- 1Department of General Surgery, Tameside General Hospital, Ashton-Under-Lyne, United Kingdom
- 2Department of Gastrointestinal Surgery, Royal Sussex County Hospital, Brighton, United Kingdom
- 3Department of Colo-Rectal Surgery, Worthing Hospital, Worthing, United Kingdom
Objective: The objective of this meta-analysis is to compare the perioperative surgical outcomes and cost-effectiveness of robotic ventral hernia repair (RVHR) versus laparoscopic ventral hernia repair (LVHR) with intraperitoneal mesh.
Methods: Randomised control trials (RCTs) reporting perioperative outcomes and costs in patients undergoing RVHR versus LVHR were selected from medical electronic databases and meta-analysis was conducted in accordance with the guidelines of the Cochrane Collaboration using statistical software RevMan version 5.
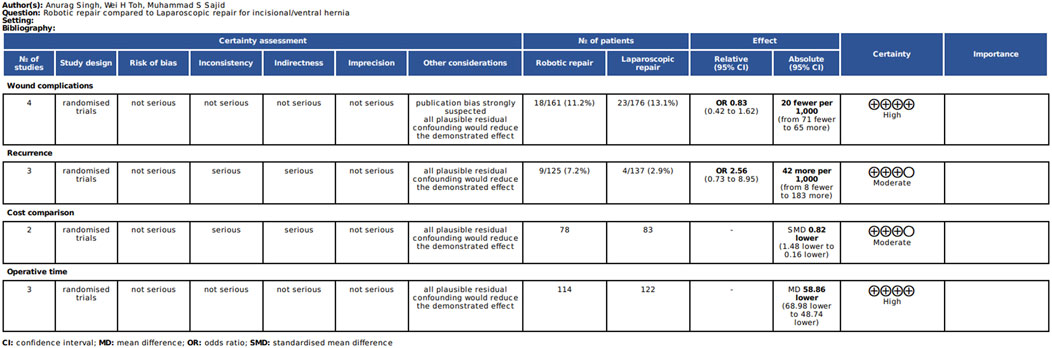
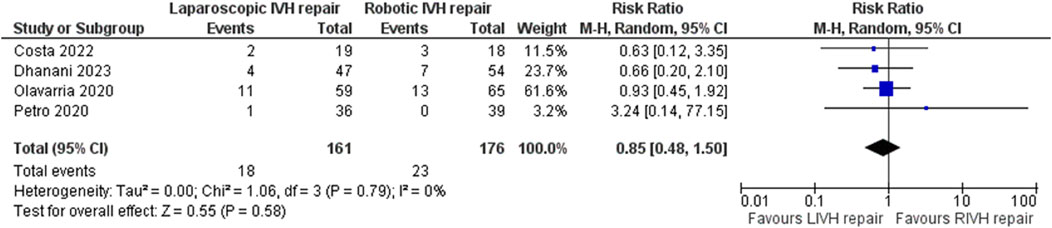
Results: Four RCTs on 337 patients reporting perioperative outcomes and cost comparison were included. In the random effect model analysis, the duration of operation was shorter, and cost was lower in the LVHR group but with significant statistical heterogeneity [standardized mean difference (SMD) −48.07, 95%, CI (−78.06, −18.07), Z = 3.14, P = 0.002], [SMD 0.82, 95%, CI (−1.48, −0.16), Z = 2.45, P = 0.01]. However, the variables of hernia recurrence and surgical site complications were statistically similar in both groups without any statistical heterogeneity among the included studies [Risk Ratio (RR) 1.05, 95%, CI (0.22, 4.99), Z = 0.06, P = 0.95], [RR 0.85, 95%, CI (0.48, 1.50), Z = 0.55, P = 0.58].
Conclusion: This systematic review demonstrates that RVHR does not offer any superiority among the compared perioperative variables (Duration of operation, hernia recurrence and surgical site complications) and it is not cost-effective when compared to LVHR. Due to the paucity of the RCTs and significant heterogeneity among the compared variables, a major multi-centre RCT is needed to validate these findings.
