Until the end of the 20th century, the repair of incisional hernias (IH) by suture alone was an accepted practice with high recurrence rates reported in observational studies [1–3]. During that period, other observational studies showed lower recurrence rates by adding a permanent synthetic prosthesis to the repair [4–6]. In 2000, a pivotal study was published marking a significant shift in the surgical treatment of IH, being the first randomized analysis comparing the use of a permanent synthetic mesh versus no mesh and its impact on recurrence [7]. The initial results of this research were confirmed over the long term [8], demonstrating a meaningful lower recurrence of IH in patients where a permanent synthetic mesh was added [7, 8]. This initial randomized study strengthened the use of permanent prosthetic mesh as the treatment of choice in the surgical approach to IH. The widespread adoption of mesh in IH treatment likely led to the perception of this entity’s treatment (in terms of reducing recurrence) as a mechanical problem involving only the technical aspects of closing a defect, either with sutures, autologous plasty, or mesh [9]. However, voices soon advocated the view that hernia recurrence should be seen as a much more complex problem, where biology plays a decisive role [10, 11]. Following these arguments [10, 11], if the recurrence of an IH after mesh repair depends only on the technique, what would be the answer to the question: what happens if the process is standardized and excellence in practice is achieved? The answer could be represented by a two-dimensional Cartesian coordinate graph, showing an “S”-shaped curve (Figure 1A). Initially, a high level of variability in the results would be represented by a fluctuating line; over time, these fluctuations would decrease, indicating a more consistent process. Ultimately, the line would stabilize (i.e., plateau), indicating that the best possible results are being consistently achieved over time. However, when analyzing the general information from the literature data, this does not seem to be the case, with a different overall graph being observed (Figure 1B). Thus, in 2003 a population-based analysis (over 10,000 patients) evaluated temporal trends and outcomes after IH repair [12]. The graphs from the study showed a progressive increase in reoperations for IH over time, without a final “plateau” (i.e., recurrence stabilization). Interestingly, the progressive increase was for both patients operated on with and without mesh, with those receiving mesh having a later reintervention. These findings have been confirmed by more recent epidemiological analyses with data from registries [13]. The described context simply supports the considerations made two decades ago [10, 11]. The etiology of IH is multifactorial, and several factors beyond a mere technical aspect can get involved in the event of a recurrence. Furthermore, the use of mesh in IH repair may represent just a “delaying” strategy in the reappearance of IH. In conclusion, the current use of mesh in IH repair may be just a “palliative” treatment for a complex disorder.
FIGURE 1
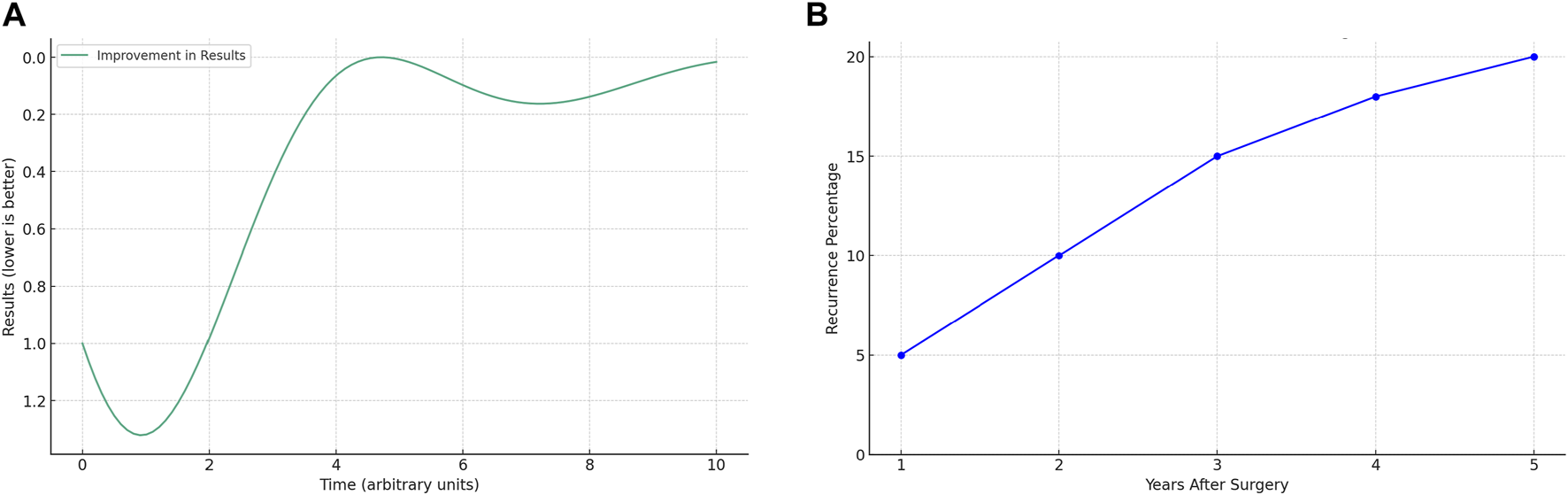
Curves of recurrence evolution: (A) Theoretical expected evolution after standardization; (B) General evolution observed in the literature data.
