- 1Department of Colorectal Surgery, Cardiff and Vale University Health Board, Cardiff, United Kingdom
- 2Real-World Evidence, OPEN Health, Marlow, United Kingdom
- 3Market Access, Becton Dickinson Surgery UK, Wokingham, United Kingdom
Background: Incisional hernia (IH) is a common complication of abdominal surgery affecting between 12.8% and 30% of patients. In spite of this, rates of IH repair remain low, at around 5% in the literature. We aimed to assess the rate of IH repair in the UK across surgical specialties and the cost burden associated with IH repair.
Methods: This is a retrospective observational study of patients undergoing abdominal surgery in England between 2012 and 2022 using the Hospital Episode Statistics (HES) database. Index abdominal surgery was identified between March 2014 and March 2017. Diagnostic and surgical procedure codes were used to identify pre-operative risk factors, index surgeries, IH repair and healthcare contact. Healthcare resource use (HCRU) costs were derived for index surgery and all post-index, non-elective inpatient admissions and outpatient visits using Healthcare Resource Group (HRG) codes within HES.
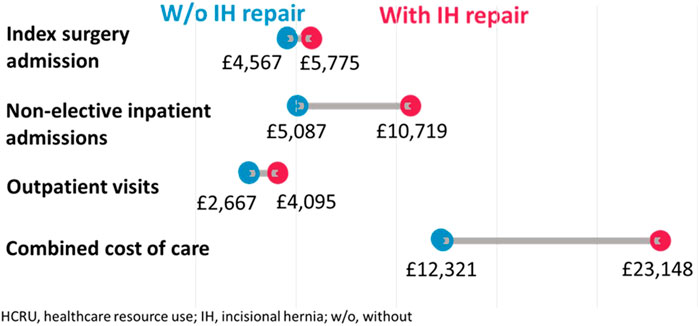
Results: Of 297,134 patients undergoing abdominal surgery, 5.1% (n = 15,138) subsequently underwent incisional hernia repair. By specialty, rates were higher in Colorectal (10.0%), followed by Hepatobiliary (8.2%), Transplant (6.8%), Urological (4.0%), Bariatric (3.5%), Vascular (3.2%) and Gynaecological (2.6%) surgery. Patients undergoing IH repair had more healthcare contacts, longer length of inpatient stays and more A+E visits vs. those with no IH repair post index surgery (83% ≥ 1 A+E visit vs. 69%), as well as higher rates of referral to mental health services (19.8% vs. 11.5%). IH repair was associated with an average HCRU cost of £23,148 compared to £12,321 in patients with no IH repair.
Conclusion: Patients undergoing IH repair have a greater morbidity than those not undergoing repair, shown by higher HCRU and more healthcare contacts. Despite this, rates of surgery for IH are low, suggesting that most patients with hernias are not undergoing repair. Emphasis must be placed squarely on primary prevention, rather than cure.
Introduction
Incisional hernia (IH) is a common complication of abdominal surgery, affecting 12.8%–30% of patients [1, 2]. Risk factors for developing IH include, but are not limited to, increasing age, obesity, smoking, location of surgical incision, suture material and closure technique [1, 3–6]. Extensive research has focussed on prevention of IH and risk reduction strategies, yet despite use of these interventions, incidence of incisional hernia remains at 10%–13% [3, 7, 8].
The impact of incisional hernia to both patients and healthcare services should not be overlooked. Patients with incisional hernia report significantly lower quality of life and body image scores compared to patients without [9]. Furthermore, operative repair of incisional hernia is challenging, carrying high recurrence rates and an overall mortality rate of 1% [10, 11]. Patients undergoing repair of incisional hernia may enter a vicious cycle of recurrence and re-operation with increasingly poor outcomes with each attempt [12]. The cost of this to healthcare services is significant, with hernia-related healthcare expenditure in the United States reaching $3.2 billion dollars annually [12, 13].
Prevention of incisional hernia is of the utmost importance in reducing the associated morbidity and cost of incisional hernia. Recent techniques such as the small stitch technique and mesh prophylaxis have shown promising results, yet widespread uptake both remains low [14]. Attitudes towards abdominal wall closure following abdominal surgery potentially reflect a misunderstanding about the burden of incisional hernia to patients and healthcare services.
