Abstract
The history of pre peritoneal groin hernia surgery start only after solving the problems related to asepsis, antisepsis and anesthesia. Fundamental work on the use of a new form of polyethylene to create synthetic meshes was carried out in the 1950s by C. Usher. L. Nyhus was the first to popularize the use of a mesh. But the inventor of the first synthetic prosthesis was Don Eugène Acquaviva in 1944, and the first surgeon to discuss the installation of a pre-peritoneal prosthesis for the treatment of hernias of the groin is Jerome Corti in his thesis in 1949. In the 50 s and 60 s H. Fruchaud had particularly and directly influenced Jean Rives and René Stoppa, and due to the poor results of techniques without prosthesis, particularly for complex hernias Rives and Stoppa techniques were then disseminated with lots of variations, (G. Wantz, J.H. Alexandre, R. D. Kugel….) But the parietalization step was difficult to achieve for many colleagues and the development of endoscopy has made it possible to clearly demonstrate this crucial step in order to properly unroll the prosthesis. Franz Ugahary put up resistance against endoscopy with the Grid Iron technique in 1995, the fist open minimal invasive pre peritoneal approach. In 2004, Pelissier invented a specific semi-rigid prosthesis, which made it possible to codify with colleagues the Trans Inguinal Pre-Peritoneal (TIPP) technique. But it was also necessary to master the step of parietalization of the cord, this is probably why the ONSTEP technique was created in 2005. It is a partially preperitoneal technique without parietalization W. Akkersdick has tackled the challenge with the Trans Rectus sheath Pre Peritoneal (TREPP) technique in 2006, a pure posterior approach. For my part I modified the TIPP technique in 2011 using Ugahary’s dissection principles, the Minimal Open Pre Peritoneal (MOPP) technique was created. It is only in recent years that the literature has provided data about TIPP, TREPP, MOPP, with comparisons with others techniques. Now the new route, preperitoneal, minimal open and minimal invasive has its place in the treatment of groin hernias!
Introduction
Since antiquity, the history of inguinal hernia surgery is rich in anecdotes with most often fatal conclusions for patients [1], and this continues even during the second half of the 19th century where the subject of this article, dedicated to the preperitoneal approach to treat inguinal hernias, begins. The 19th century brings knowledge in terms of anatomy and in terms of hygiene to allow the surgeon to penetrate the preperitoneal space, the 20th century brings the synthetic prostheses to gain in efficiency, and finally the end of the 20th century and the beginning of the 21st century are decisive to define resolutely minimally invasive techniques on the basis of classical procedures. This new way then expresses itself fully by giving the first scientific guarantees that we are entitled to expect. The main objective of this article, besides recalling historical facts by sometimes correcting certain injustices concerning underestimated and sometimes even forgotten authors, is to put into perspective the links which exist between surgeons of several generations who had the same ambition, to perform a surgery that was a priori complex in the least invasive way possible and which was aimed at the greatest number of patients.
Development
The anatomical data were clarified and shared by A.P. Cooper in 1807 [2], A. Bogros in 1823 [3], A Thomson in 1836 [4], A.A. Retzius, 1858 [5], completed by E. Bassini in 1887 [6], and later by E.E. Shouldice in 1945 [7], H. Fruchaud in 1956–1957 [8, 9] (Figure 1), C.B. McVay in 1958 [10] and R.E. Condon in 1971 [11]. Even though knowledge of anatomy might have allowed it, therapeutic means were very ineffective before the use of asepsis, antisepsis and anesthesia. Thus, during the first part of the 19th century, the pioneers were mainly interested in these patients in very poor condition with an irreducible hernia whose outcome was in any case spontaneously fatal. They also used the posterior approach, but most often patients died of gangrene [1]. Most other patients who were not directly at risk for complications were not operated on.
FIGURE 1
Henri Fruchaud (1894–1960).
During the same decades, the British surgeon Joseph Lister described in 1867 the success of a method to combat postoperative infections: antisepsis [12]. This idea came to him from the demonstration made by Louis Pasteur a few years before, which highlighted the role of microbes in the origin of infections. Asepsis came to complement Lister’s antisepsis, which had only been accepted very gradually. Ultimately, the two processes allowed a real development of surgery from 1885, and particularly allowed the opening of parietal spaces with a drastically reduced rate of fatal post-operative infection [1].
It is precisely around these same decades that research concerning local and general anesthesia would be published and spread [13]. From nitrous oxide to chloroform in the 1840s for general anesthesia, cocaine for local anesthesia, Freud 1884, P. Reclus (7,000 cases) Paris, and the invention of the spinal anesthesia in August 1898 by August Bier. All the pillars (anatomy, anesthesia, antisepsis, asepsis) were in place and would be immediately used for hernia surgery from the second part of the 18th and beginning of the 19th century.
The pioneers for the posterior approach are, according to Chavasse, Crompton of Birmingham [14], followed by Niven [15] and Annandale who repeated the Crompton’s procedure in 1876 [16]. He was followed by Lawson Tait [17] from Birmingham, then by Bates [18] and G.L. Cheatle 1920 from the England- King’s college hospital London, who was a devoted disciple of Lister [19]. Patino clarifies: “Cheatle, in 1920, described an operation for the radical cure of inguinal and femoral hernias through a medial abdominal section, without entering the peritoneal cavity” [20, 21], and in 1921 Cheatle reported on the use of the Pfannenstiel incision. In 1936 Henry [22] emphasized the advantages of Cheatle’s approach in the cure of bilateral femoral hernias with a little impact before World War II. At this period, we spoke about the Cheatle-Henry procedure that provides excellent exposure of anatomic structures adjacent to the femoral canal. And it is finally Henry who popularized the posterior approach among the pioneers of the second half of the 20th century, with Mc Evedy [23], but always without the help of a prosthesis. The gold standard at that time was the anterior approach, following the works of Bassini [6] and Shouldice [7]. For femoral hernias, McVay described his eponymous technique in 1938 [10], but surgeons did not accept his original description. They omitted making the relaxation incision and results were not as good as those published by McVay. So, everything was in place for the next decisive step which was the birth of synthetic prostheses.
The inventor of the first synthetic prosthesis was Don Eugène Acquaviva from Marseille. He personally had manufactured, patented and used a nylon mesh for an incisional hernia in 1944 [24, 25] (Figure 2), and the first surgeon to discuss the installation of a pre-peritoneal prosthesis for the treatment of a groin hernia, which was a femoral hernia (but without realizing it himself), was his son-in-law Dr Jérôme Corti in his thesis in 1949 [26] (Figure 3). Don Eugène Acquaviva was particularly innovative in terms of the design of synthetic mesh and its use in ventral surgery. His work was published thanks to the interest shown by Lucien Leger from Hospital Cochin in Paris, who was the editor of the “notes of surgical techniques” in the “Presse Medicale” journal. These notes were widely distributed and were serious references at the French as well as at the international level. The nylon prosthesis patented by Acquaviva would soon be used by Bourgeon and would also be inserted into the preperitoneal space [27, 28].