Introduction
A ventral hernia is one of the most common presentations among the patients encountered by the surgeons and the general practitioner [1]. In the UK alone around 100,000 abdominal wall hernia surgeries are repaired annually [2] which includes a significant proportion of ventral hernias (VH). The operative management of VH can be challenging due to the diversity of surgical approaches (open repair, laparoscopic repair, robotic repair), techniques of mesh fixation, size of the defect and implantation of a wide variety of biological or synthetic meshes necessary to achieve desired outcomes of minimum hernia recurrence risk and other post-operative complications such as surgical site infection, haemorrhage and enterocutaneous fistula [3]. Prior to the 1990s, VH repairs were primarily done through an open approach [4]. With the advent of the laparoscopic approach, surgeons utilised this approach to reduce the risk of hernia recurrence and postoperative surgical site infections with better health-related quality of life. Nonetheless, the laparoscopic approach is associated with a few drawbacks, primarily poor views due to intra-abdominal adhesions and reduced manoeuvrability of laparoscopic instruments [5].
The first documented use of the robotic approach for surgical procedures was reported in the year 2000 [6]. The use of a robotic approach for the surgical resections of urological malignancies and gynaecological malignancies has been a common practice in the last two decades with variable and diverse outcomes [7, 8]. Published studies have reported favourable outcomes for robotic ventral hernia repair (RVHR) compared to the relatively conventional approach of laparoscopic ventral hernia repair (LVHR) There are several studies reported in the literature demonstrating the superiority of the robotic approach for ventral hernia repair over the laparoscopic approach [7–9]. Due to the extra cost involved in performing the robotic procedures, there has always existed a debate among hernia surgeons about the effectiveness of the robotic approach. Primary variables such as duration of operation, blood loss, bowel injury, length of hospital stay, hernia recurrence, post-operative wound-related and systemic complications may well be similar in RVHR versus LVHR but secondary or tertiary variables like extra cost of the procedure and similar postoperative health-related quality of life seem to be a limiting factor in the use of robotic approach in the management of VH. The objective of this meta-analysis is to compare the perioperative surgical outcomes and cost-effectiveness of RVHR versus LVHR and report.
Methods
Data Sources and Literature Search Technique
This meta-analysis has been registered with the research registry reviewregistry1726. Electronic databases PubMed, EMBASE, MEDLINE and the Cochrane Library were reviewed and carefully searched. Relevant articles were identified with the use of MeSH terms (Robotic hernia repair, Laparoscopic hernia repair, Ventral hernia repair) and Boolean operators (AND, OR) and PICO approach was used to systematically refine and narrow down the search results. The references were further searched to identify the relevant articles for a detailed analysis.
Trial Selection
The inclusion criteria for the systematic review was the randomised control trials (RCTs) comparing RVHR against LVHR, reporting perioperative outcomes and cost analysis. All trials regardless of their language of publication and number of recruited patients were deemed suitable for inclusion.
Data Collection and Management
The published data was searched and collected by authors independently on a pre-planned standard data extraction sheet. The collected data was scrutinized involving all authors to detect any discrepancy and a mutual agreement was reached about accuracy. The main variables for data collection included were the list of published authors, the country where the RCT was conducted, year of publication, demographic details of the study population, hernia recurrence numbers, duration of operation, surgical site infections, wound seroma, wound break down, delayed wound healing, cost of the laparoscopic procedure and the cost of the robotic procedure.
Evidence Synthesis Using RevMan Statistical Software
RevMan version 5.4 (Review Manager 5.4, The Nordic Cochrane Centre, Copenhagen, Denmark) was used for the statistical analysis [10] of the data. In order to present the summated outcome of continuous variables such as cost of the procedure and duration of operation; the standardised mean difference (SMD) was used, and the risk ratio was used to present the summated outcomes of dichotomous data (Wound complication and hernia recurrence). The SMD and RR were calculated and presented with a 95% confidence interval (CI) under the random-effects model analysis [11, 12]. A forest plot was used for the graphical presentation of the results. The statistical heterogeneity was calculated by computing the chi2 test, with significance set at P < 0.05 whereas the quantification of the heterogeneity was tested using the I2 test with a maximum value of 30 per cent identifying low heterogeneity [13]. For the calculation of the SMD, the inverse-variance method was used and for the calculation of the risk ratio, the Mantel- Haenszel method was used under the random effect model analysis [14, 15]. If standard deviation was not reported in the published article on RCT, it was estimated either from the range or p-value or 0.5 was added in the cell frequency assuming the same variance in both the groups which might not be true in all the cases. The estimate of the difference between both techniques was pooled, depending upon the effect weights in results determined by each trial estimate variance.