This study aims to quantify the incidence of incisional hernia repair following open abdominal surgery and the impact of incisional hernia to patients and healthcare services in England.
Methods
This was a retrospective observational study using population level data taken from the Hospital Episode Statistics (HES) database. The primary objective of this study was to describe the rate of incisional hernia repair following open abdominal surgery. Secondary objectives include the rate of IH repair according to surgical specialty, identifying risk factors for subsequent IH repair and the healthcare resource usage (HCRU) and cost associated with IH repair.
HES Database
HES is a data warehouse containing records of all patients admitted to NHS hospitals in England [15]. The HES database contains data on hospital diagnoses, procedures, treatment, healthcare resource use (including inpatient admissions [elective and non-elective], outpatient visits, and accident and emergency [A&E] visits). Associated Healthcare Resource Group (HRG) codes are also recorded in HES to track the activity-based income received by hospitals in England for given HCRU [16].
For this study access to HES was provided under licence via Harvey Walsh Ltd. (operating as OPEN Health Ltd.) from NHS Digital. Data Sharing Agreement: DARS-NIC-05934-M7V9K. Copyright © 2023, NHS Digital. Re-used with the permission of NHS Digital. All rights reserved. Harvey Walsh Ltd. follow NHS Digital HES Analysis Guidelines and required security policies to ensure that data was handled appropriately.
Patient Selection: Identification of Index Surgery and Incisional Hernia
This study included patients with an Office of Population Censuses and Surveys Classification of Surgical Operations and Procedures 4th Revision (OPCS-4) code recorded within an inpatient admission for intra-abdominal, urologic or gynaecologic surgery in HES between 1st April 2014 and 31st March 2017. A list of OPCS codes used can be seen in Supplementary Appendix SX. The first such surgery within this period was termed the patient’s “Index Surgery.” Electronic medical records (EMR) in HES between 1st June 2012 and 30th June 2022 were used to identify risk factors at index surgery, comorbidities, post-index HCRU and incisional hernia repair. Patients were excluded if they had less than 12 months follow up, had an incisional hernia repair prior to or during their index surgery, had multiple surgical specialties at the time of index surgery, or who had a caesarean section recorded at any time.
Patients identified as undergoing index surgery were further categorised into two sub-cohorts: Those with incisional hernia repair post-index surgery (termed IH repair); defined by the presence of both an ICD-10 code for abdominal hernia and an OPCS-4 procedure code for IH repair within the same HES inpatient admission (see Supplementary Appendix SX for code list), which was used as a surrogate for incisional hernia, and those who did not fit the above criteria (termed no IH repair).
Identification of Pre- and Post-Index Surgery Variables
International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10) codes were used to identify relevant pre-operative risk factors recorded in HES at the time of index surgery and post-operative complications. If an IH repair was recorded post index surgery, only post-operative complications recorded prior to the IH repair were included.
HES data was used to identify scheduled and unscheduled secondary care encounters including elective and non-elective inpatient admissions, outpatient visits and A&E attendance. Length of stay (LOS) was calculated as the duration of each unique non-elective inpatient admissions in days.
HCRU costs were derived by mapping HRG codes to Payment by Results (PbR) NHS National Tariff Workbooks of costs for the applicable financial year of resource use [17]. All-cause HCRU costs were defined per patient as the cumulative cost of index surgery, and all post-index inpatient admissions (elective and non-elective) and outpatient visits within the study period.
Statistical Analysis
Statistical analysis was completed using R version 4.2.2 (R Core Team, 2022). Rates of IH repair were calculated as a percentage of patients undergoing a post-index IH repair over the total population of patients with an index surgery of interest recorded between 1st April 2014 and 31st March 2017.
In addition, separate univariate Cox proportional hazard (PH) models were used to determine the incidence risk of IH repair from index surgery for pre-operative risk factors of interest with hazard ratios (HRs) with 95% confidence intervals (95% CIs) and associated p-values presented. Person-years at risk was calculated from index surgery until earliest of first IH repair recorded, patient death, emigration from England or end of the study period (30th June 2022).
Descriptive statistics were used to describe post-index surgery complications and HCRU.
Small number suppression (i.e., events with <7 occurrences are replaced with a “*”) was conducted in line with NHS digital guidance to prevent inadvertent patient identification [18].