FIGURE 2
Don Eugène Acquaviva (1897–1976).
FIGURE 3

Dominique Corti (1919–1983).
However, the fundamental work was carried out by C. Usher (Figure 4) in his private practice in Houston, Texas [29]. He used a new ethylene polymer woven into a mesh, the Marlex prosthesis, which was fabricated to his design, and used for groin hernia surgery in 1958. A knitted Marlex product was introduced in 1961. The same year a braided Marlex suture appeared [30]. Polypropylene monofilament, an isotactic polymer which retains its tensile strength, was introduced in 1962, recommended as an inert suture to close contaminated wounds [31, 32]. Monofilament polypropylene suture is still the preferred synthetic material today! Usher therefore carried out numerous experimental and clinical studies resulting in 20 papers on hernia between 1958 and 1967 [30–38]. As Read said [29], “Usher realized Billroth’s vision,” (1878) as quoted by Vincenz Czerny in his textbook, “If we could artificially produce tissues of the density and toughness of fascia and tendon, the secret of the radical cure of hernia would be discovered.”
FIGURE 4
Francis C. Usher (1908–1980).
But the acceptance of prosthetic materials in parietal surgery was very low. As Read reminds us [39] Usher said, “surgeons are usually reluctant to use a prosthesis for fear of wound complications and a natural disinclination to use foreign materials.” Note that before Usher, and thanks to his own experimental work [31], early polymers such as Nylon (Acquaviva), Dacron, Orlon and Teflon had been the most studied, but the results were disappointing. Foreign body reaction, sepsis, stiffness, fragmentation, loss of tensile strength, and encapsulation have prevented their widespread use. Metal prostheses (Tantalum Gauze) had also given disappointing results, as Debord recalls [40], even though stainless-steel mesh had enthusiastic users until the 80s [41]. This hostility against protheses would last a long time and this was confirmed to me by Jean Rives (Figure 5). He told me during a 2-h recorded interview on 6 October 2011, that he had been heavily criticized in the 1960s and 1970s, because of his practice of using prosthetic material for simple non-recurrent hernias, even by his colleagues who were also his friends [42].
FIGURE 5
Jean Rives (1922–2012).
Moreover, even though Usher widely used prostheses in the preperitoneal space with parietalization of the cord, the official laurels would preferentially go to Nyhus (Figure 6) and too few colleagues who popularized the use of a mesh allowed the Cheatle-Henry and Mc Evedy incision [19–21]. In their 1959 paper, Nyhus and colleagues described the use of a synthetic sponge (Ivalon®) to reinforce the posterior wall of a recurrent hernia [43, 44]. Due to its poor tolerance, the Ivalon sponge would quickly be abandoned in favor of the Marlex mesh created by Usher. At that time, many surgeons applied the principles published by Nyhus: Sheehan (1961), Mahorn and Goss (196, Smith (1962), Huguier (1963), Estrin (1963), Andrews (1968) and Read (1968).
FIGURE 6

Llyod Milton Nyhus (1923–2008).
In 1956, only a few years before Usher Nyhus and Henry, Fruchaud [9] had insisted on the need for broad coverage of the musculo-pectineal orifice which bears his name. Henry Fruchaud had particularly influenced Jean Rives and René Stoppa (Figure 7) who had worked in the anatomy laboratory of the Faculty of Medicine of Algiers. During this period Fruchaud worked on his two famous books [8, 9], never translated before Robert Bendavid in 2006 [45] and therefore largely unknown in the Anglo-Saxon world despite the efforts of R. Stoppa to promote them. So, in the 70s, directly influenced by their mentor, J. Rives [46, 47], and then R. Stoppa [48–50] described their techniques in a general context still unfavorable to the use of parietal prostheses, except gradually for complex groin hernias. The polyester Dacron mesh (mersilene) was first used in France by J. Rives following the presentation of the mesh by the laboratory that marketed it [41]. R. Stoppa was inspired by the Rives’ technique for bilateral hernias by creating his eponymous technique. Eventually, and probably partly due to the popularity of Lichtenstein’s technique, the gold standard in the 1980s, the idea of using a prosthesis had finally become commonly accepted. Even surgeons who were still against the use of prostheses admitted the advantages for the most complex cases, and the techniques of Rives and Stoppa were then disseminated with lots of variations, such as G. Wantz [51], (Figure 8), and J.H. Alexandre [52, 53], (Figure 9) techniques.
FIGURE 7
René Stoppa (1921–2006).
FIGURE 8

George Wantz (1923–2000).
FIGURE 9

Jean Henry Alexandre (1931–2019).
Jean Henri Alexandre’s technique is a step to remember towards less invasive solutions. It could be considered as a precursor of the TIPP technique. The approach was a classic anterior approach as it provided for the ligation of the inferior epigastric vessels to facilitate access to the preperitoneal plane, the prosthesis being fixed. But at the time these techniques required regional or general anesthesia and classic hospitalization.