Quality of Analysis
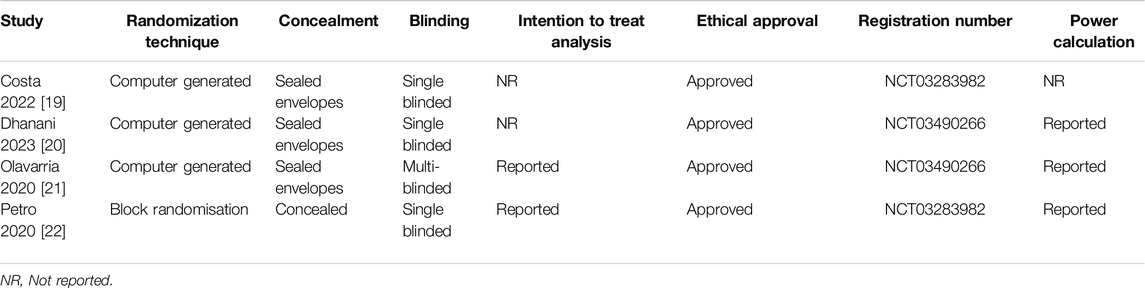
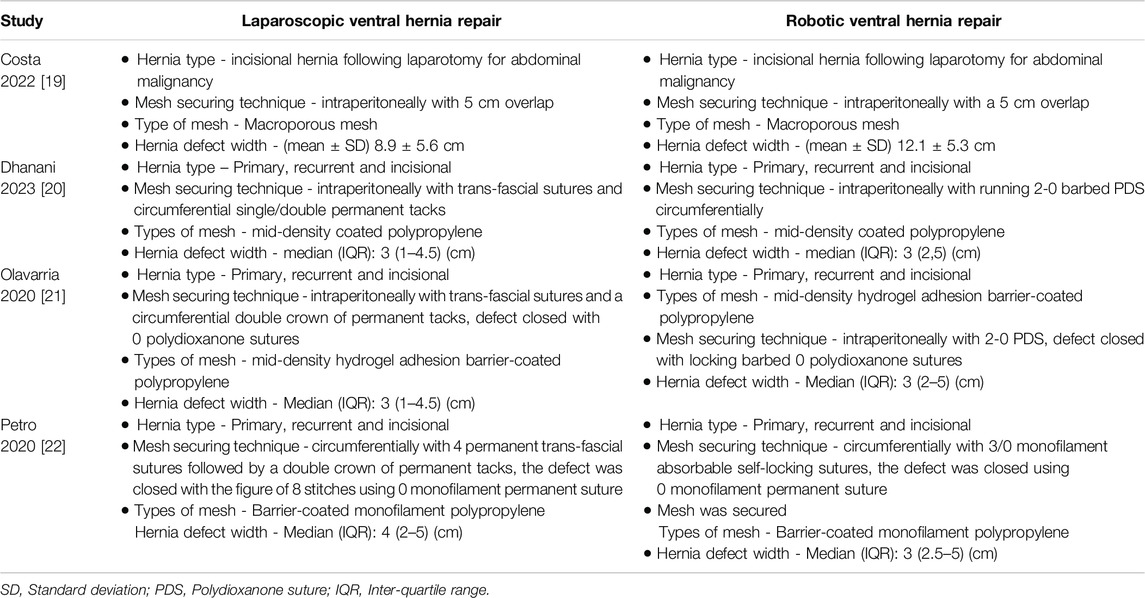
The quality of the included RCTs was assessed by using various reported tools including the tool provided by the Cochrane Collaboration [16–18]. The quality of included studies is given in Table 1 and depicted in Figures 1, 2.
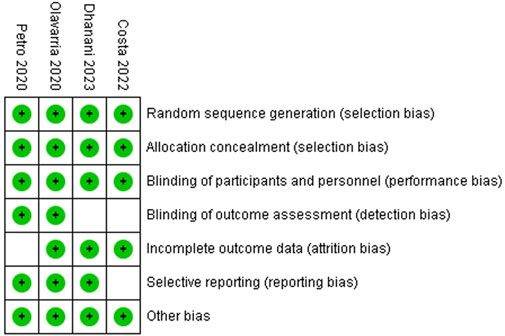
Figure 1. Risk of bias summary: review authors’ judgements about each risk of bias item in included trials.
