kempe T Rapinda KK Single A Bilevicius E Frohlich JR et al Drinking to Cope during COVID‐19 Pandemic: The Role of External and Internal Factors in Coping Motive Pathways to Alcohol Use, Solitary Drinking, and Alcohol Problems. Alcohol Clin Exp Res (2020) 44(10):2073–83. 10.1111/acer.14425
29.
Weerakoon SM Jetelina KK Knell G Messiah SE . COVID-19 Related Employment Change Is Associated with Increased Alcohol Consumption during the Pandemic. Am J Drug Alcohol Abuse (2021) 47(6):730–6. 10.1080/00952990.2021.1912063
30.
Huckle T Parker K Romeo JS Casswell S . Online Alcohol Delivery Is Associated with Heavier Drinking during the First New Zealand COVID‐19 Pandemic Restrictions. Drug alcohol Rev (2021) 40(5):826–34. 10.1111/dar.13222
31.
McPhee MD Keough MT Rundle S Heath LM Wardell JD Hendershot CS . Depression, Environmental Reward, Coping Motives and Alcohol Consumption during the COVID-19 Pandemic. Front Psychiatry (2020) 11:574676. 10.3389/fpsyt.2020.574676
32.
Acuff SF Strickland JC Tucker JA Murphy JG . Changes in Alcohol Use during COVID-19 and Associations with Contextual and Individual Difference Variables: A Systematic Review and Meta-Analysis. Psychol Addict Behav (2022) 36(1):1–19. 10.1037/adb0000796
33.
Garnett C Jackson S Oldham M Brown J Steptoe A Fancourt D . Factors Associated with Drinking Behaviour during COVID-19 Social Distancing and Lockdown Among Adults in the UK. Drug Alcohol Depend (2021) 219:108461. 10.1016/j.drugalcdep.2020.108461
34.
Kilian C Carr S Schulte B Manthey J . Increased Alcohol‐specific Mortality in Germany during COVID‐19: State‐level Trends from 2010 to 2020. Drug Alcohol Rev (2022) 42:633–40. 10.1111/dar.13573
35.
Tucker JS Rodriguez A Green HD Jr Pollard MS . Trajectories of Alcohol Use and Problems during the COVID-19 Pandemic: The Role of Social Stressors and Drinking Motives for Men and Women. Drug and Alcohol Dependence (2022) 232:109285. 10.1016/j.drugalcdep.2022.109285
36.
Patel AK Balasanova AA . Unhealthy Alcohol Use. JAMA (2021) 326(2):196. 10.1001/jama.2020.2015
37.
Rehm J . The Risks Associated with Alcohol Use and Alcoholism. Alcohol Res Health (2011) 34(6):135–43.
38.
Capasso A Jones AM Ali SH Foreman J Tozan Y DiClemente RJ . Increased Alcohol Use during the COVID-19 Pandemic: The Effect of Mental Health and Age in a Cross-Sectional Sample of Social media Users in the US. Prev Med (2021) 145:106422. 10.1016/j.ypmed.2021.106422
39.
Deeken F Reichert M Zech H Wenzel J Wedemeyer F Aguilera A et al Patterns of Alcohol Consumption Among Individuals with Alcohol Use Disorder during the COVID-19 Pandemic and Lockdowns in Germany. JAMA Netw Open (2022) 5(8):e2224641. 10.1001/jamanetworkopen.2022.24641
40.
Harris PA Taylor R Minor BL Elliott V Fernandez M O'Neal L et al The REDCap Consortium: Building an International Community of Software Platform Partners. J Biomed Inform (2019) 95:103208. 10.1016/j.jbi.2019.103208
41.
Harkness A . The Pandemic Stress Index. Coral Gables, FL: University of Miami (2020).
42.
Stoddard J Reynolds EK Paris R Haller S Johnson S Zik J et al The Coronavirus Impact Scale: Construction, Validation, and Comparisons in Diverse Clinical Samples. PsyArXiv Preprints [Preprint] (2021). Available at: https://psyarxiv.com/kz4pg/ (Accessed October 22, 2022).
43.
Mehta S . COVID-19 Community Response Survey. Baltimore, Maryland: Johns Hopkins Bloomberg School of Public Health (2020). Available at: https://tools.niehs.nih.gov/dr2/index.cfm/resource/22096 (Accessed November 2, 2022).
44.
Hamilton CM Strader LC Pratt JG Maiese D Hendershot T Kwok RK et al The PhenX Toolkit: Get the Most from Your Measures. Am J Epidemiol (2011) 174(3):253–60. 10.1093/aje/kwr193
45.
SAS Institute Inc. SAS/ACCESS 9.4 Interface to ADABAS: Reference. Cary, NC: SAS Institute Inc. (2013).
46.
StataCorp. Stata Statistical Software: Release, 15. College Station, TX: StataCorp LLC (2017).
47.
Galea S Merchant RM Lurie N . The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention. JAMA Inter Med (2020) 180(6):817–8. 10.1001/jamainternmed.2020.1562
48.
Clay JM Parker MO . Alcohol Use and Misuse during the COVID-19 Pandemic: A Potential Public Health Crisis?Lancet Public Health (2020) 5(5):e259. 10.1016/S2468-2667(20)30088-8
49.
