Abstract
Background: Hernia patches for umbilical hernia repair have gained popularity due to their short operation time and ease of use. However, up to 10% re-operation and 8% recurrence rates at 2-year follow-up have been published. This retrospective cohort study presents the long-term results of the hernia patch technique for umbilical hernia repair.
Methods: All adult patients who underwent a primary umbilical hernia repair at Oulu University Hospital hernia surgery units during 2014–2018 were included in the study. The primary outcome measure was recurrence rate. Secondary outcomes were complications and re-operation rate.
Results: A total of 619 elective primary umbilical hernia repairs were performed during 2014–2018. The major technique used was Ventralex™ ST hernia patch repair (79.0%, 488/619) for small hernias with a mean width of 1.8 (SD 0.79) cm. Most of the patches (84.7%, 414/488) were placed in the preperitoneal space. Hernia recurrence rate of patient operated on using Ventralex™ ST hernia patch was 2.5% (12/488) during a mean follow-up time of 68 (SD 16, 43–98) months. Re-operation rate for another reason than recurrence was 1.6% (8/488). Clavien-Dindo complications ≥3 occurred in 4.1% (20/488) of cases and surgical site infection rate was 3.3% (16/488).
Conclusion: Umbilical hernia repair using a Ventralex™ ST hernia patch placed in preperitoneal space have acceptable results in terms of recurrence and re-operations in this cohort study.
Introduction
Umbilical hernia is classified as a primary abdominal wall hernia with no previous surgery to the hernia site located at the midline between the rectus sheaths 3 cm above or 3 cm below the umbilicus [1]. Prevalence of umbilical hernia in adults is about 2% [2]. Umbilical hernia repair is the second most common hernia operation in the Western world [3].
The European Hernia Society (EHS) and American Hernia Society (AHS) recommend the use of a flat permanent mesh in preperitoneal space to repair an umbilical hernia when the hernia defect is larger than 1 cm [4]. Recurrence rate after suture repair of umbilical hernia can be up to 54.5% [2]. Recent meta-analysis concluded that mesh repair compared to suture repair is associated with a lower risk of recurrence and no difference in surgical-site infection, hematomas, or chronic pain [3].
A ventral patch is a preformed mesh designed mainly for small umbilical hernia repairs. The patch can be placed either in intraperitoneal or preperitoneal space through a small fascial defect, after which it self-expands. Hernia repair using a ventral patch is considered a quick and elegant procedure [5]. The composite prosthesis used in Oulu University Hospital, Ventralex™ ST hernia patch (Bard Davol, Warwick, RI, United States), consists of non-absorbable anterior mesh, an absorbable posterior layer and memory ring. The posterior layer is designed to keep the prosthesis from adhering to the intestine [6]. Intraperitoneal behaviour of three composite meshes (Ventralex™ ST hernia Patch, Proceed™ Ventral Patch and Parietex™ Composite Ventral Patch) have been studied on rabbits with serial follow up laparoscopies after implantation. Omental or bowel adhesion were found at 6 weeks in 33%–89% of cases despite different protective layers [7].
Ponten et al. reported significantly more complications and more re-operations in the ventral patch group (Proceed® mesh) compared to preperitoneal flat polypropylene mesh [8]. There are also case reports about mesh migration to bowel after Venralex™ hernia patch used in incisional hernia repair [9]. Several studies have shown low complication, recurrence and reoperation rates after ventral patch repair for small umbilical hernias [5, 6, 10–12]. Nevertheless, authorities from hernia surgical associations have taken a sceptical view of ventral patches, mainly because of costs and complications and recurrences seen after patch repair has been used in improper situations [4]. Most small umbilical hernias in the Oulu University Hospital region have been operated on using Ventralex™ ST hernia patch placed either in preperitoneal or intraperitoneal space. Due to the interest in achieving clarity to this contradiction, the aim of this study is to investigate the long-term results of umbilical hernia patch repair.
Methods
Study Design
This is a retrospective cohort study. A surgical database search was conducted to find all patients operated on for primary umbilical hernia in hernia surgery units in Oulu University Hospital between 2014 and 2018. This time period was chosen in order to obtain an adequate follow-up time and number of patients. Exclusion criteria were age under 18, emergency operation, recurrent umbilical hernia repair. Study flow chart is seen in Figure 1. Patients, who had an elective primary umbilical hernia repair using the Ventralex™ ST hernia patch were included. Ethical review board permission was obtained prior starting the study.