In our view, the previous argument not only affects the treatment of IH but can also be applied to its prevention. Thus, one of the most important studies regarding the prevention of IH with non-absorbable synthetic mesh after elective midline laparotomy shows similar long-term curves (5-year) [14]. Preventive mesh only delays the onset of IH. These same long-term results were previously observed in other similar works [15]. Moreover, when it comes to preventing IH with non-absorbable synthetic mesh after emergency midline laparotomy, the scarce long-term follow-up data also show a similar phenomenon where the mesh only delays the onset of the hernia [16]. Finally, it is interesting to note that other studies concerning the closure of the abdominal wall, where the efficacy of meshes in the treatment or prevention of IH is not evaluated, reveal similar curves. Specifically, a long-term analysis of the results of the application of the closure technique recommended in clinical guidelines (i.e., small bites) after both elective and emergency midline laparotomy [17, 18].
In summary, the recurrence of an IH after its treatment or prevention with a permanent synthetic mesh seems to represent only a “delaying” strategy in both elective and emergency surgery. Furthermore, there may be evidence that the closure of a midline laparotomy using the best technique currently recommended in clinical guidelines also only represents a “delaying” strategy in the onset of an IH.
A surgical technique of excellence is key in the outcomes of the treatment or prevention of an IH. However, it seems evident that IH is a complex biological problem. More investment is needed in fundamental research to increase the understanding of an IH genesis. Nevertheless, this fundamental research may take decades to be applied to daily practice, and for this reason, we believe that investment should also be made in clinical research with a view to improve current surgical approaches and prosthetic materials, with the aim of enhancing the best “delaying” strategies of the onset of an IH and preventing the deleterious effects that the footprint (i.e., recurrence, chronic pain, chronic infection, etc.) of techniques and materials can leave on our patients.
Statements
Author contributions
ML-C and JP contributed equally to the conception, drafting and review of this manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to acknowledge the assistance of ChatGPT (based on the GPT-4 model by OpenAI) in the editing and refinement of Figure 1.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Van der Linden FT Van Vroonhoven TJ . Long-Term Results After Surgical Correction of Incisional Hernia. Neth J Surg (1988) 40:127–9.
2.
Read RC Yoder G . Recent Trends in Management of Incisional Herniation. Arch Surg (1989) 124:485–8.
3.
Geçim IE Koçak S Ersoz S Bumin C Aribal D . Recurrence After Incisional Hernia Repair: Results and Risk Factors. Surg Today (1996) 26:607–9.
4.
Gillion JF Bégin GF Marecos C Fourtanier G . Expanded Polytetrafluoroethylene Patches Used in the Intraperitoneal or Extraperitoneal Position for Repair of Incisional Hernias of the Anterolateral Abdominal wall. Am J Surg (1997) 174:16–9.
5.
McLanahan D King LT Weems C Novotney M Gibson K . Retrorectus Prosthetic Mesh Repair of Midline Abdominal Hernia. Am J Surg (1997) 173:445–9.
6.