Another variation is the R.D. Kugel technique [54]. The initial Kugel mesh had an abundant amount of foreign material present. Problems with the initial recoil ring resulted in pain and even bowel perforation. Another version of this mesh type contained a resorbable memory ring. The Kugel technique has often been compared to the TIPP technique [55]. This is where Franz Ugahary [56, 57] (Figure 10) and Edouard Pelissier [58] (Figure 11) come in and are seen as the two true pioneers of minimally invasive preperitoneal surgery: During the early 1990s they were thinking about how to place a prosthesis in the preperitoneal space in a decidedly less invasive way than the Stoppa and Rives techniques, used for complex cases by these authors and without wanting to embark on endoscopic surgery, which they found more invasive. In this period the TAPP was the most used endoscopic technique. Pelissier was convinced and familiar with techniques using the anterior route (modified Bassini, Shouldice) under local anesthesia, with the desire to promote outpatient care [59, 60]. He used the Stoppa Rives procedure for the more complex cases. In May 1990 he had the idea of using a pre-peritoneal prosthesis after hearing Gilbert [61] presenting his plug [62] at a conference in Nice during the first French international hernia surgery symposium. The plug was a 5 cm square of polypropylene opened from the middle of one side to the center and inserted through the deep inguinal opening, with the cord passing through the slit. However, the technique was not easy to achieve and there were not many indications. The second influence came from Rutkow and Robbins [63] who had designed the plug, which was introduced through the hernial orifice, but the prosthesis was not spread flat. Although the results seemed very good in terms of recurrence, it came at the cost of a rate of chronic pain (8.6%) due to the shrinkage of the prosthesis, which ended up forming a sort of hard core [64]. These two relative failures confirmed our pioneer in his first idea; to invent a prosthesis that spreads flat in the pre-peritoneal space, introduced through the hernia orifice, self-deploying, and by performing an intervention preferably under local anesthesia. Local anesthesia was associated with an outpatient procedure at this period, and already widely practiced in many countries, but unfortunately not in several others where it was almost impossible for reasons of organization of the health system, including France. But the idea of outpatient surgery was still on the minds of many. Pelissier began to work extensively from 1999 with the development of different prototypes which finally led in September 2004 to the launch of the first prosthesis specifically dedicated to being spread forward in the pre-peritoneal space: the Polysoft prosthesis. The prosthesis would first be split to allow passage for the cord [58], using the principle of the split prosthesis as in the Gilbert and Liechtenstein procedures, which was easier. Very quickly interested in Pelissier’s principle, Frederik Berrevoet (Figure 12) and Stephen de Gendt had invited E. Pelissier to the University Hospital of Ghent for a workshop. Frederik Berrevoet was not satisfied with Lichtenstein’s technique which was mainly used in Belgium at that time and not convinced by the intraperitoneal route of the TAPP endoscopic technique which was spreading more quickly than the TEP technique. They immediately used the technique with the specific prosthesis but without splitting he prosthesis and therefore parietalizing the cord [65, 66]. And Pelissier would quickly make the parietalization, because of two recurrences through the split in the prosthesis [61]. It is very interesting to point out that the technique was thus finalized by E. Pelissier, F. Berrevoet, S. De Gendt and colleagues in Belgium and quickly disseminated in France by J.F. Gillion and J.M. Chollet [67, 68] (Figure 13) and finally called Trans Inguinal Pre-Peritoneal (TIPP). It still appeared difficult to achieve for certain colleagues who returned to the Lichtenstein technique, after having learned the technique from the first promoters who organized workshops in their respective operating rooms, as observed by E. Pelissier [61]. And for the same reason two authors rom Porto, A. Lourenco and R. S. da Costa, developed the Onstep technique in 2005, pursuing the idea of splitting the prosthesis and simplifying the learning of the technique by avoiding the parietalization step [69]. Onstep technique is a partially preperitoneal technique as the lower and medial part of the prosthesis are in the preperitoneal space and the upper and lateral part are positioned as in the Lichtenstein technique, under the aponeurosis of the external oblique muscle.
FIGURE 10

Franz Ugahary.
FIGURE 11

Edouard Pelissier.
FIGURE 12

Frederik Berrevoet.
FIGURE 13

Jean François Gillion and Jean Michel Chollet.
We can thus realize that in this adventure one of the points of friction remains the notion of parietalization ! Let’s look at this:
Due to the not the experience of surgeons, this step of parietalization has slowed down the dissemination of the posterior route. This is why René Stoppa in 1973 published the drawing of his intervention “the Giant Preperitoneal Repair” (GPPR), one side with parietalization and the other side with a slit in the prosthesis even though in his practice he never split the prosthesis (Figure 14). If Acquaviva [24, 25] and Bourgeon [27, 28] were pionners to develop the principle of spreading a prosthesis in the preperitoneal space, it was Usher, who was the first in 1959 to publish the principle of parietalization of the cord as Read recalls [29]. Read said: “Another valuable concept he (Usher) documented was the use of unsplit groin prostheses with overlap and interrupted suturing lateral to the internal inguinal ring to allow extended preperitoneal obliquity of the spermatic cord. In his own (Usher) words: “Rather than cut a notch in the mesh, we prefer to suture the lateral border of the mesh well lateral to the curving border of the internal oblique muscle, providing a 'shelf’ for the cord to rest on, and preserving the normal obliquity of the internal ring.” Here is yet another reason to highlight Usher, this formidable precursor who epitomizes the best of 20th Century Herniology” [29]. In 1992, Jean Henri Alexandre was the first to propose the parietalization of the cord by an anterior inguinal incision, making his technique an early version of TIPP [52, 53]. Everything accelerated with the arrival of endoscopic surgery during the early 90s, with very gradually an acceptance of the posterior approach using the principles of Stoppa (Totally Extra Peritoneal technique, (TEP)) and facilitating the understanding and realization of the necessary parietalization, thanks to the magic of video images.
FIGURE 14
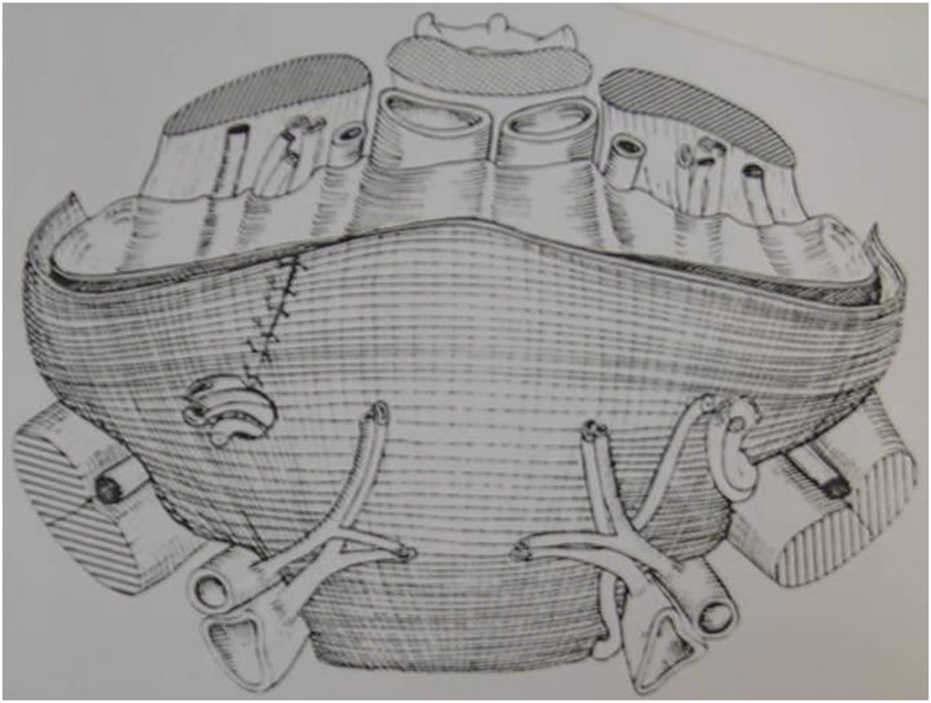
Stoppa: The great prosthesis for the reinforcement of the visceral sac (GPRVS).