FIGURE 1
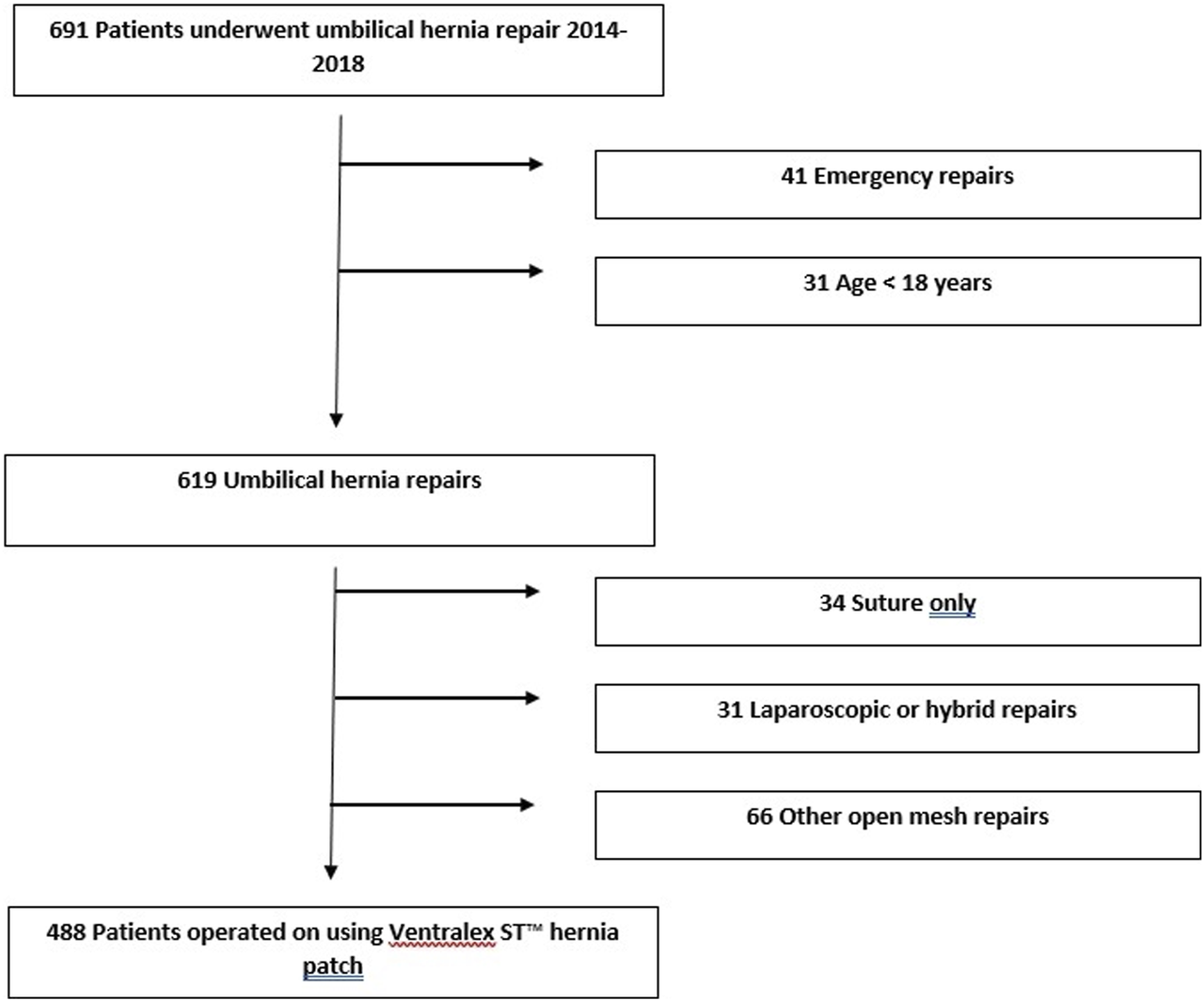
Flow chart of patients in the study.