Results
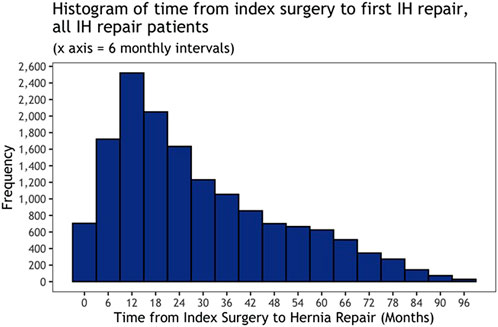
A total of 297,134 patients were included in the study who had undergone abdominal surgery between 1st April 2014 and 31st March 2017 and were followed up for a median time of 6.5 years following that index surgery. Of those, 5.1% (n = 15,138) underwent subsequent operative repair of incisional hernia. There were no recorded instances of patients having prophylactic mesh placement at the time of their index surgery. When analysed by index surgical specialty, colorectal surgery had the highest rates of incisional hernia repair at 10.0%, with gynaecological surgery having the lowest rates at 2.6%. A complete breakdown can be seen in Table 1. The median time from index surgery to incisional hernia repair was 24 months (Interquartile range [IQR] 13.42), patients most commonly underwent IH repair within the first 18 months following index surgery (Figure 1).
Risk Factors for IH Repair
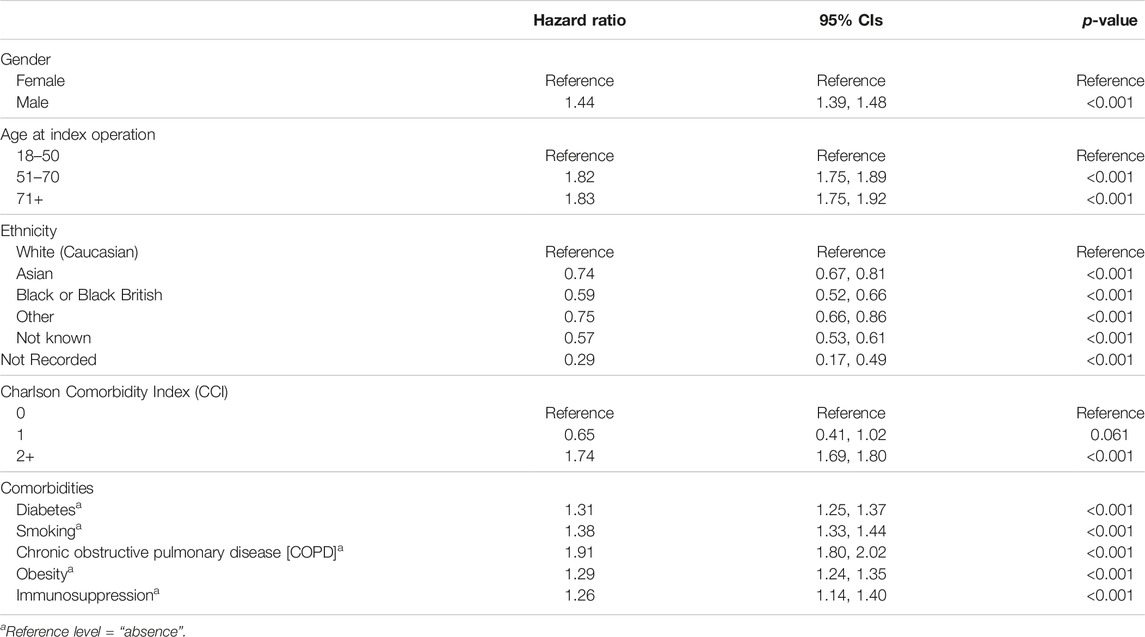
Patients undergoing incisional hernia repair had higher rates of diabetes (15.2% vs. 12.5%), smoking (23.5% vs. 18.1%), Chronic Obstructive Pulmonary Disease (COPD) (8.6% vs. 5.1%) and obesity (18.7% vs. 14.7%) at time of their index surgery when compared to patients who did not have IH repair. Univariate analysis of pre-operative risk factors revealed that patients older at index surgery (>50 years of age) (HR: 1.82, 95% CIs: 1.75–1.89, p < 0.001), male (HR: 1.44, 95% CIs: 1.39–1.48, p < 0.001) and with COPD (HR: 1.91, 95% CIs: 1.80–2.02, p < 0.001) had the greatest risk of requiring subsequent incisional hernia repair (see Table 2 for more information).