Arnaud JP Tuech JJ Pessaux P Hadchity Y . Surgical Treatment of Postoperative Incisional Hernias by Intraperitoneal Insertion of Dacron Mesh and an Aponeurotic Graft: A Report on 250 Cases. Arch Surg (1999) 134:1260–2.
7.
Luijendijk RW Hop WC Van den Tol MP De Lange DC Braaksma MM Ijzermans JN et al A Comparison of Suture Repair With Mesh Repair for Incisional Hernia. N Engl J Med (2000) 343:392–8.
8.
Burger JW Luijendijk RW Hop WC Halm JA Verdaasdonk EG Jeekel J . Long-Term Follow-Up of a Randomized Controlled Trial of Suture Versus Mesh Repair of Incisional Hernia. Ann Surg (2004) 240:578–83.
9.
Langer C Liersch T Kley C Flosman M Suss M Siemer A et al Twenty-Five Years of Experience in Incisional Herniasurgery. A Comparative Retrospective Study of Incisional Hernia Repairs of 432 Incisional Hernia Repairs. Chirurg (2003) 74:638–45.
10.
Klinge U Krones CJ . Can We Be Sure That the Meshes Do Improve the Recurrence Rates?Hernia (2005) 9(1):1–2. 10.1007/s10029-004-0294-6
11.
Klinge U Binnebösel M Rosch R Mertens P . Hernia Recurrence as a Problem of Biology and Collagen. J Minim Access Surg (2006) 2(3):151–4. 10.4103/0972-9941.27729
12.
Flum DR Horvath K Koepsell T . Have Outcomes of Incisional Hernia Repair Improved With Time? A Population-Based Analysis. Ann Surg (2003) 237(1):129–35. 10.1097/00000658-200301000-00018
13.
Kokotovic D Bisgaard T Helgstrand F . Long-Term Recurrence and Complications Associated With Elective Incisional Hernia Repair. JAMA (2016) 316(15):1575–82. 10.1001/jama.2016.15217
14.
Van den Dop LM Sneiders D Yurtkap Y Werba A van Klaveren D Pierik REGJM et al Prevention of Incisional Hernia With Prophylactic Onlay and Sublay Mesh Reinforcement vs. Primary Suture Only in Midline Laparotomies (PRIMA): Long-Term Outcomes of a Multicentre, Double-Blind, Randomised Controlled Trial. Lancet Reg Health Eur (2023) 36:100787. 10.1016/j.lanepe.2023.100787
15.
Caro-Tarrago A Olona C Millán M Olona M Espina B Jorba R . Long-Term Results of a Prospective Randomized Trial of Midline Laparotomy Closure With Onlay Mesh. Hernia (2019) 23(2):335–40. 10.1007/s10029-019-01891-2
16.
Bravo-Salva A Argudo-Aguirre N González-Castillo AM Membrilla-Fernandez E Sancho-Insenser JJ Grande-Posa L et al Long-Term Follow-Up of Prophylactic Mesh Reinforcement After Emergency Laparotomy. A Retrospective Controlled Study. BMC Surg (2021) 21(1):243. 10.1186/s12893-021-01243-x
17.
Deerenberg EB Henriksen NA Antoniou GA Antoniou SA Bramer WM Fischer JP et al Updated Guideline for Closure of Abdominal Wall Incisions From the European and American Hernia Societies. Br J Surg (2022) 109(12):1239–50. 10.1093/bjs/znac302
18.
Söderbäck H Masood A Leo J Sandblom G . Introduction of Small Stitch Small Bite Technique: A Retrospective Long-Term Follow-Up. Langenbecks Arch Surg (2022) 407(6):2527–35. 10.1007/s00423-022-02530-8
Summary
Keywords
hernia, incisional hernia, prevention, treatment, mesh
Citation
López-Cano M and Pereira JA (2024) Incisional Hernia Depends on More Than Just Mesh Placement. J. Abdom. Wall Surg. 3:12954. doi: 10.3389/jaws.2024.12954
Received
05 March 2024
Accepted
21 March 2024
Published
04 April 2024
Volume
3 - 2024
Updates
Copyright
© 2024 López-Cano and Pereira.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: M. López-Cano, 27689mlc@comb.cat
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.