Medical records were accessed to find baseline patient information, operative notes, and post-operative course. Follow-up and complication data were collected between January 2022 and May 2022 from patients’ medical files by a single researcher (JH). Number of all operations are presented mainly to describe the entire patient population. Primary endpoints for this study were hernia recurrence and hernia-related re-operations. A patient was considered to have recurrence if recurrent hernia was clinically diagnosed, seen in radiological examination or if patient underwent operation for recurrence. Secondary endpoints were surgical site infection rate (SSI), surgical site occurrence (SSO), other complications graded using Clavien-Dindo classification and chronic pain.
Statistical Methods
Continuous variables are presented as means with standard deviations (SD), unless otherwise stated. Categorical data are presented as percentages and proportions.
A power analysis was not performed, since all eligible patients during the study period were included in the study. Student’s t-test or Welch’s t-test was used for between group comparisons for continuous variables. The Welch’s t-test was used if the assumption of homogenous variances was not met. Categorical variables were compared using Χ2 or Fisher’s exact test. Two-tailed p-values are reported. SPSS for windows (IBM Corp. Released 2019. IBM SPSS Statistics for Windows, Version 26.0. Armonk, NY: IBM Corp) was used for statistical analyses.
Results
Between 2014 and 2018 a total of 619 adult patients underwent elective umbilical hernia repair and 488 of these patients were operated on using the Ventralex™ ST hernia patch (Figure 1). Decisions concerning operative technique were made according to the preference of the operating surgeon.
Baseline of patients and hernia characteristics are presented in Table 1. Two thirds of the patients were males (n = 331, 67.9%) with mean age being 49.6 (SD 13.0) years. Patients were relatively healthy with only 11.5% (n = 56) having an American Society of Anesthesiologist (ASA) rating of ≥3. The prevalence of smoking was 18% (n = 87) at the time of operation. A majority (n = 350, 71.6%) of hernias were classified as medium size (1–4 cm) with only 1.6% (n = 8) being large (>4 cm). The mean hernia width for Ventralex™ ST hernia patch repair was 1.8 (SD 0.79, 0.3–6) cm. The operating surgeon diagnosed coexistent rectus diastasis in 5.7% (n = 28) patients. Patients with noted diastasis had more recurrences 14.3% (n = 4) vs. patients with no mention of rectus diastasis 1.7% (n = 8) (p 0.003).
TABLE 1
| All patients (n = 488) | Recurrence (n = 12) | No recurrence (n = 476) | p-value | |
|---|---|---|---|---|
| Age, mean (SD, range) | 49.6 (13.0, 20–88) | 43.5 (18.0, 23–77) | 49.8 (12.9, 20–88) | 0.10 |
| Female, n (%) | 157 (32) | 7 (58) | 150 (32) | 0.063 |
| Body Mass Index, kg/m2, mean (SD) | 28.9 (4.9) | 28.8 (6.1) | 28.9 (4.9) | >0.9 |
| Comorbidities | ||||
| Cardiac disease, n (%) | 140 (28.7) | 2 (16.7) | 138 (29.0) | 0.52 |
| Diabetes mellitus, n (%) | 58 (11.9) | 2 (16.7) | 56 (11.8) | 0.64 |
| Hepatic disease, n (%) | 4 (0.8) | 1 (8.3) | 3 (0.6) | 0.10 |
| Pulmonary disease, n (%) | 68 (13.9) | 1 (8.3) | 67 (14.1) | >0.9 |
| Renal disease, n (%) | 4 (0.8) | 0 (0) | 4 (0.8) | >0.9 |
| Current smoker, n (%) | 87 (17.8) | 3 (25) | 84 (17.6) | 0.46 |
| ASA 1, n (%) | 178 (36.5) | 3 (25) | 175 (36.8) | 0.60 |
| ASA 2, n (%) | 253 (51.8) | 7 (58.3) | 246 (51.7) | — |
| ASA 3, n (%) | 56 (11.5) | 2 (16.7) | 54 (11.3) | — |
| ASA 4, n (%) | 1 (0.2) | 0 (0) | 1 (0.2) | — |
| Hernia characteristics(n = 448) | ||||
| Hernia width <1 cm, n (%) | 91 (20.3) | 3 (30) | 88 (20.1) | 0.69 |
| Hernia width 1–4 cm, n (%) | 349 (77.9) | 7 (70) | 342 (78.1) | — |
| Hernia width 4 cm, n (%) | 8 (1.8) | 0 (0) | 8 (1.8) | — |
| Mean hernia width, cm (SD, range) | 1.8 (0.79, 0.3–6) | 1.5 (0.39, 1–2) | 1.9 (0.8, 0.3–6) | 0.12 |
| Rectus diastasis, n (%) | 28 (5.7) | 4 (33.3) | 24 (5.1) | 0.003 |
Description of patient characteristics.