Post-Operative Complications
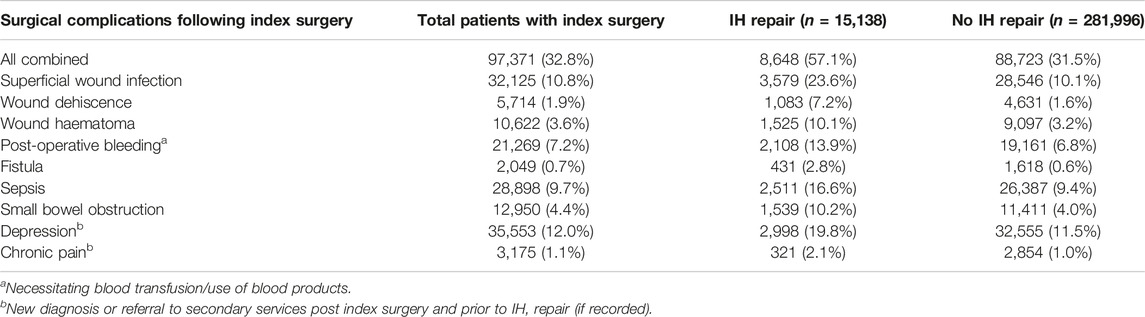
Of all patients undergoing abdominal surgery, 32.8% (97,371) experienced a postoperative complication, breakdowns of which can be seen in Table 3. Following index surgery, patients who went on to have incisional hernia repair had experienced higher rates of surgical site infection (23.6% vs. 10.1%), wound dehiscence (7.2% vs. 1.6%), bleeding (necessitating blood transfusion) (13.9% vs. 6.8%), fistulation (2.8% vs. 0.6%), small bowel obstruction (10.2% vs. 4.0%). This translated to a longer median length of stay (LOS) at index surgery (7 days [IQR: 4.13] vs. 3 days [IQR: 2.7]) for patients who would have a future repair. Patients undergoing IH repair had higher rates of referral to mental health services (19.8% vs. 11.5%), and chronic pain services (2.1% vs. 1.0%) in the follow-up period compared to patients who did not have IH repair.
Healthcare Resource Usage and Costs
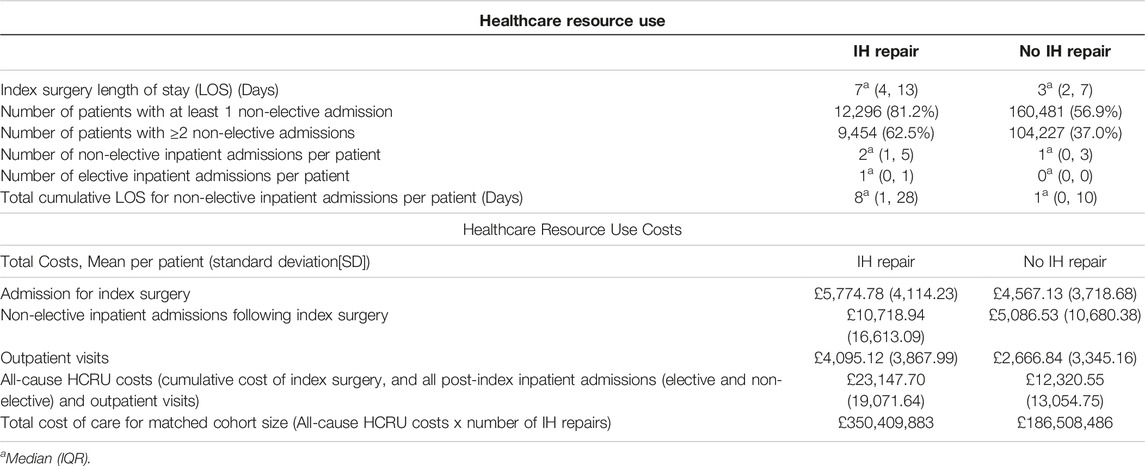
Table 4 shows the differing healthcare-related attendances between those undergoing IH repair and those who did not, alongside associated costs. In the period following index surgery, 62.5% of patients with an IH repair had ≥2 non-elective admissions to hospital, with the median number of non-elective admissions being 2 (IQR: 1.5) vs. 37.0% of patients without a post-index IH repair, with the median number of non-elective admissions being 1 (IQR: 0.3) in these patients. The median cumulative LOS per patient for non-elective inpatient admissions was 8 days (IQR: 1, 28) in patients with an IH repair and 1 day (IQR: 0, 10) in patients with no repair post index surgery.