After this brief digression we can address the contribution of Franz Ugahary. At this period, it was interesting to note that exactly like Pelissier, Ugahary used Bassini and Lichtenstein as basic techniques, and Stoppa-Wantz for complex cases. In Ugahary’s mind the idea was to precisely reproduce the unilateral Stoppa (Wantz technique) by minimally invasive and purely posterior route. Thus, the Grid Iron type technique was born in 1995, influenced by the seamstress talents of the author’s grandmother, perfectly explaining Ugahary’s specific way of unrolling a classic or even lightweight mesh through a small incision [57]. With his technique, Ugahary is the true founder of the minimally invasive and minimal open totally preperitoneal and totally posterior technique. Ugahary’s strength was to propose new surgical principles, small “grid-iron” incision and specific dissection technique with special valves, to succeed in reproducing Wantz’s technique, with the possibility of using any regular or lightweight flat mesh and above all, allowing a technique that can be carried out under local anesthesia on an outpatient basis. For Pelissier, it was the invention of the prosthesis which allowed the realization of the TIPP technique, while Ugahary created a new operating technique that could use the then available basic meshes. Initially also being a vascular surgeon and having extensive experience in the extraperitoneal approach to large vessels [70], Ugahary took his perfect knowledge of anatomy, and he was very close to René Stoppa and Georges Wantz particularly. Finally, it was Ugahary who succeeded Wantz’s project, which was to perform a unilateral Stoppa in outpatient settings. His technique was immediately adopted by Georges Wantz, a very renowned hernia surgeon in New York, in the same way as his personal technique, especially after a demonstration carried out by F. Ugahary at the medical Hospital-Cornell Medical Center New York [70].
In 1997 René Stoppa, a close friend of Wantz and who directly inspired his technique, had visited Franz Ugahary in Tiel, Netherlands, who then immediately praised his technique as we can read in this letter addressed to F. Ugahary on 31 October 1997 [71]. “… I appreciated the principles of your operation: a posterior approach of Fruchaud myopectineal hole, a large piece of prosthetic mesh, your trend toward minimization of the wall surgical aggression (mini and grid-iron incision) … For me, your technical proposition seems to take place between Nyhus’ or Wantz’ operations through supra-inguinal incisions on one hand, and ours on the other hand … For transmitting, publishing, and teaching your technique, I suggest that you accurately describe every step and guide-marks. Mentioning pitfalls and errors are also a well-advised pedagogical precaution. Don’t forget that you are a gifted skilled surgeon, compared to many colleagues … ” The last sentence was loaded with meaning: is the technique easily reproducible? Stoppa asked me the same question directly while I was presenting the technique to the French academy of surgery in 2004 [72].
The first step of the original technique is the 3 cm incision above the deep inguinal ring as a McBurney incision without the incision of the peritoneum (Grid iron); the huge dissection in the preperitoneal space, typical for the Ugahary technique with different sizes of atraumatic retractors; the reduction of a medial sac, if any; the parietalization of the cord with a dissection of a lateral sac, if any; the checking of the femoral and obturator areas; the use of a 15 by 10 cm regular flat mesh or a lightweight mesh unrolled in the dissected space. No mesh fixation needed. No suture on the musculo fascial plane (transversalis fascia) [57].
In 2000, I was informed of the existence of the Kugel technique [73, 74] which was not yet available in Europe. At that time, I used to operate groin hernias usually with the endoscopic TAPP technique. I asked Stoppa for his opinion on the Kugel technique, He informed me that he knew the technique and had spoken twice with Kugel and without further comment he quickly advised me to visit F. Ugahary … After two short stays in Tiel (Netherlands), and the time necessary to assemble specially manufactured (and patented) instrumentation, I was able to carry out the technique in 2001. It quickly and definitively replaced my TAPP endoscopic technique. I preferentially used the original Ugahary technique between 2001 and 2011 for more than 1,000 hernia repairs with good results. A prospective study on the first 300 operated hernias has been published [72] by the French National Academy of Surgery in 2004. It showed the good results of the technique in terms of recurrence and chronic pain.
The unrolling of the flat mesh through the small incision according to the initial Ugahary technique appeared difficult to reproduce for many colleagues. To successfully carry out the intervention through a 3 – 4 cm incision, it was also necessary to have experience in the dissection of the pre-peritoneal spaces, to be familiar with the parietalization of the spermatic cord, to know how to handle the flexible parietal prostheses (flat polyester or polypropylene mesh, lightweight meshes … ) available at this period and to have the appropriate instrumentation (specific valves). For all these reasons, most surgeons still preferred the Lichtenstein technique, with less frequently endoscopic techniques, and while a few surgeons successfully used Ugahary’s principles, there were not many. I remained very motivated because I thought i had a very promising technique: on the one hand the good principles of a pure posterior preperitoneal approach: on the other hand, its resolutely minimally invasive nature, and finally with these very promising results in some hands. And even after having organized workshops in Cagnes sur Mer and after having presented the technique and its results in all directions (Congresses, French Academy of Surgery, publications) [72, 75, 76], it still appeared difficult to understand for many colleagues and therefore difficult to reproduce.
But as we detailed above, with the same state of mind (except that it is not a pure posterior route), we were joined by the TIPP technique. Following the ingenuity of Edouard Pelissier, it was easier to manipulate the prosthesis specifically created to be placed from the front in the preperitoneal space, which was very difficult to do with prostheses used endoscopically or with other prostheses available at this period.
So, I had the idea (Figure 15) of combining some principles of Ugahary with others of TIPP. I visited Frederik Berrevoet, and Steven De Gendt in Ghent University Hospital in Oct 2007, and Jean François Gillion and Jean Michel Chollet in Antony Private Hospital near Paris to see the TIPP technique in some of the best hands. I carried out this project in 2011. The MOPP technique follows most of the steps of the TIPP technique: from the incision (which is somewhat reduced), the passage at the level of the inguinal canal through the deep inguinal ring, to the spreading of a large prosthesis in the preperitoneal space, with the specific method of Ugahary: dissecting the planes using different sizes of dissectors and retractors. This particularly atraumatic technique eliminates the need for any haemostasis procedures in the deep planes.
FIGURE 15
Marc Soler.
The innovation hinges on the identification of the transversalis fascia (TF) during two pivotal steps: The TF covers the deep inguinal orifice. Recognizing it at this juncture initiates the entry into the preperitoneal space, paving the way for preperitoneal dissection. The TF also constitutes the internal spermatic fascia. Identifying and severing it systematically commences the parietalization of the cord elements. Rationalizing these two essential steps for placing a large prosthesis in the preperitoneal space makes the technique more easily reproducible and teachable. The publication with the help of the specific French database (only used by parietal specialists) have shown very good results on the technique in the hands of the author [77, 78]. More long-term results and a very precise presentation of all the stages of the technique were published in 2024 [79]. The results concerning 1,401 patients show a very low recurrence rate and chronic pain.