For continuous variables standard deviation (SD) is presented.
Age (years) at operation is presented in the table.
Operative details for patients operated on with Ventralex™ ST hernia patch are described in Table 2. A majority of cases were performed by experienced surgeons (n = 293, 59.9%). Fascial defect was closed in 60 (12.3%) patients. Mesh was placed in preperitoneal space in 414 (84.8%) patients, in intraperitoneal space in 30 (5.9%) patients, and was unclear in 45 (9.2%) patients. The location of the mesh was classified as indistinct if the operating surgeon was not sure that the mesh was completely in the preperitoneal space or if the location remained unclear based on the surgical report. Dissection of the preperitoneal space is usually done through a small hernia port and sometimes it might be difficult to say for sure if there are small tears in the peritoneum or if the small peritoneal tears have been completely closed. A small 4-cm patch was most frequently used (n = 228, 46.7%), followed by a medium-sized 6-cm patch (n = 177, 36.3%). This resulted in a mean of 1.8 cm (SD 0.63) mesh overlap per side. Most of the operations were performed as a day case surgery with a mean length of stay of 0.7 (SD 0.7, min-max 0–7) days.
TABLE 2
| All patients n = 488 | Recurrence n = 12 | No recurrence n = 476 | p-value | |
|---|---|---|---|---|
| Specialist operator vs. resident, n (%) | 293 (60) | 5 (41.7) | 288 (60.5) | 0.24 |
| Fascia defect completely closed, n (%) | 60 (12.3) | 4 (33.3) | 56 (11.8) | 0.048 |
| Antibiotic prophylaxis, n (%) | 379/484 (78) | 11 (91.7) | 368/472 (78.0) | 0.48 |
| Hernia completely reducible, n (%) | 328/461 (70.9) | 9/11 (81.8) | 318/450 (70.7) | 0.52 |
| Day surgery, n (%) | 193 (39.5) | 6 (50) | 187 (40.7) | 0.65 |
| Mesh location, n (%) | 0.14 | |||
| Preperitoneal | 414 (84.8) | 9 (75) | 405 (85.1) | — |
| Intraperitoneal | 29 (5.9) | 0 (0) | 29 (6.1) | — |
| Indistinct | 45 (9.2) | 3 (25) | 42 (8.8) | — |
| Mesh size, n (%) | 0.11 | |||
| 4 cm | 228 (46.7) | 9 (75) | 219 (46.6) | — |
| 6 cm | 177 (36.3) | 3 (25) | 174 (37.0) | — |
| 8 cm | 77 (15.8) | 0 (0) | 77 (16.4) | — |
| Mesh overlap cm, mean (SD, min–max) | 1.8 (0.63, 0.5–3.8) | 1.5 (0.42, 1–2.3) | 1.8 (0.64, 0.5–3.8) | 0.13 |
| <1 cm, n (%) | 69/442 (15.6) | 2/10 (20) | 67/432 (15.5) | 0.87 |
| 1–2 cm, n (%) | 237/442 (53.6) | 6/10 (60) | 231/432 (53.5) | — |
| 2–3 cm, n (%) | 125/442 (28.3) | 2/10 (20) | 123/432 (28.5) | — |
| ≥3 cm, n (%) | 11/442 (2.5) | 0/10 (0) | 11/432 (2.5) | — |
| Suture material to fixate the mesh | 0.61 | |||
| Fast absorbable, n (%) | 11/458 (2.4) | 0 (0) | 12/470 (2.3) | — |
| Slow absorbable, n (%) | 8/458 (1.7) | 0 (0) | 8/470 (1.7) | — |
| Non-absorbable, n (%) | 438/458 (95.6) | 12 (100) | 438/470 (95.7) | — |
Description of operative details in operations using a Ventralex™ ST hernia patch.
Mesh overlap is reported in cm per side.