Patients who underwent IH repair averaged total costs of £23,147 per patient (pp) in the follow-up period between index surgery and IH repair, compared to £12,320pp in those who did not undergo IH repair (Figure 2). The average cost of an operative IH repair admission was £2,155pp. The total cost of care in patients undergoing IH repair was £350,414,424 compared to £186,515,298 when matching cohort sizes; a cost-difference of £163,899,126. A complete breakdown of healthcare usage and cost can be seen in Table 4.
Discussion
This retrospective review of population-level data from England describes the post-operative journey that patients undergo following abdominal surgery in England. A recent publication from the French national database estimated the cost of incisional hernia repair to be €4,153 per repair, in keeping with other publications [11]. Our paper is the first, however, to describe the morbidity and cost incurred to patients between their index surgery and repair.
Our results demonstrate that 5% of all patients undergoing abdominal surgery will undergo subsequent repair of incisional hernia. This figure is identical to data published from the French national database by Gignoux et al., who demonstrated a re-operation rate of 5% over a 5-year follow-up period, alongside data from a systematic review by Bosanquet et al which reported the risk of undergoing IH repair of 5.2% [1, 19]. Surgical specialties with higher rates of IH included Colorectal, Hepatobiliary and Transplant surgery, with lower rates identified in Urologic, Bariatric, Vascular and Gynaecologic surgery.
Higher rates of IH repair in colorectal and transplant patients are consistent with the findings of Basta et al., who reported rates of 7.7% and 4.8%, respectively [10]. Hernia repair has traditionally been the bastion of the general surgeon, and higher rates of hernia repair in the general surgical subspecialties may simply be due to increased awareness and early detection, without the delays of referral to another specialty. This is supported by lower-than-expected rates of repair in non-general surgical specialties such as Gynaecology and Urology.
Patients undergoing vascular surgery, specifically aortic surgery, are at increased risk of incisional hernia development, so it is perhaps surprising to see lower rates of incisional hernia repair than average in our cohort [20]. The reasons for this are not immediately apparent but may reflect a more comorbid population group that are unfit for subsequent incisional hernia repair.
In this study, the median time between index surgery and IH repair was 24 months, similar to figured reported by Kockerling et al. in 2015, in which 50% of recurrent incisional hernias had been repaired within 2 years of index surgery [21]. The risk of incisional hernia development continues up to 3 years post-surgery, implying a trend of intervention in early, smaller incisional hernias, rather than chronic complex hernias [22]. Whether this is the case or if this impacts subsequent hernia recurrence rates is beyond the scope of this study.
This paper demonstrates that patients undergoing incisional hernia repair have increased rates of complications after their index surgery, such as surgical site infection, wound dehiscence and fistulation compared to patients that do not undergo repair. Incisional hernia occurs as a result of failure of the abdominal wall to heal. SSI, dehiscence and fistulation represent impaired wound healing and have been recognised in the literature as risk factors for IH development [23–25]. In our cohort, 19.8% of patients undergoing IH repair were referred to mental health services in the time period between index surgery and IH repair. Van Ramshorst et al. in 2012 demonstrated lower quality of life and body image scores in patients with incisional hernia compared to those without, yet there was no difference in scores for mental health between the two groups [9]. The link between IH and referral to mental health services in our results is not clear; the differing rates of in our study may reflect the impact that post-operative complications have on the patient rather than being attributed to the hernia alone. Nonetheless, our data supports the importance of “getting it right first time” both in terms of reducing post-operative complications and subsequent impact on patient wellbeing.