Selected Endpoints for Analysis
The recurrence of VH at the end of the follow-up period was considered the primary endpoint for this systematic review. The criteria to diagnose the VH recurrence included the symptomatic presentation of the patient with a recurrent lump at the site of previous surgery, clinical assessment by a senior surgeon and the reporting of the radiological diagnostic investigation to confirm it. The secondary endpoints were the surgical site complications, duration of operation, length of hospital stay and the cost of LVHR as well as the cost of RVHR.
Results
The primary search of the standard medical databases yielded 22 potential includable studies in this systematic review. After going through the various stages of screening, 18 trials were excluded due to the reasons given in the PRISMA flowchart (Figure 3).
Methodological Quality of Included Studies
The reported quality variables in the included RCTs used to assess their strength of published evidence is summarized in Table 1. The randomization technique used in the included RCTs was computer generated in all RCTs [19–22]; the concealment was done using sealed envelopes in three included RCTs [19–21]; single blinding was reported in three RCTs [19, 20, 22] and multi-blinding [21] was reported in one included RCT. All included studies reported ethical approval and were registered before the conduction of the trial. Power calculation was done and reported in three studies [20–22].
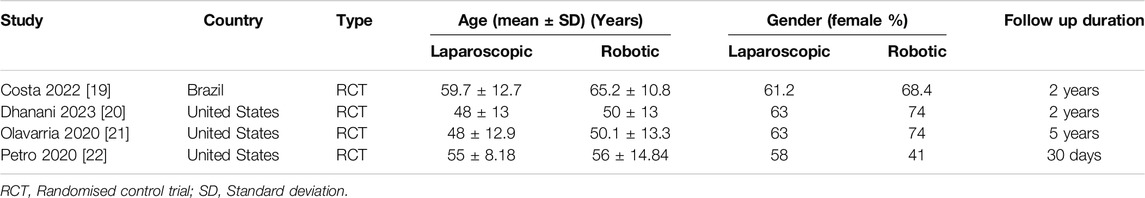
Characteristics and Demographics of Included Studies
Four RCTs [19–22] on 337 patients were included to study for perioperative outcomes and cost comparison. A one year-follow up of Petro, et, al; was used to study the recurrence rate as well [23]. One included RCT was reported from Brazil [19] and three reported RCTs were from the USA [20–22]. The characteristics of the included RCTs are presented in Table 2 and the treatment protocols used in the included studies are presented in Table 3.
Primary Outcome Analysis
In the random effects model analysis, the incidence of VH recurrence was statistically similar between groups of laparoscopic versus robotic groups [RR 1.05, 95%, CI (0.22, 4.99), Z = 0.06, P = 0.95; Figure 4]. There was moderate heterogeneity among included RCTs (Tau2 = 1.26; Chi2 = 5.99, df = 2; (p = 0.05; I2 = 67%).
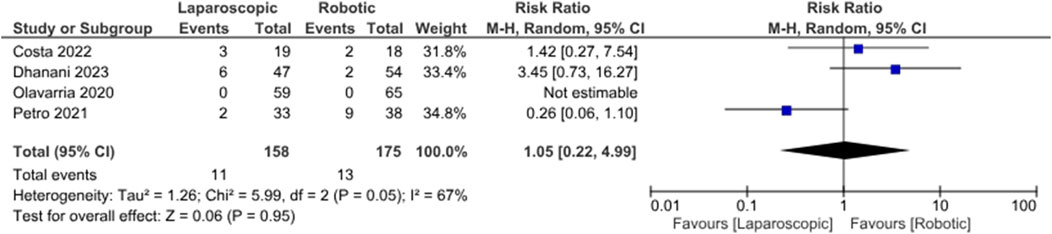
Figure 4. Forest plot showing the risk of recurrence in LVHR versus RVHR group. The outcome is presented as a risk ratio with a 95% confidence interval.