Long-term results for Ventralex™ ST hernia patch repair are summarized in Table 3. Hernia recurrence was found in 12 (2.5%) patients during the mean follow-up time of 68 (SD 16) months. Reoperation rate from any cause was 4.1% (n = 20). Three of the patients underwent reoperation due to fistula, three for chronic pain and rectus diastasis (two of these patients also had recurrence) and another three also for pain and excess scar formation or abnormal reaction to mesh. One patient was operated on for SSI. Fistulas were skin to mesh or suture fistulas. No enterocutaneous fistulas was found in this series. In reoperations due to fistula mesh was not explanted. Mesh was removed in seven patients during reoperations for chronic pain or infection or recurrence. Preperitoneal mesh location resulted 7.7% (n = 32), intraperitoneal 10.3% (n = 3) and Indistinct 17.8% (n = 8) Claviend-Dindo ≥2 complication rate (p 0.041). Recurrence rate with preperitoneal mesh was 2.2% (n = 9), intraperitoneal 0% (n = 0) and with indistinct 6.7% (n = 3) (p 0.12). Similarly Clavien-Dindo ≥3 complication rates were 3.6% (n = 15) with preperitoneal mesh, 0% (n = 0) intraperitoneal and 11.1% (n = 5) for indistinct (p 0.05). All three patients operated for chronic pain were originally operated with fascial defect left open. Symptomatic seromas also occurred in patients whose fascial defect was not closed. Patient characteristics (Table 1) and operation data (Table 2) are also presented separately for patients with recurrence and for patients without recurrence.
TABLE 3
| All patients (n = 488) | Recurrence (n = 12) | No recurrence (n = 476) | p-value | |
|---|---|---|---|---|
| Hernia recurrence, n (%) | 12 (2.5) | — | — | |
| Hernia recurrence operated, n (%) | 12 (2.5) | — | — | |
| Re-operation for other reason, n (%) | 8 (1.6) | 3 (33) | 5 (2.9) | |
| SSI, n (%) | 16 (3.3) | 0 | 16 (3.3) | >0.9 |
| Seroma, n (%) | 3 (0.6) | 0 | 3 (0.6) | >0.9 |
| Hematoma, n (%) | 5 (1.0) | 0 | 5 (1.1) | >0.9 |
| SSO, n (%) | 40 (8.2) | — | — | |
| SSOPI, n (%) | 20 (4.1) | — | — | |
| Chronic pain, n (%) | 8 (1.6) | 1 (8.3) | 7 (1.5) | 0.18 |
| Clavien-Dindo, during follow-up time, n (%) | — | |||
| 1 | 2 (0.4) | — | — | |
| 2 | 23 (4.7) | — | — | |
| 3 | 20 (4.1) | — | — | |
| 30-day Clavien-Dindo, n (%) | — | |||
| 1 | 2 (0.4) | — | — | |
| 2 | 26 (5.7) | — | — | |
| 3 | 2 (0.4) | — | — | |
| Follow-up time months, mean (SD, min-max) | 68 (16, 43–98) | 72 (15, 48–93) | 68 (16, 43–98) | 0.32 |
Description of results for patients operated on using Ventralex ST™ hernia patch.
Standard deviation (SD) is presented for continuous variables.
Surgical site occurrence (SS0) includes seromas and hematomas.
Surgical site occurrences requiring procedural interventions (SSOPI).
Discussion
In line with previous reports, this study showed that the use of the Ventralex™ ST hernia patch placed in preperitoneal space in umbilical hernia repair has acceptable results in terms of recurrence and complications.
Porrero et al. [6] reported similar complication rates in their retrospective series. Studies with smaller numbers of patients have had more mixed results, with recurrence rates ranging from 0% to 8.9% [5, 11, 13, 14]. To our knowledge, there is only one published randomized controlled trial comparing flat preperitoneal polypropylene mesh with an intraperitoneal or preperitoneal Proceed® ventral patch in small umbilical hernia repairs. In this study, significantly more complications and more re-operations in the ventral patch group were reported compared to flat mesh [8].