Willem Akkersdijk has also tackled the challenge in 2006 with the Trans Rectus sheath Pre-Peritoneal (TREPP) technique [80], a sutureless technique in the same spirit as the Ugahary technique but using the TIPP (Pelissier) prosthesis! TREPP added a significant advantage to the open and minimally invasive preperitoneal approach. It is a perfectly codified [81], with 9 steps, pure posterior approach therefore leaving the anterior planes completely untouched unlike the TIPP and MOPP techniques which are techniques that open the inguinal canal. The TREPP technique is perfectly suitable for nearly all kind of groin hernias, including some of recurrent ones [82–84]. As W. Akkersdijk said [85], “TREPP was developed in the era of endoscopic surgery. The preperitoneal space had gained popularity and the upstream principle was advocated as a logical way to keep the mesh in the right position, even without fixing it and to minimize the chance of recurrences. TREPP has not always been called the same. In the beginning it was called the rectus sheath approach. The absence of a posterior rectus fascia was one of the reasons this route was chosen to reach the preperitoneal spaces just beneath the lateral edges of the rectus muscle. Compared to other open preperitoneal techniques, Ugahary, Pelissier, Rives-Stoppa, with the TREPP technique, the dissection was minimized and the view on the internal ring was optimized by the point of entrance of the preperitoneal space.” W. Akkersdijk insists on the fact that “muscle tension may also cause problems in the creation of the preperitoneal space. Optimal muscle relaxation can be reached by spinal anesthesia or like in endoscopic groin surgery, general anesthesia.”
It seemed obvious to all the pioneers of the new open approach that this minimal open route was much less invasive than endoscopic techniques known as minimally invasive techniques (MIS)! But these were only expert opinions without published studies with a high level of evidence…
It is only in recent years that the literature has provided data about TIPP and TREPP, with comparisons to other techniques and has shown good results of this third way of operating on inguinal hernias. However, drawing parallels to other preperitoneal techniques suggests that MOPP’s outcomes might align with other open or endoscopic methods such as TREPP, TEP and TAPP. Hurel and colleagues [86] support this assumption in their conclusion from a recent propensity score matching analysis comparing 1-year postoperative chronic pain using Lichtenstein, TIPP (including MOPP), TAPP and TEP techniques. Their findings highlight Lichtenstein’s clear disadvantage and an indistinguishable difference between TIPP (including MOPP), TAPP and TEP. To further explore the potential benefits of the open preperitoneal approach, consider this study by M. Reinhorn and colleagues [87] which emphasizes the potential benefits of open posterior mesh placement (TREPP) over endoscopic repair in terms of short-term Quality of Life (QoL) and seroma formation, with equivalent hernia recurrence rates. Agarwal et al. [88] show the advantages of TREPP/MOPP over Lichtenstein regarding patient-reported QoL, sustained for a year, and reduced opioid intake 30 days post-surgery. Zwols [89] and Koning [90] also highlight the superiority of preperitoneal techniques over the Lichtenstein method. J.L. Faessen [91] shows in pilot study that TREPP is comparable to TEP and Lichtenstein in terms of recurrence rates, chronic post-operative inguinal pain, and clinically significant adverse events.
Conclusion
Ongoing studies expert are published in the same JAWS special issue provide additional information regarding the treatment of scrotal hernias using the MOPP technique [92], as well as another study comparing the results of the treatment of scrotal hernias using TIPP/MOPP versus Lichtenstein and endoscopic techniques [93]. I hope that this article and the special issue dedicated to the modern preperitoneal minimally invasive route will open lots of eyes. New studies, randomized, or as I think, using smart data from specific databases, must confirm the advantages or equivalences of these techniques compared to the other two groups. It should be interesting to highlight the advantages due to the minimally invasive nature, making it possible to operate on more complex hernias and the most fragile or elderly patients, using a large preperitoneal prosthesis and thus avoiding the Lichtenstein technique more commonly used in these patients. But, at this moment, this is still only the idea of a small percentage of surgeons. As Usher experienced as reported by Read, as Rives experienced and expressed to me, as Fruchaud experienced as reported by Stoppa, innovators often struggle to move their ideas forward and bring them to fruition. This is perhaps what is happening to the promoters of minimally invasive preperitoneal surgery who for nearly 30 years have been campaigning for this third way, having the virtues of the great principles currently accepted and the virtues of less invasiveness, and more economical and more ecological. Time will tell whether this path will have its place or whether it will only delay the use of new technologies for all.
Statements
Author contributions
MS writing, reviewing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Stoppa R Wantz GE Munegato G Pluchinotta A . In: Hernia Healers an Illustrated History, Velizy Villacoublay, Arnette (1998). p. 1–31.
2.
Cooper AP . The Anatomy and Surgical Treatment of Abdominal Hernia (2 Vols). London: Longman (1807).
3.
Bogros AJ . Essai sur L’anatomie Chirurgicale de la Région Iliaque et Description d’un Nouveau Procédé Pour Faire la Ligature des Artères Épigastriques et Iliaque Externe. Th Paris 1823, N° 153.A Paris de L’imprimerie de Didot le Jeune, Imprimeur de La Faculté de Médecine, Rue Des Maçons, Sorbonne N°13 (2025).
4.
Thomson A . Cause Anatomique de la Hernie Inguinale Externe. J des connaissances médicales pratiques de pharmacologie (1836)(4) 137.
5.
Retzius AA . Some Remarks on the Proper Design of the Semilunar Lines of Douglas. With Three Illustrations. Edimb Med J (1858) 3(3):865–7.
6.
Bassini E . Sulla Cura Radicale Dell’ Ernia Inguinale. Arch Soc Ital Chir (1887)(4) 30.
7.
shouldice EE . Surgical Treatment of Hernia. Ontario Med Rev (1945) 12:43.
8.
Fruchaud H . Anatomie chirurgicale des hernies de l’aine. Doin Ed. Paris (1957).
9.
Fruchaud H . Le Traitement Chirurgical des Hernies de L’aine Chez L’adulte. Doin Ed. Paris (1956).
10.
McVAY CB ChAPP JD . Inguinal and Femoral Hernioplasty; the Evaluation of a Basic Concept. Ann Surg (1958) 148:499–512. 10.1097/00000658-195810000-00001
11.
Condon RE . Surgical Anatomy of the Transversus Abdominis and Transversalis Fascia. Ann Surg (1971) 173:1–5. 10.1097/00000658-197101000-00001
12.
Lister BJ . The Classic: On the Antiseptic Principle in the Practice of Surgery. 1867. Clin Orthop Relat Res (2010) 468:2012–6. 10.1007/s11999-010-1320-x
13.