Secondary Outcomes Analysis
In the random effects model analysis, the risk of surgical site complications (surgical site infection, seroma formation, wound break down, slow wound healing, failed wound healing) was statistically similar between LVHR group and RVHR group and there was no heterogeneity [RR, 0.85, 95%, CI (0.48, 1.50), Z = 0.55, p = 0.58; Figure 5], (Tau2 = 0.00; Chi2 = 1.06, df = 3; (p = 0.79; I2 = 0%). The duration of operation was shorter in patient undergoing LVHR compared to RVHR indicating superiority of laparoscopic approach over robotic approach [SMD -48.07, 95%, CI (−78.06, −18.07), z = 3.14, p = 0.002; Figure 6]. However, there was statistically significant heterogeneity among included studies on the calculation of this variable (Tau2 = 680.13; Chi2 = 362.84, df = 2; (p = 0.00001; I2 = 99%). In addition, LVHR was associated with reduced cost compared to RIVR in the random effects model analysis [SMD 0.82, 95%, CI (−1.48, −0.16), z = 2.45, p = 0.01; Figure 7]. However, there was statistically significant heterogeneity among included RCTs (Tau2 = 0.15; Chi2 = 2.87, df = 1; (p = 0.09; I2 = 65%).
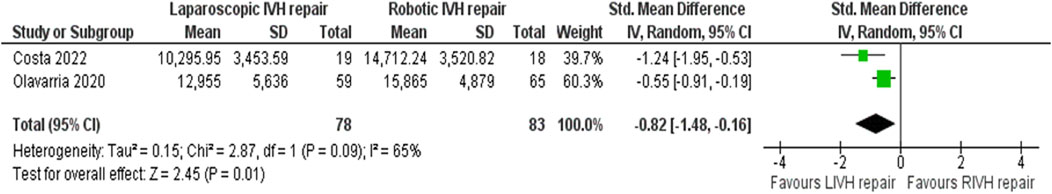
Figure 5. Forest plot showing the risk of surgical site complications in LVHR versus RVHR group. The outcome is presented as a risk ratio with a 95% confidence interval.
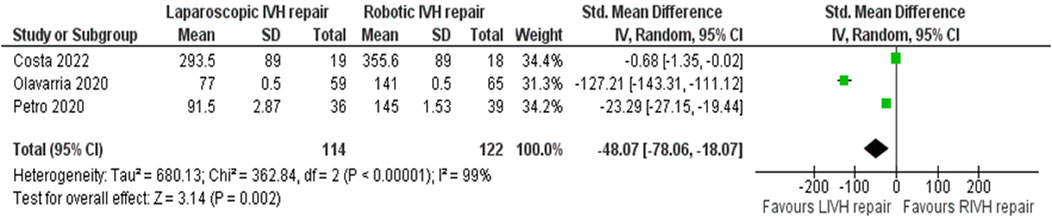
Figure 6. Forest plot showing the duration of operation in LVHR and RVHR cohorts. The outcome is presented as a standardised mean difference with a 95% confidence interval.
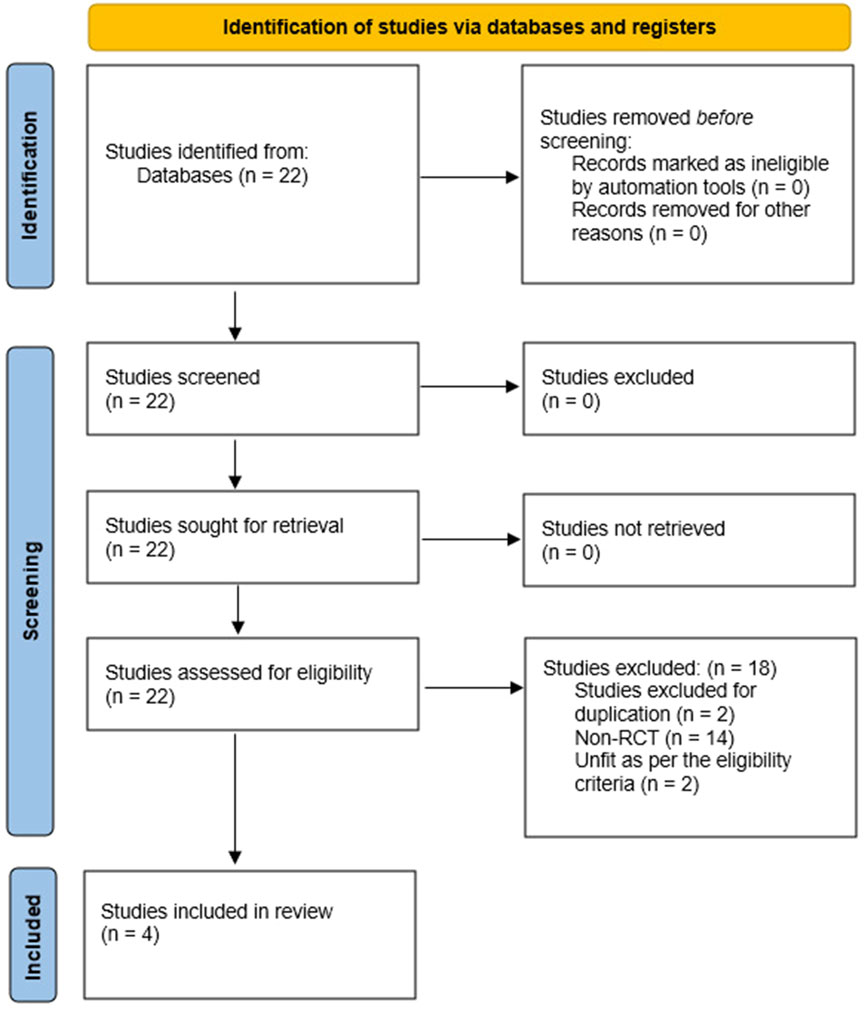
Figure 7. Forest plot showing the operative cost in LVHR and RVHR cohorts. The outcome is presented as a standardised mean difference with a 95% confidence interval.