European and American hernia associations recommend in their guidelines that symptomatic umbilical hernias should be repaired using an open approach with a preperitoneal flat mesh. In the associations’ guideline article, the authors concluded that the use of intraperitoneal preformed patches for umbilical hernia repairs may shorten operating time, but may be associated with increased complication rates compared with placing a flat mesh in the preperitoneal space. They also point out the high costs of pre-shaped prosthetics with anti-adhesive barriers [4].
There are several different techniques for mesh placement in the preperitoneal space using open surgery, laparoscopic or robotic approaches. For smaller umbilical hernias, open technique using ventral patches is attractive because the procedure is quick and simple even for less-experienced surgeons. There are numerous composite hernia patches on the market, and these can in most cases be inserted into preperitoneal or intraperitoneal space. The significance of patch placement either in preperitoneal or intraperitoneal space remains unclear [8]. Intraperitoneal Ventralex™ hernia patch has shown similar complication rates but lower early postoperative pain scores when compared to onlay mesh [11]. The most severe complications are related to mesh bowel attachment or abdominal mesh migration favouring preperitoneal mesh placement. It is not easy to avoid peritoneal tears during the preperitoneal space dissection or mesh placement pass relatively small hernia port. Because of this it might be beneficial to use mesh with antiadhesive barrier even when mesh is placed preperitoneally. Preperitoneal technique secure adequate mesh contact to abdominal wall, whereas in intraperitoneal mesh placement preperitoneal fat might interfere mesh integration. In this cohort preperitoneal location of the mesh decrease recurrence and complication rates compared to intraperitoneal or indistinct mesh locations. However, the study design was not intentional for this kind of comparison and our results are not all statistically significant. Superiority of preperitoneal placement of Ventralex™ has not been proven in comparative study [15].
In this study population, almost one-fifth of patients had a small hernia (width<1 cm) where mesh repair was not recommended. However, there is recent evidence favouring mesh repair also in this patient group. A Danish register study concluded that mesh reduces recurrences even in small hernias but increases early complications. In this series onlay mesh repairs had a lower recurrence rate compared to other types of meshes [16].
In this study population, fascia defect was mostly left open and mesh was sutured to the edges of the defect, contrary to recent guideline recommendation by EHS. Fascial defect closure is one of the essential part of all types of ventral hernia repair techniques. It has been shown to reduce hernia recurrences and SSO in laparoscopic intraperitoneal onlay mesh repairs [17, 18]. Leaving the fascia open did not seem to cause a large number of recurrences in this study. However, mesh to skin or suture fistulas and mesh reactions led to several (6) re-operations. These complications might be avoidable if the fascia is closed. Therefore, we recommend that the fascia defect should be closed when using a preformed hernia patch. A large proportion of patients received small (4 cm) mesh, although current guidelines recommend a minimum of a 2-cm mesh overlap which is impossible to achieve with small mesh. Mesh overlap of less than 1 cm has shown to be a risk factor for recurrence when using Ventralex™ ST hernia patch for umbilical hernia repair [19]. Although the mesh overlap is smaller than recommended, again it did not seem to cause problems in this series when median hernia size was relatively small.
Limitations
This is a cohort study with all limitations in relation to retrospective data collection. A major problem is caused by the fact that surgical reports for pre- and intraoperative parameters are incomplete. Surgical technique was not standardized, and surgeons used what they were familiar with or what they thought was best for the given patient (e.g., whether to close the defect or not, or what size mesh to use), which led to heterogeneity. Further, follow-up data were collected merely from the medical records, which inevitably led to underreporting of complications.
Still, we believe that recurrence rate and (Clavien-Dindo ≥3) complications are close to correct since data were collected from our own hernia surgical units within our geographically vast hospital district. Patients usually seek treatment for complications at the hospital where they were operated on.
Information bias may exist depending on surgeons’ choice of operative method and the differing quality of individual operative reports. Simple hernia surgery in Finland is done by general surgeons who have adopted the patch repair technique since Ventralex™ ST hernia patch has been available. Hereby, a majority of surgeons were experienced and familiar with the technique. However, our patient cohort is highly selected, and results might not be generalizable. It should be noted that patients in this cohort were relatively healthy in terms of comorbidities and mostly of working age. Despite the retrospective nature of this study, the outcomes reflect normal clinical practice in our hospital. Our study design did not give us the possibility to make any kind of comparative analysis of different operative techniques or meshes.