Kilian C O'Donnell A Potapova N López‐Pelayo H Schulte B Miquel L et al Changes in Alcohol Use during the COVID‐19 Pandemic in Europe: A Meta‐analysis of Observational Studies. Drug Alcohol Rev (2022) 41(4):918–31. 10.1111/dar.13446
50.
Gritsenko V Skugarevsky O Konstantinov V Gritsenko V Skugarevsky O Konstantinov V et al COVID 19 Fear, Stress, Anxiety, and Substance Use Among Russian and Belarusian university Students. Int J Ment Health Addict (2020) 19:2362–8. 10.1007/s11469-020-00330-z
51.
Lechner WV Laurene KR Patel S Anderson M Grega C Kenne DR . Changes in Alcohol Use as a Function of Psychological Distress and Social Support Following COVID-19 Related University Closings. Addict Behav (2020) 110:106527. 10.1016/j.addbeh.2020.106527
52.
Callinan S Smit K Mojica‐Perez Y D'Aquino S Moore D Kuntsche E . Shifts in Alcohol Consumption during the COVID‐19 Pandemic: Early Indications from Australia. Addiction (2021) 116(6):1381–8. 10.1111/add.15275
53.
Rodriguez LM Litt DM Stewart SH . Drinking to Cope with the Pandemic: The Unique Associations of COVID-19-Related Perceived Threat and Psychological Distress to Drinking Behaviors in American Men and Women. Addict Behav (2020) 110:106532. 10.1016/j.addbeh.2020.106532
54.
Carlyle M Leung J Walter ZC Juckel J Salom C Quinn CA et al Changes in Substance Use Among People Seeking Alcohol and Other Drug Treatment during the COVID-19 Pandemic: Evaluating Mental Health Outcomes and Resilience. Subst Abuse (2021) 15:11782218211061746–8. 10.1177/11782218211061746
55.
De Goeij MC Suhrck M Toffolutti V van de Mheen D Schoenmakers TM Kunst AE . How Economic Crises Affect Alcohol Consumption and Alcohol-Related Health Problems: a Realist Systematic Review. Soc Sci Med (2015) 131:131–46. 10.1016/j.socscimed.2015.02.025
56.
Nielsen MB Christensen JO Knardahl S . Working at home and Alcohol Use. Addict Behav Rep (2021) 14:100377. 10.1016/j.abrep.2021.100377
57.
Hanson JD Noonan C Harris A Oziel K Sarche M MacLehose RF et al Alcohol Consumption during COVID Among Women with an Existing Alcohol-Use Disorder. Int J Environ Res Public Health (2021) 18(18):9460. 10.3390/ijerph18189460
58.
Pollard MS Tucker JS Green HD . Changes in Adult Alcohol Use and Consequences during the COVID-19 Pandemic in the US. JAMA Netw Open (2020) 3(9):e2022942. 10.1001/jamanetworkopen.2020.22942
59.
Avena NM Simkus J Lewandowski A Gold MS Potenza MN . Substance Use Disorders and Behavioral Addictions during the COVID-19 Pandemic and COVID-19-Related Restrictions. Front Psychiatry (2021) 12:653674. 10.3389/fpsyt.2021.653674
60.
TheCorporation RAND . Alcohol Consumption Rises Sharply during Pandemic Shutdown; Heavy Drinking by Women Rises 41% (2020). Available at: https://www.rand.org/news/press/2020/09/29.html (Accessed December 1, 2022).
61.
Peltier MR Verplaetse TL Mineur YS Petrakis IL Cosgrove KP Picciotto MR et al Sex Differences in Stress-Related Alcohol Use. Neurobiol Stress (2019) 10:100149. 10.1016/j.ynstr.2019.100149
62.
Morens DM Fauci AS . Emerging Pandemic Diseases: How We Got to COVID-19. Cell (2020) 182(5):1077–92. 10.1016/j.cell.2020.08.021
63.
Dey M Frazis H Loewenstein MA Sun H . Ability to Work from home: Evidence from Two Surveys and Implications for the Labor Market in the COVID-19 Pandemic. Washington, D.C., US: Monthly Labor Review U.S. Bureau of Labor Statistics (2020). 10.21916/mlr.2020.14
64.
Jeremy N Michael L . Accuracy of Self-Reported Drinking: Observational Verification of ‘Last Occasion’ Drink Estimates of Young Adults. Alcohol Alcohol (2011) 46(6):709–13. 10.1093/alcalc/agr138
Summary
Keywords
COVID-19, pandemic, adult, alcohol, moderation
Citation
Srinagesh A, Forthal S, Madden SP, Stein LAR and Muench F (2023) Impacts of COVID-19 on alcohol use among help-seeking adults. Adv. Drug Alcohol Res. 3:11159. doi: 10.3389/adar.2023.11159
Received
30 December 2022
Accepted
02 May 2023
Published
15 May 2023
Volume
3 - 2023
Edited by
Emmanuel Onaivi, William Paterson University, United States
Reviewed by
Z. Carl Lin, Harvard Medical School, United States
Lester Rosario Rodriguez, University of Puerto Rico, Puerto Rico
Updates
Copyright
© 2023 Srinagesh, Forthal, Madden, Stein and Muench.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aradhana Srinagesh, asrinagesh@uri.edu
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.