Discussion
Based upon the findings of this systematic review, LVHR seems to have the advantage over RVHR in terms of shorter duration of operation, lower cost of the procedure and equivalent efficacy for surgical site complications and hernia recurrence. RVHR failed to prove any clinical advantage over LVHR. Although these are very conclusive findings, however, this conclusion should be taken cautiously because of the paucity of RCTs with fewer patients undergoing VH repair.
Comparison With Existing Literature
A previously published systematic review in 2023 [24] compared LVHR against RVHR and reported patient-related outcome measures. It was concluded that the available data on laparoscopic and robotic primary ventral hernia repair was scarce, and it was highly heterogeneous, thus making it difficult to assess the superiority of either approach in the management of VH. The current study provided evidence generated from the summated outcome of four RCTs and concludes that RVHR does not seem to have any proven clinical advantage over LVHR. Another published systematic review in 2020 [25] reported perioperative outcomes in a group of patients undergoing LVHR versus RVHR. The results of this review suggested that RVHR maintained some of the advantages of laparoscopic surgery and might provide an additional advantage of reduced hernia recurrence risk. This may well be explained by the ability to perform a more complex hernia repair with robotic assistance secondary to the ease of closure of the fascial defect. Whereas the current study analysed RCTs only and failed to demonstrate the previously reported advantage of the robotic approach. Several comparative trials have been reported with diverse outcomes [26, 27] and without any conclusive recommendations.
Limitations
There was significant methodological and clinical diversity among included trials indicating heterogeneity. This study is based upon the findings of four RCTs on 337 patients and due to this reason, these findings cannot be generalised. The inclusion criteria were also different and patients with incisional hernia and primary ventral were jointly recruited in both limbs of trials which can potentially contribute to the biased outcome. The size of the hernia defect was reported in all studies, but it was of different size. The duration of follow-up in included RCTs varied from 1 year to 5 years which seems to be insufficient for the accurate estimation of the recurrence rate of hernia. Power calculations and intention to treat analysis were also not reported in the two included RCTs.
Future Implications
A major multicentre RCT is mandatory to validate the findings of the current study before drawing a stronger conclusion about the advantages of the robotic approach in the management of VH. Trials on primacy ventral hernia and incisional hernia should be conducted separately to assess which group of hernia can benefit more from either approach. The patient recruitment criteria should be strict in terms of hernia defect size, type of mesh used, and technique of mesh fixation used to reduce methodological diversity in the RCTs. Trials should be conducted using a gold standard radiological diagnostic tool to detect clinical and subclinical recurrence for accurate measurement of primary outcome.
Author Contributions
(I) Conception and design: AS, MS, and WT; (II) Administrative support: AS, WT, GK, and MB; (III) Provision of study materials or patients: MS, GK, and NE; (IV) Collection and assembly of data: AS, GK, and WT; (V) Data analysis and interpretation: AS, MS, WT, and MB; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The provisional abstract of this systematic review has been presented as a short paper at the annual conference of “Association of Surgeons of Great Britain and Ireland” on 08th–10th May in Belfast, United Kingdom.