One of the major limitations is that we do not have any data on patient satisfaction or quality of life, which should be explored in future studies on umbilical hernia repair. According to previous study patients reported mostly good or excellent satisfaction 2 years after umbilical or incisional hernia repair using Ventralex™ ST hernia patch [20].
Risk factor analysis for recurrence is impossible due to the small number of recurrences. Based on the results of this cohort, the hernia patch is a feasible method to repair a small primary umbilical hernia. The preferred location of the mesh cannot be stated based on the results of this cohort. Finally, for specific patient groups, such as patients with an umbilical hernia larger than 4 cm, patients with rectus diastasis or overweight patients, other surgical options should be considered as well.
Statements
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the ethics committee of Northern Ostrobothnia Hospital District 12 April, 2021. According to local legislation a patient’s written consent is not required in this registry study.
Author contributions
JH: study design, data collection, data interpretation, manuscript development, and manuscript review. MA: study design, manuscript development, and manuscript review. EM: study design, manuscript development, and manuscript review. PO: study design, statistical analysis plan, manuscript development, and manuscript review. JS: study design, manuscript development, and manuscript review. TR: study design, manuscript development, and manuscript review. All authors contributed to the article and approved the submitted version.
Funding
This study is investigator-initiated and received funding from a Finnish government research grant.
Conflict of interest
EM previously was paid a consultancy fee from Medtronic.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
AHS, American hernia society; ASA, American society of anesthesiologists; BMI, body mass index; EHS, European hernia society; SD, standard deviation; SSI, surgical site infection; SSO, surgical site occurrence; SSOPI, surgical site occurrence requiring intervention.
References
1.
Muysoms FE Miserez M Berrevoet F Campanelli G Champault GG Chelala E et al Classification of Primary and Incisional Abdominal wall Hernias. Hernia (2009) 13(4):407–14. 10.1007/s10029-009-0518-x
2.
Kaufmann R Halm JA Eker HH Klitsie PJ Nieuwenhuizen J van Geldere D et al Mesh versus Suture Repair of Umbilical Hernia in Adults: a Randomised, Double-Blind, Controlled, Multicentre Trial. The Lancet (2018) 391(10123):860–9. 10.1016/S0140-6736(18)30298-8
3.
Madsen LJ Oma E Jorgensen LN Jensen KK . Mesh versus Suture in Elective Repair of Umbilical Hernia: Systematic Review and Meta-Analysis. BJS Open (2020) 4:369–79. 10.1002/bjs5.50276
4.
Henriksen NA Montgomery A Kaufmann R Berrevoet F East B Fischer J et al Guidelines for Treatment of Umbilical and Epigastric Hernias from the European Hernia Society and Americas Hernia Society. Br J Surg (2020) 107:171–90. 10.1002/bjs.11489
5.
Berrevoet F Doerhoff C Muysoms F Hopson S Muzi MG Nienhuijs S et al Open Ventral Hernia Repair with a Composite Ventral Patch - Final Results of a Multicenter Prospective Study. BMC Surg (2019) 19(1):93. 10.1186/s12893-019-0555-z
6.
Porrero JL Cano-Valderrama O Villar S Sánchez-Cabezudo C Ramos B Porrero B et al Umbilical Hernia Repair with Composite Prosthesis: a Single-centre Experience. Hernia (2019) 23(1):143–7. 10.1007/s10029-018-1843-8
7.
García-Moreno F Sotomayor S Pérez-López P Pérez-Köhler B Bayon Y Pascual G et al Intraperitoneal Behaviour of a New Composite Mesh (ParietexTM Composite Ventral Patch) Designed for Umbilical or Epigastric Hernia Repair. Surg Endosc (2014) 28(12):3479–88. 10.1007/s00464-014-3633-4
8.
Ponten JEH Leclercq WKG Lettinga T Heemskerk J Konsten JLM Bouvy ND et al Mesh or Patch for Hernia on Epigastric and Umbilical Sites (MORPHEUS-Trial): The Complete Two-Year Follow-Up. Ann Surg (2019) 270(1):33–7. 10.1097/SLA.0000000000003086
9.
Tsapralis D Vasiliades G Zaxou Z Delimpaltadaki M Margetousakis TH Papadakis H et al Bowel Obstruction Secondary to Migration of a Ventralex Mesh: Report of a Rare Complication. Hernia (2018) 22(4):711–4. 10.1007/s10029-017-1720-x
10.