Stoppa R Wantz GE Munegato G Pluchinotta A . Another Battle against Surgical Pain. In: Hernia Healers an Illustrated History. Velizy Villacoublay, France: Arnette (1998). p. 53–4.
14.
Chavasse TF . On a Method of Operating in Strangulated Umbilical Hernia. Lancet (1882) 119:865. 10.1016/S0140-6736(02)23124-4
15.
Niven JA . A New Operation for the Relief of Hernia. Lancet (1861) 77:276. 10.1016/S0140-6736(02)42094-6
16.
Annandale T . Case in Which a Reducible Oblique and Direct Inguinal and Femoral Hernia Existed on the Same Side and Were Successfully Treated by Operation. Edinb Med J (1876) 21:1087–91.
17.
Tait L . A Discussion on Treatment of Hernia by Median Abdominal Section. Br Med J (1891)(2) 685–91. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2273659/pdf/brmedj04407-0007.pdf (Accessed June–September, 2024).
18.
Bates VC . New Operation for the Cure of Indirect Inguinal Hernia. JAMA (1913) 60(26):2032–3. 10.1001/jama.1913.04340260006003
19.
Cheatle GL . An Operation for the Radical Cure of Inguinal and Femoral Hernia. Br Med J (1920) 2:68–9. 10.1136/bmj.2.3107.68
20.
Patino JF . A History of the Treatment of Hernia. In: NyhusLMCondonRE, editors. Hernia. 4th ed. Philadelphia: J.B.Lippincott Company (1995). p. 3–15.
21.
Patiño JF . The Nyhus Preperitoneal Repair of Groin Hernias. In: BendavidRAbrahamsonJArreguiMEFlamentJBPhillipsEH, editors. Abdominal Wall Hernias. New York, NY: Springer (2001). p. 391–5. 10.1007/978-1-4419-8574-3_58
22.
Henry AK . Operation for Femoral Hernia by a Midline Preperitoneal Approach: With a Preliminary Note on the Use of This Route for Reducible Inguinal Hernia. Lancet (1936) 1:531–3.
23.
Mc Evedy BV . The Internal Approach for Inguinal Hernia. Posgrad Med J (1966) 42:548–50. 10.1136/pgmj.42.491.548
24.
Acquaviva DE Bourret P Corti D . Considérations sur l’emploi des plaques de nylon dites crinoplaques comme matériel de plastie pariétale. Cong fr de chirurgie. Paris: Masson (1949). p. 453.
25.
Soler M Giuly JA Bendavid R . Don Eugène Acquaviva (1897-1976): The Real Founder of Modern Parietology Using a Prosthetic Mesh. Hernia (2021) 25:1733–5. 10.1007/s10029-021-02398-5
26.
Corti D . Nylon et plastie. Marseille, France: University of Marseille (1949). [Thesis]. [Marseille, France](Personal collection).
27.
Bourgeon R Guntz M . Notre Expérience de la Thérapeutique des Vastes Hernies Inguinales par Plaque de Nylon. Afrique Française chirurgicale (1955) 423–7.
28.
Bourgeon R Borecelli J Masson J . La Technique des Cures de Hernies de L’aine par Plaque de Nylon. Nice Med (1970) 8:97.
29.
Read RC Francis C . Usher Herniologist of the Twentieth Century. Hernia (1999) 3:167–71. 10.1007/BF01195320
30.
Usher FC Allen JE Jr Crosthwait RW Cogan JE . Polypropylene Monofilament. A New Biologically Inert Suture for Closing Contaminated Wounds. J Am Med Assn (1962) 10(179):780–2. 10.1001/jama.1962.03050100034006b
31.
Usher FC Wallace SA . Tissue Reaction to Plastics; a Comparison of Nylon, Orlon, Dacron, Teflon, and Marlex. Arch Surg (1958) 76:997–9.
32.
Usher FC Gannon JP . Marlex Mesh, a New Plastic Mesh for Replacing Tissue Defects. I. Experimental Studies. Arch Surg (1959) 78:131–7. 10.1001/archsurg.1959.04320010133022
33.
Usher FC Fries JG Ochsner JL Tuttle LL Jr . Marlex Mesh, a New Plastic Mesh for Replacing Tissue Defects. II Clinical Studies. Arch Surg (1959) 78:138–45. 10.1001/archsurg.1959.04320010140023
34.
Usher FC Hill JR Ochsner JL . Hernia Repair With Marlex Mesh. A Comparison of Techniques. Surgery (1959) 46:718–24.
35.
Usher FC Cogan GE Lowry TI . A New Technique for the Repair of Inguinal and Incisional Hernias. Arch Surg (1960) 81:847–54. 10.1001/archsurg.1960.01300050169030
36.
Usher FC Knitted Marlex Mesh. An Improved Marlex Prosthesis for Repairing Hernias and Other Tissue Defects. Arch Surg (1961) 82: 771–3. 10.1001/archsurg.1961.01300110133017
37.
Usher FC . Hernia Repair With Marlex Mesh. An Analysis of 541 Cases. Arch Surg (1962) 84:325–8. 10.1001/archsurg.1962.01300210059012
38.
Usher FC . Hernia Repair With Knitted Polypropylene Mesh. Surg Gynec Obstet (1963) 117:239–40. Available from: https://pubmed.ncbi.nlm.nih.gov/14048019/ (Accessed June–September, 2024).
39.
Read RC . Prosthesis in Abdominal Wall Hernia Surgery. In: BendavidR, editor. Prosthesis and Abdominal Wall Hernias, 5. Austin, TX: R.G. Landes Company (1994). ((Read: Usher said: Surgeon reluctant to use a prosthesis)).
40.
Debord JR . The Historical Development of Prosthetics in Hernia Surgery. Surg Clin North Am (1998) 78:973–1006. 10.1016/S0039-6109(05)70365-0
41.
Duron JJ . Clinical Application of Stainless Mesh. In: BendavidRAbrahamsonJArreguiMEFlamentJBPhillipsEH, editors. Abdominal Wall Hernias. New York, NY: Springer (2025). p. 258–61. 10.1007/978-1-4419-8574-3_33
42.
Recorded Interview With Jean Rives Conducted at His Parisian Home on Oct 6, 2011. (2025). Unpublished. Author's personal collection.
43.
Nyhus LM Stevenson LM Listerud MB Harkins HN . Preperitoneal Herniorrhaphy; a Preliminary Report in Fifty Patients. West J Surg Obstet Gynecol (1959) 67:48–54. Available from: https://pubmed.ncbi.nlm.nih.gov/13636181/ (Accessed June–September, 2024).
44.
Nyhus LM Condon RE Harkins HN . Clinical Experiences With Preperitoneal Hernial Repair for All Types of Hernia of the Groin, With Particular Reference to the Importance of Transversalis Fascia Analogues. Am J Surg (1960) 100:234–44. 10.1016/0002-9610(60)90296-8
45.