References
1. Sheetz, KH, Claflin, J, and Dimick, JB. Trends in the Adoption of Robotic Surgery for Common Surgical Procedures. JAMA Netw Open (2020) 3(1):e1918911. doi:10.1001/jamanetworkopen.2019.18911
2. Pawlak, M, Tulloh, B, and de Beaux, A. Current Trends in Hernia Surgery. NHS Engl The Ann The R Coll Surgeons Engl (2020) 102(1):25–7. doi:10.1308/rcsann.2019.0118
3. Poulose, BK, Shelton, J, Phillips, S, Moore, D, Nealon, W, Penson, D, et al. Epidemiology and Cost of Ventral Hernia Repair: Making the Case for Hernia Research. Hernia (2012) 16(2):179–83. doi:10.1007/s10029-011-0879-9
4. Zayan, NE, Meara, MP, Schwartz, JS, and Narula, VK. A Direct Comparison of Robotic and Laparoscopic Hernia Repair: Patient-Reported Outcomes and Cost Analysis. Hernia (2019) 23(6):1115–21. doi:10.1007/s10029-019-01943-7
5. Corcione, F, Esposito, C, Cuccurullo, D, Settembre, A, Miranda, N, Amato, F, et al. Advantages and Limits of Robot-Assisted Laparoscopic Surgery: Preliminary Experience. Surg Endosc Other Interv Tech (2005) 19(1):117–9. doi:10.1007/s00464-004-9004-9
6. Hockstein, NG, Gourin, CG, Faust, RA, and Terris, DJ. A History of Robots: From Science Fiction to Surgical Robotics. J Robot Surg (2007) 1:113–8. doi:10.1007/s11701-007-0021-2
7. Armijo, P, Pratap, A, Wang, Y, Shostrom, V, and Oleynikov, D. Robotic Ventral Hernia Repair Is Not Superior to Laparoscopic: A National Database Review. Surg Endosc (2018) 32(4):1834–9. doi:10.1007/s00464-017-5872-7
8. Chen, YJ, Huynh, D, Nguyen, S, Chin, E, Divino, C, and Zhang, L. Outcomes of Robot-Assisted Versus Laparoscopic Repair of Small-Sized Ventral Hernias. Surg Endosc (2017) 31(3):1275–9. doi:10.1007/s00464-016-5106-4
9. Coakley, KM, Sims, SM, Prasad, T, Lincourt, AE, Augenstein, VA, Sing, RF, et al. A Nationwide Evaluation of Robotic Ventral Hernia Surgery. Am J Surg (2017) 214(6):1158–63. doi:10.1016/j.amjsurg.2017.08.022
10. Review Manager (RevMan) [Computer program]. The Nordic Cochrane Centre. Copenhagen: The Cochrane Collaboration (2008). Available from: http://tech.cochrane.org/revman/download/windows64 (Accessed October 03, 2018).
11. DerSimonian, R, and Laird, N. Meta-analysis in Clinical Trials. Control Clin Trials (1986) 7:177–88. doi:10.1016/0197-2456(86)90046-2
12. Demets, DL. Methods for Combining Randomized Clinical Trials: Strengths and Limitations. Stat Med (1987) 6:341–50. doi:10.1002/sim.4780060325
13. Higgins, JP, and Thompson, SG. Quantifying Heterogeneity in a Meta-Analysis. Stat Med (2002) 21:1539–58. doi:10.1002/sim.1186
14. E Matthias, SG Davey, and DG Altman, editors. Systematic Reviews in Health Care: Meta-Analysis in Context. 2nd ed. London: BMJ Publishing Group (2001). p. 487.
15. Deeks, JJ, Altman, DG, and Bradburn, MJ. Statistical Methods for Examining Heterogeneity and Combining Results from Several Studies in Meta-Analysis. In: M Egger, GD Smith, and DG Altman, editors. Systematic Reviews in Health Care: Meta-Analysis in Context. 2nd ed. Londong: John Wiley and Sons, Ltd (2001). p. 285–312.