Given that patients undergoing IH repair have higher rates of post-operative complications, it is perhaps not surprising that healthcare associated resource use is higher in this group of patients than in those with no repair. Increased post-operative length of stay, and more unplanned hospital attendances, translates to an average cost difference of £10,827 per patient between each group, and a matched cohort-size cost difference of over £163 million. Consistent with the findings reported in this manuscript, a cost analysis of incisional hernia in a population of US patients published by Fischer et al. demonstrated higher average readmission costs in patients with hernia, as well as higher combined costs of care ($41,053 vs. $81,183, p < 0.001) [13]. The costs described in our paper exclude those of the incisional hernia repair and subsequent care and suggest that the financial burden of incisional hernia is greater still.
There are limitations to our study, chiefly the use of incisional hernia repair as a surrogate for diagnosis of incisional hernia. As previously mentioned, rates of incisional hernia vary from 12.8% to 30% in the literature, therefore our rate of repair is an underestimate of the true rate of herniation in our cohort. Further work is needed to identify and chart the morbidity, cost and decision making in patients diagnosed with IH who do not undergo operative repair, as it appears that it is the minority of patients who undergo IH repair. Another limitation is the inability to draw cause and effect between cost, attendances, and IH repair. Our data demonstrates that most of the cost difference is in non-elective admissions. Whether these admissions are related to the incisional hernia itself, or as a consequence of the increased rates of post-operative complications is not clear, and further work in this area is needed. Nonetheless, the risk of needing IH repair is increased in patients who suffer complications following their index surgery. Focus should be on prevention of not just incisional hernia at index surgery, but also on the post-operative complications, such as SSI and wound dehiscence that correlate with increased incisional hernia rates.
This study highlights that 5% of all patients undergoing abdominal surgery will undergo further surgery to repair incisional hernia, and charts what happens to these patients before they undergo their repair. In order to reduce the risk of IH and the burden to both patients and healthcare services, the focus needs to be on prevention. Implementation of current European and American Hernia society guidance, alongside pre-operative risk assessment and targeted mesh-augmented abdominal wall closure will reduce incidence of IH but need to be combined with broader national improvement programmes such as “Getting It Right First Time” (GIRFT) in order to reduce variation in all aspects of post-operative surgical care, across surgical specialties [7, 26]. Prevention of incisional hernia should not be the focus of one surgical specialty and further work is needed to raise awareness of this issue and the issue of prevention outside of the traditional hernia specialties.
Conclusion
Patients undergoing abdominal surgery are at risk of developing incisional hernia, regardless of surgical specialty. Patients who undergo repair of IH are more likely to have increased rates of post-operative complications and have higher rates of healthcare usage and costs of care compared to patients who do not undergo surgery.
This paper is the first to attempt to map the patient journey between index surgery and first IH repair, but further work is needed to identify the missed majority of patients with incisional hernia who do not undergo repair. Urgent strategies to change practice and implement prevention guidelines are needed to reduce the burden of morbidity and cost associated with IH repair.
Data Availability Statement
The datasets presented in this article are not readily available as they were retrieved from the Hospital Episodes Statistics (HES) Database; NHS Digital. Information about how to access this database can be found at digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics/users-uses-and-access-to-hospital-episode-statistics.
Ethics Statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and the institutional requirements.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
The authors declare that this study received funding from Becton Dickinson Surgery UK. The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of Interest
Authors EW, CR, and PW are employed by OPEN Health. Author PB is employed by Becton Dickinson Surgery UK.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
Data access and running of the analysis would have not been made possible without facilitation by Dave Heaton (Open Health). The initial study concept was discussed in part also with Myriam Alexander (Open Health). This study has been presented as a poster at the ESCP’s 18th Scientific and Annual Conference [27].