Fruchaud H . The Surgical Anatomy of Hernias of the Groin. In: BendavidBRRCunninghamP, editors. Translated. Toronto (2006).
46.
Rives J Stoppa R Fortesa L Nicaise H . Les Pièces en Dacron et Leur Place Dans la Chirurgie des Hernies de L’aine. a Propos de 65 Cas Recueillis sur une Statistique Intégrale de 274. Ann Chir (1968) 22:159–71. Available from: https://pubmed.ncbi.nlm.nih.gov/4247384/ (Accessed June–September, 2024).
47.
Rives J Lardennois B Flament JB Couvert G . La Pièce en Tulle de Dacron, Traitement de Choix des Hernies de L’aine de L’adulte. A Propos de 183 cas. Chirurgie (1973) 99:564–75. Available from: https://pubmed.ncbi.nlm.nih.gov/4277952/ (Accessed June–September, 2024).
48.
Stoppa R Petit J Abourachid H Henry X Duclaye C Monchaux G et al Procédé Original de Plastie des Hernies de L'aine. L'interposition Sans Fixation D'une Prothèse en Tulle de Dacron par Voie Médiane Sous-Péritonéale. Chirurgie (1973) 99:119–23. Available from: https://pubmed.ncbi.nlm.nih.gov/4269677/ (Accessed June–September, 2024).
49.
Stoppa R Rives J Warlaumont C Palot JP Verhaeghe P Delattre JF et al The Use of Dacron in the Repair of Hernias of the Groin. Surg Clin North Am (1984) 64:269–85. 10.1016/s0039-6109(16)43284-6
50.
Verhaeghe P . Technique De Stoppa. In: Vidéo-Atlas Chirurgie Herniaire Tome 1. Paris: Springer (2010). 10.1007/978-2-8178-0148-3_23
51.
Wantz GE . Unilateral Giant Prosthesis Reinforcement of the Visceral Sac. In: WantzGE, editor. Atlas of Hernia Surgery. New York, NY: Raven Press (1991). p. 133–51.
52.
Alexandre JH Dupin P Levard H Billebaud T . Treatment of Inguinal Hernia With Unsplit Mersylene Prosthesis. Significance of the Parietalization of the Spermatic Cord and the Ligation of Epigastric Vessels. Presse Med. Presse Med (1984) 13:161–3.
53.
Alexandre JH Bouillot JL Dupin P Aouad K Bethoux JP . Cure of Inguinal Hernias With Large Preperitoneal Prosthesis: Experience of 2,312 Cases. J Minim Access Surg (2006) 2(3):134–8. 10.4103/0972-9941.27725
54.
Kugel RD . The Kugel Repair for Groin Hernias. In: BendavidR, editor. Abdominal Wall Hernias. Principles and Management. New-York: Springer-Verlag (2001). p. 504–7.
55.
The HerniaSurge Group. International Guidelines for Groin Hernia Management. Hernia (2018) 22:1–165. 10.1007/s10029-017-1668-x
56.
Ugahary F Simmermacher R . Groin Hernia Repair Via a Grid-Iron Incision: An Alternative Technique for Preperitoneal Mesh Incision. Hernia (1998) 2(3):1232–125. 10.1007/BF01250028
57.
Ugahary F . The Gridiron Hernioplasty. In: BendavidRAbrahamsonJArreguiMEFlamentJB, editors. Abdominal Wall Hernias Principles and Management. New York: Springer-Verlag (2001). p. 407–11.
58.
Pelissier EP . Inguinal Hernia: Preperitoneal Placement of a Memory-Ring Patch by Anterior Approach. Preliminary Experience. Hernia (2006) 10:248–52. 10.1007/s10029-006-0079-1
59.
Pélissier EP Girard JF . Herniorraphie Inguinale Sous Anesthésie Locale Avec Hospitalisation Brève Inguinal Herniorrhaphy Under Local Anesthesia With Short Hospitalization. Chirurgie (1991) 117(2):186–8.
60.
Pélissier EP Blum D . Herniorraphie Type Bassini-Houdard. Résultats à Long-Terme et Facteurs de Récidive The Bassini-Houdard Type herniorhaphy. Long-Term Results and Factors of Recurrence. Chirurgie (1993) 119(5):252–5.
61.
Interview With Edouard Pelissier in 2024. (1991). Unpublished. Author's personal collection.
62.
Gilbert AI . Sutureless Repair of Inguinal Hernia. Am J Surg (1992) 163:331–5. 10.1016/0002-9610(92)90015-J
63.
Rutkow IM Robbins AW . Tension Free Inguinal Herniorrhaphy: A Preliminary Report on the “Mesh Plug” Technique. Surgery (1993) 114:3–8.
64.
Pelissier EP Blum D . The Plug Method in Inguinal Hernia: Prospective Evaluation of Postoperative Pain and Disability. Hernia (1997) 1(4):185–9. 10.1007/BF01234756
65.
Berrevoet F Sommeling C De Gendt S Breusegem C De Hemptinne B . The Preperitoneal Memory-Ring Patch for Inguinal Hernia: A Prospective Multicentric Feasibility Study. Hernia (2009) 13(3):243–9. 10.1007/s10029-009-0475-4
66.
Berrevoet F Maes L Reyntjen s K Rogiers X Troisi R de Hemptinne B . Transinguinal Preperitoneal Memory Ring Patch Versus Lichtenstein Repair for Unilateral Inguinal Hernias. Langenbecks Arch Surg (2010) 395(5):557–62. 10.1007/s00423-009-0544-2
67.
Gillion JF Chollet JM . Chronic Pain and Quality of Life (QoL) After Transinguinal Preperitoneal (TIPP) Inguinal Hernia Repair Using a Totally Extraperitoneal, Parietalized, Polysoft ® Memory Ring Patch: A Series of 622 Hernia Repairs in 525 Patients. Hernia (2013) 17:683–92. 10.1007/s10029-013-1121-8
68.
Gillion JF Pelissier E . Transinguinal Preperitoneal (TIPP) Inguinal Hernia Repair Using a Totally Extraperitoneal, Parietalized, Memory-Ring Patch. In: CampanelliG, editor. The Art of Hernia Surgery. Cham: Springer (2018). 10.1007/978-3-319-72626-7_31
69.
Lourenco A Da Costa RS . The ONSTEP Inguinal Hernia Repair Technique: Initial Clinical Experience of 693 Patients, in Two Institutions. Hernia (2013) 17:357–64. 10.1007/s10029-013-1057-z
70.
Interview With Franz Ugahary in 2024 Unpublished. (2025). Author's personal collection.
71.
Letter From René Stoppa Addressed to F. Ugahary on October 31. (1997). personal collection.