16. Jadad, AR, Moore, RA, Carroll, D, Jenkinson, C, Reynolds, DJ, Gavaghan, DJ, et al. Assessing the Quality of Reports of Randomized Clinical Trials: Is Blinding Necessary? Control Clin Trials (1996) 17:1–12. doi:10.1016/0197-2456(95)00134-4
17. Chalmers, TC, Smith, H, Blackburn, B, Silverman, B, Schroeder, B, Reitman, D, et al. A Method for Assessing the Quality of a Randomized Control Trial. Control Clin Trials (1981) 2:31–49. doi:10.1016/0197-2456(81)90056-8
18. Dudgeon, D, and Rangel, S. Development of a Quality Assessment Scale for Retrospective Clinical Studies in Paediatric Surgery. J Pediatr Surg (2003) 38:396. doi:10.1053/jpsu.2003.50114
19. Costa, TN, Abdalla, RZ, Tustumi, F, Junior, UR, and Cecconello, I. Robotic-Assisted Compared With Laparoscopic Incisional Hernia Repair Following Oncologic Surgery: Short- and Long-Term Outcomes of a Randomized Controlled Trial. J Robot Surg (2023) 17(1):99–107. doi:10.1007/s11701-022-01403-y
20. Dhanani, NH, Lyons, NB, Olavarria, OA, Bernardi, K, Holihan, JL, Shah, SK, et al. Robotic versus Laparoscopic Ventral Hernia Repair: Two-Year Results From a Prospective, Multicenter, Blinded Randomized Clinical Trial. Ann Surg (2023) 278(2):161–5. doi:10.1097/SLA.0000000000005903
21. Olavarria, OA, Bernardi, K, Shah, SK, Wilson, TD, Wei, S, Pedroza, C, et al. Robotic versus Laparoscopic Ventral Hernia Repair: Multicenter, Blinded Randomized Controlled Trial. BMJ (2020) 370:m2457. doi:10.1136/bmj.m2457
22. Petro, CC, Zolin, S, Krpata, D, Alkhatib, H, Tu, C, Rosen, MJ, et al. Patient-Reported Outcomes of Robotic vs Laparoscopic Ventral Hernia Repair with Intraperitoneal Mesh: The PROVE-IT Randomized Clinical Trial. JAMA Surg (2021) 156(1):22–9. doi:10.1001/jamasurg.2020.4569
23. Petro, CC, Thomas, JD, Tu, C, Krpata, DM, Beffa, LR, Rosen, MJ, et al. Robotic vs Laparoscopic Ventral Hernia Repair With Intraperitoneal Mesh: 1-Year Exploratory Outcomes of the PROVE-IT Randomized Clinical Trial. J Am Coll Surg (2022) 234(6):1160–5. doi:10.1097/XCS.0000000000000171
24. Dixit, R, Prajapati, OP, Krishna, A, Rai, SK, Prasad, M, and Bansal, VK. Patient-reported Outcomes of Laparoscopic Versus Robotic Primary Ventral and Incisional Hernia Repair: A Systematic Review and Meta-Analysis. Hernia (2023) 27(2):245–57. doi:10.1007/s10029-022-02733-4
25. Goettman, MA, Riccardi, ML, Vang, L, Dughayli, MS, and Faraj, CH. Robotic Assistance in Ventral Hernia Repair May Decrease the Incidence of Hernia Recurrence. J Minim Access Surg (2020) 16(4):335–40. doi:10.4103/jmas.JMAS_92_19
26. Prabhu, AS, Dickens, EO, Copper, CM, Mann, JW, Yunis, JP, Phillips, S, et al. Laparoscopic vs Robotic Intraperitoneal Mesh Repair for Incisional Hernia: An Americas Hernia Society Quality Collaborative Analysis. J Am Coll Surg (2017) 225(2):285–93. doi:10.1016/j.jamcollsurg.2017.04.011
Keywords: laparoscopic ventral hernia repair, robotic ventral hernia repair, perioperative outcomes, cost comparison, IPOM
Citation: Singh A, Toh WH, Elzahed N, Khera G, Baig MK, Mihailescu A and Sajid MS (2025) Laparoscopic Versus Robotic Ventral Hernia Repair With Intraperitoneal Mesh: A Systematic Review and Meta-Analysis Comparing the Perioperative Outcomes Randomised Controlled Trials. J. Abdom. Wall Surg. 3:13809. doi: 10.3389/jaws.2024.13809
Received: 15 September 2024; Accepted: 17 December 2024;
Published: 22 January 2025.
Copyright © 2025 Singh, Toh, Elzahed, Khera, Baig, Mihailescu and Sajid. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anurag Singh, YW51cmFnc2luZ2gzMTM5QGdtYWlsLmNvbQ==
 Anurag Singh
Anurag Singh Wei H. Toh2
Wei H. Toh2 Andrei Mihailescu
Andrei Mihailescu