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontierspartnerships.org/articles/10.3389/jaws.2024.12452/full#supplementary-material
References
1. Bosanquet, DC, Ansell, J, Abdelrahman, T, Cornish, J, Harries, R, Stimpson, A, et al. Systematic Review and Meta-Regression of Factors Affecting Midline Incisional Hernia Rates: Analysis of 14 618 Patients. PLoS One (2015) 10:e0138745. doi:10.1371/journal.pone.0138745
2. Torkington, J, Harries, R, and O’Connell, S Incisional Hernia Following Colorectal Cancer Surgery According to Suture Technique: Hughes Abdominal Repair Randomized Trial (HART). Br J Surg (2022) 109:943–50. doi:10.1093/bjs/znac198
3. Deerenberg, EB, Harlaar, JJ, Steyerberg, EW, Lont, HE, van Doorn, HC, Heisterkamp, J, et al. Small Bites Versus Large Bites for Closure of Abdominal Midline Incisions (STITCH): A Double-Blind, Multicentre, Randomised Controlled Trial. The Lancet (2015) 386:1254–60. doi:10.1016/S0140-6736(15)60459-7
4. Höer, J, Lawong, G, Klinge, U, and Schumpelick, V. Einflussfaktoren der Narbenhernienentstehung Retrospektive Untersuchung an 2.983 Laparotomierten Patienten Über Einen Zeitraum von 10 Jahren. Der Chirurg (2002) 73:474–80. doi:10.1007/s00104-002-0425-5
5. Sørensen, LT, Hemmingsen, UB, Kirkeby, LT, Kallehave, F, and Jørgensen, LN. Smoking Is a Risk Factor for Incisional Hernia. Arch Surg (2005) 140:119–23. doi:10.1001/archsurg.140.2.119
6. den Hartog, FPJ, van Egmond, S, Poelman, MM, Menon, AG, Kleinrensink, GJ, Lange, JF, et al. The Incidence of Extraction Site Incisional Hernia After Minimally Invasive Colorectal Surgery: A Systematic Review and Meta-Analysis. Colorectal Dis (2023) 25:586–99. doi:10.1111/codi.16455
7. Deerenberg, EB, Henriksen, NA, Antoniou, GA, Antoniou, SA, Bramer, WM, Fischer, JP, et al. Updated Guideline for Closure of Abdominal Wall Incisions From the European and American Hernia Societies. Br J Surg (2022) 109:1239–50. doi:10.1093/bjs/znac302
8. Jairam, AP, Timmermans, L, Eker, HH, Pierik, REGJM, van Klaveren, D, Steyerberg, EW, et al. Prevention of Incisional Hernia With Prophylactic Onlay and Sublay Mesh Reinforcement Versus Primary Suture Only in Midline Laparotomies (PRIMA): 2-Year Follow-Up of a Multicentre, Double-Blind, Randomised Controlled Trial. The Lancet (2017) 390:567–76. doi:10.1016/S0140-6736(17)31332-6
9. van Ramshorst, GH, Eker, HH, Hop, WCJ, Jeekel, J, and Lange, JF. Impact of Incisional Hernia on Health-Related Quality of Life and Body Image: A Prospective Cohort Study. Am J Surg (2012) 204:144–50. doi:10.1016/j.amjsurg.2012.01.012
10. Basta, MN, Kozak, GM, Broach, RB, Messa, CA, Rhemtulla, I, DeMatteo, RP, et al. Can We Predict Incisional Hernia? Ann Surg (2019) 270:544–53. doi:10.1097/SLA.0000000000003472
11. Ortega-Deballon, P, Renard, Y, de Launay, J, Lafon, T, Roset, Q, and Passot, G. Incidence, Risk Factors, and Burden of Incisional Hernia Repair After Abdominal Surgery in France: A Nationwide Study. Hernia (2023) 27:861–71. doi:10.1007/s10029-023-02825-9
12. Fischer, JP, Basta, MN, Wink, JD, Krishnan, NM, and Kovach, SJ. Cost-Utility Analysis of the Use of Prophylactic Mesh Augmentation Compared With Primary Fascial Suture Repair in Patients at High Risk for Incisional Hernia. Surgery (2015) 158:700–11. doi:10.1016/j.surg.2015.02.030
13. Fischer, JP, Basta, MN, Mirzabeigi, MN, Bauder, AR, Fox, JP, Drebin, JA, et al. A Risk Model and Cost Analysis of Incisional Hernia After Elective, Abdominal Surgery Based Upon 12,373 Cases: The Case for Targeted Prophylactic Intervention. Ann Surg (2016) 263:1010–7. doi:10.1097/SLA.0000000000001394
14. Fischer, JP, Harris, HW, López-Cano, M, and Hope, WW. Hernia Prevention: Practice Patterns and Surgeons’ Attitudes About Abdominal Wall Closure and the Use of Prophylactic Mesh. Hernia (2019) 23:329–34. doi:10.1007/s10029-019-01894-z
15. Thorn, JC, Turner, E, Hounsome, L, Walsh, E, Donovan, JL, Verne, J, et al. Validation of the Hospital Episode Statistics Outpatient Dataset in England. Pharmacoeconomics (2016) 34:161–8. doi:10.1007/s40273-015-0326-3
16. Chapman, C, Laguecir, A, and Quentin, W. Management Accounting and Efficiency in Health Services: The Foundational Role of Cost Analysis. In: J Cylus, I Papanicolas, and P Smith, editors. Health System Efficiency. Geneva, Switzerland: WHO (2016). p. 75–98.