72.
Soler M Ugahary F . E-Memories of the National Academy of Surgery (2004) 3:28–33. Available from: https://e-memoire.academiechirurgie.fr/ememoires/005_2004_3_3_28x33.pdf. (Accessed June–September, 2024).
73.
Kugel RD . Minimally Invasive, Non Laparoscopic, Preperitoneal, and Sutureless, Inguinal Herniorrhaphy. Am J Surg (1999) 178(4):298–302. 10.1016/s0002-9610(99)00181-66
74.
Kugel RD . The Kugel Repair for Groin Hernias. Surg Clin North Am (2003) 83(5):1119–39. 10.1016/S0039-6109(03)00123-3
75.
Soler M . Technique De Grid-Iron Ugahary. In: Vidèo-Atlas Chirurgie Herniaire Tome 1. Paris: Springer (2010). 10.1007/978-2-8178-0148-3_21
76.
Beck M Gillion JF Soler M . Traitement des hernies de l’aine par voie inguinale. EMC. Techniques chirurgicales - Appareil digestif. Numéro 2 (2022) Vol. 39:1–23. Copyright © 2022 Elsevier Masson SAS. 10.1016/s0246-0424(22)43306-1
77.
Soler M . The Minimal Open Preperitoneal (MOPP) Approach to Treat the Groin Hernias, With the History of the Preperitoneal Approach. Ann Laparosc Endosc Surg (2017) 2:133. 10.21037/ales.2017.06.08
78.
Soler M . Minimal Open Preperitoneal (MOPP) Technique. In: CampanelliG, editor. The Art of Hernia Surgery A Step-by-step Guide. Milan: Springer (2018). p. 319–26.
79.
Soler M . The Minimal Open Preperitoneal (MOPP) Approach for Treating Groin Hernias: Technique, Indications, and Results. Ann Laparosc Endosc Surg (2024) 9:3. 10.21037/ales-23-37
80.
Koning GG Andeweg CS Keus F van Tilburg MW van Laarhoven CJ Akkersdijk WL The Transrectus Sheath Preperitoneal Mesh Repair for Inguinal Hernia: Technique, Rationale, and Results of the First 50 Cases. Hernia (2012) 16(3):295–9. 10.1007/s10029-011-0893-y
81.
Akkersdijk WL Andeweg CS Bokkerink WJ Lange JF van Laarhoven CJ Koning GG . Teaching the Transrectus Sheath Preperiotneal Mesh Repair: TREPP in 9 Steps. Int J Surg (2016) 30:150–4. 10.1016/j.ijsu.2016.04.037
82.
Lange JF Lange MM Voropai DA van Tilburg MW Pierie JP Ploeg RJ et al Trans Rectus Sheath Extra-Peritoneal Procedure (TREPP) for Inguinal Hernia: The First 1,000 Patients. World J Surg (2014) 38(8):1922–8. 10.1007/s00268-014-2475-5
83.
Bökkerink WJ Persoon AM Akkersdijk WL van Laarhoven CJ Koning GG . The TREPP as Alternative Technique for Recurrent Inguinal Hernia After Lichtenstein’s Repair: A Consecutive Case Series. Int J Surg (2017) 40:73–7. 10.1016/j.ijsu.2017.02.022
84.
Persoon AM Bökkerink WJV Akkersdijk WL van Laarhoven CJHM Koning GG . Case Series of Recurrent Inguinal Hernia After Primary TREPP Repair: Re-TREPP Seems Feasible and Safe. Int J Surg Case Rep (2018) 51:292–5. 10.1016/j.ijscr.2018.08.060
85.
Interview with Willem Akkersdijk. (2024). Unpublished. Author's personal collection.
86.
Hurel R Bouazzi L Barbe C Kianmanesh R Romain R Gillion JF et al Lichtenstein versus TIPP versus TAPP Versus TEP for Primary Inguinal Hernia, a Matched Propensity Score Study on the French Club Hernie Registry. Hernia (2023) 27:1165–77. 10.1007/s10029-023-02737-8
87.
Reinhorn M Fullington N Agarwal D Olson MA Ott L Canavan A et al Posterior Mesh Inguinal Hernia Repairs: A Propensity Score Matched Analysis of Laparoscopic and Robotic Versus Open Approaches. Hernia (2023) 27:93–104. 10.1007/s10029-022-02680-0
88.
Agarwal D Bharani T Fullington N Ott N Olson M Poulose B et al Improved Patient-Reported Outcomes after Open Preperitoneal Inguinal Hernia Repair Compared to Anterior Lichtenstein Repair: 10-Year ACHQC Analysis. Hernia (2023) 27:1139–54. 10.1007/s10029-023-02852-6
89.
Zwols TLR Slagter N Veeger NJGM Mollers MJM Hess DA Jutte E et al Transrectus Sheath Pre-Peritoneal (TREPP) Procedure Versus Totally Extraperitoneal (TEP) Procedure and Lichtenstein Technique: A Propensity-Score-Matched Analysis in Dutch High-Volume Regional Hospitals. Hernia (2021) 25:1265–70. 10.1007/s10029-020-02291-7
90.
Koning GG Keus F Koeslag L Cheung CL Avçi M Van laarhoven CJHM et al Randomized Clinical Trial of Chronic Pain After the Transinguinal Preperitoneal Technique Compared With Lichtenstein’s Method for Inguinal Hernia Repair. Br J Surg (2012) 99:1365–73. 10.1002/bjs.8862
91.
Faessen JL Stoot JHMB Van Vugt R Safety and Efficacy in Inguinal Hernia Repair: A Retrospective Study Comparing TREPP, TEP and Lichtenstein (SETTLE). Hernia (2021) 25:1309–15. 10.1007/s10029-020-02361-w
92.
Soler M Gillion FJ . Are ‘European’ Scrotal Hernias Repairable with the Minimal Open Pre-peritoneal Technique (MOPP)? in Press JAWS Special Issue. (2024).
93.
Metoudi A Gillion JF Soler M . TIPP/MOPP versus Lichtenstein and Laparoscopic Techniques for Large Inguinoscrotal Hernia Repair: A Comprehensive Registry-Based Study. (2024). In press JAWS special issue
Summary
Keywords
prosthesis, groin hernia, history, open, preperitoneal
Citation
Soler M (2025) Groin Hernia Repair, the History of the Open Pre-Peritoneal Route Towards a Minimally Invasive Approach. Narrative Review. J. Abdom. Wall Surg. 4:13861. doi: 10.3389/jaws.2025.13861
Received
28 September 2024
Accepted
15 January 2025
Published
17 February 2025
Volume
4 - 2025
Updates
Copyright
© 2025 Soler.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marc Soler, soler.marc2@wanadoo.fr
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.