Ambe P Meyer A Köhler L . Repair of Small and Medium Size Ventral Hernias with a Proceed Ventral Patch: A Single center Retrospective Analysis. Surg Today (2013) 43(4):381–5. 10.1007/s00595-012-0245-2
11.
Agca B Iscan Y . Comparison of Intraperitoneal Ventralex ST Patch versus Onlay Mesh Repair in Small and Medium Primer Umbilical Hernia. Int J Abdom Wall Hernia Surg (2019) 2(1):1. 10.4103/ijawhs.ijawhs_24_18
12.
Rajwade BK Patel RV Jain YD Bhoge RP Sharma PP . Ventral Hernia Repair Using Ventralex® ST Patch: A Single-Center Study of Clinical Outcomes and Complications. Cureus (2022) 14:e29341. 10.7759/cureus.29341
13.
Tollens T Den Hondt M Devroe K Terry C Speybroeck S Aelvoet C et al Retrospective Analysis of Umbilical, Epigastric, and Small Incisional Hernia Repair Using the VentralexTM Hernia Patch. Hernia (2011) 15(5):531–40. 10.1007/s10029-011-0816-y
14.
Martin DF Williams RF Mulrooney T Voeller GR . Ventralex Mesh in Umbilical/epigastric Hernia Repairs: Clinical Outcomes and Complications. Hernia (2008) 12(4):379–83. 10.1007/s10029-008-0351-7
15.
Kulacoglu H . Comment to: Umbilical hernia repair with composite prosthesis—a single-center experience. Porrero JL, Cano-Valderrama O, Villar S, et al. Hernia (2020) 24:225–6. 10.1007/s10029-019-01980-2
16.
Henriksen NA Jensen KK Bisgaard T Helgstrand F, the Danish Hernia Database. Suture or Mesh Repair of the Smallest Umbilical Hernias: A Nationwide Database Study. World J Surg (2022) 46(8):1898–905. 10.1007/s00268-022-06520-1
17.
Martin-del-Campo LA Miller HJ Elliott HL Novitsky YW . Laparoscopic Ventral Hernia Repair with and without Defect Closure: Comparative Analysis of a Single-Institution Experience with 783 Patients. Hernia (2018) 22(6):1061–5. 10.1007/s10029-018-1812-2
18.
Tandon A Pathak S Lyons NJR Nunes QM Daniels IR Smart NJ . Meta-analysis of Closure of the Fascial Defect during Laparoscopic Incisional and Ventral Hernia Repair. Br J Surg (2016) 103:1598–607. 10.1002/bjs.10268
19.
Porrero JL Cano-Valderrama O Castillo MJ Marcos A Tejerina G Cendrero M et al Importance of Mesh Overlap on Hernia Recurrence after Open Umbilical Hernia Repair with Bilayer Prosthesis. Am J Surg (2018) 216(5):919–22. 10.1016/j.amjsurg.2018.01.041
20.
Gillion JF Dabrowski A Jurczak F Dugue T Bonan A Chollet JM . Patient-reported Outcome Measures 2 Years after Treatment of Small Ventral Hernias Using a Monofilament Polypropylene Patch Covered with an Absorbable Hydrogel Barrier on its Visceral Side. Int J Abdom Wall Hernia Surg (2018) 1(3):99. 10.4103/ijawhs.ijawhs_20_18
Summary
Keywords
recurrence, umbilical hernia, umbilical hernia repair, ventral patch, hernia patch
Citation
Hiekkaranta JM, Ahonen M, Mäkäräinen E, Ohtonen P, Saarnio J and Rautio T (2023) Ventralex™ ST Hernia Patch Repair for Small Umbilical Hernia is Safe and Effective: A Retrospective Cohort Study. J. Abdom. Wall Surg. 2:11499. doi: 10.3389/jaws.2023.11499
Received
20 April 2023
Accepted
24 May 2023
Published
02 June 2023
Volume
2 - 2023
Updates
Copyright
© 2023 Hiekkaranta, Ahonen, Mäkäräinen, Ohtonen, Saarnio and Rautio.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Juha M. Hiekkaranta, juha.hiekkaranta@kainuu.fi
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.