17. NHS Digital (2009) Sponsoring Organisation: Implementation Healthcare Resource Groups 4 (HRG4) DATA SET CHANGE NOTICE-OPCS Classification of Interventions and Procedures Version 4.4.
18. Herbert, A, Wijlaars, L, Zylbersztejn, A, Cromwell, D, and Hardelid, P. Data Resource Profile: Hospital Episode Statistics Admitted Patient Care (HES APC). Int J Epidemiol (2017) 46:1093–i. doi:10.1093/ije/dyx015
19. Gignoux, B, Bayon, Y, Martin, D, Phan, R, Augusto, V, Darnis, B, et al. Incidence and Risk Factors for Incisional Hernia and Recurrence: Retrospective Analysis of the French National Database. Colorectal Dis (2021) 23:1515–23. doi:10.1111/codi.15581
20. Antoniou, GA, Georgiadis, GS, Antoniou, SA, Granderath, FA, Giannoukas, AD, and Lazarides, MK. Abdominal Aortic Aneurysm and Abdominal Wall Hernia as Manifestations of a Connective Tissue Disorder. J Vasc Surg (2011) 54:1175–81. doi:10.1016/j.jvs.2011.02.065
21. Köckerling, F, Koch, A, Lorenz, R, Schug-Pass, C, Stechemesser, B, and Reinpold, W. How Long Do We Need to Follow-Up Our Hernia Patients to Find the Real Recurrence Rate? Front Surg (2015) 2:24. doi:10.3389/fsurg.2015.00024
22. Fink, C, Baumann, P, Wente, MN, Knebel, P, Bruckner, T, Ulrich, A, et al. Incisional Hernia Rate 3 Years After Midline Laparotomy. Br J Surg (2013) 101:51–4. doi:10.1002/bjs.9364
24. Tubre, DJ, Schroeder, AD, Estes, J, Eisenga, J, and Fitzgibbons, RJ. Surgical Site Infection: The “Achilles Heel” of All Types of Abdominal Wall Hernia Reconstruction. Hernia (2018) 22:1003–13. doi:10.1007/s10029-018-1826-9
25. Henriksen, NA, Helgstrand, F, Vogt, KC, Jorgensen, LN, Bisgaard, T, Danish Hernia, D, et al. Risk Factors for Incisional Hernia Repair After Aortic Reconstructive Surgery in a Nationwide Study. J Vasc Surg (2013) 57:1524–30. doi:10.1016/j.jvs.2012.11.119
26. Abercrombie, J, and Frcs, MB. General Surgery GIRFT Programme National Specialty Report GIRFT Clinical Lead for General Surgery. London: NHS England (2017).
Keywords: incisional hernia, incisional hernia prevention, outcomes, morbidity, incisional hernia repair
Citation: Smith L, Wilkes E, Rolfe C, Westlake P, Cornish J, Brooks P and Torkington J (2024) Incidence, Healthcare Resource Use and Costs Associated With Incisional Hernia Repair. J. Abdom. Wall Surg. 3:12452. doi: 10.3389/jaws.2024.12452
Received: 21 November 2023; Accepted: 06 February 2024;
Published: 28 February 2024.
Copyright © 2024 Smith, Wilkes, Rolfe, Westlake, Cornish, Brooks and Torkington. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Laurie Smith, bGF1cmllLnNtaXRoQHdhbGVzLm5ocy51aw==
†ORCID: Laurie Smith, orcid.org/0000-0003-0201-9373; Emily Wilkes, orcid.org/0000-0003-4294-6892; Julie Cornish, orcid.org/0000-0003-4360-4472; Jared Torkington, orcid.org/0000-0002-3218-0574
 Laurie Smith
Laurie Smith Emily Wilkes2†
Emily Wilkes2†