Abstract
Background: The nature of itch sensation varies depending upon the patient and the disease. However, few studies have focused on verbal expressions describing itch of atopic dermatitis (AD) in quality.
Objectives: To investigate itch quality in patients with AD compared with that of urticaria.
Methods: We conducted an online questionnaire survey describing itch experiences in June 2021. Participants were Japanese patients who had visited hospitals for their consultations and treatments of AD or urticaria in the last 6 months, and 295 and 290 responses, respectively, to questions using 12 terms describing itch quality were analyzed.
Results: The most suitable expression describing intense itch that patients could not help scratching differed between the diseases, where most AD patients selected “muzumuzu” (a mimetic word for creepy–crawly itch) (27%) or “painful itch” (20%), and most urticaria patients selected “muzumuzu” (24%) or “itch like mosquito bites” (22%). The most suitable expressions describing itch that would make patients happiest if improved was “painful itch” (27%) in AD patients, significantly higher than urticaria patients (19%). More AD patients (55%) responded that they sometimes felt itch even after the skin symptoms had subsided than urticaria patients (41%). The most suitable expression of remnant itch selected was “muzumuzu” for AD (58/161 patients, 36%) and urticaria (29/120 patients, 24%).
Conclusion: The quality of itch sensations can be classified not only between diseases but also during the clinical course of each disease. Significant expressions that patients with AD use to describe itch sensations could promote more appropriate treatment for itch.
Introduction
Itch is the most burdensome symptom in all age groups with atopic dermatitis (AD). It is associated with the development of sleep disorders, psychiatric disorders, and impaired quality of life in patients [1, 2]. The perception of itch is very personal and subjective and varies not only in intensity but also in its triggers, the time of day and season, the body area involved, and treatment methods, depending on the patient. Itch is sometimes severe despite mild skin symptoms in AD [3, 4]. Therefore, it is important to focus on itch as well as skin symptoms for the treatment of AD.
The nature of itch sensation may also vary depending on the individual patient and the disease. If we know how patients perceive and express their feeling of itch using words, we can assess the quality of itch. The visual analog scale and numerical rating scale (NRS) commonly used to evaluate itch can only assess the intensity of itch felt by patients. The classification of itch based on differences in itch quality may help choose and develop more appropriate treatments. However, few studies have examined the quality of itch [4–7].
This study was therefore conducted an online questionnaire to investigate the quality of itch using verbal expressions describing itch felt by patients. The participants were patients with AD and were compared with those with urticaria. We, here, described their frequency of use and associations with severity, site, season, time of day, and treatment response for the expressions describing itch and compared them between the diseases.
Materials and methods
Questionnaire and participants
An advance survey was conducted to collect Japanese expressions commonly used to describe the itch sensation by patients with AD or urticaria as answers to an open-ended question. After excluding emotional words such as “troublesome” or “unbearable” from the collected expressions, we grouped similar terms together and prepared typical candidate expressions based on other previous studies [4–6]. The Atopic Itch Consensus Meeting members, which comprised dermatologists, pediatricians, allergists, and basic researchers of itch (Supplementary Table S1), discussed the candidate expressions and determined a list of 12 terms describing itch that responders could select in the questionnaire (Table 1).
TABLE 1
| 1 | Itch like insect crawling |
|---|---|
| 2 | Chikuchiku (prickly itch, like wearing a sweater right on the skin) |
| 3 | Muzumuzu (creepy-crawly itch, a bit like tickling) |
| 4 | Piripiri (like tingling) |
| 5 | Burning itch |
| 6 | Tickling itch |
| 7 | Itch like mosquito bites |
| 8 | Painful itch |
| 9 | Itch like being pressed |
| 10 | Itch like being pinched |
| 11 | Hard to describe itch |
| 12 | Others |
Twelve terms used to describe itch sensations.
Phrases in parenthesis are English explanations of Japanese ideophones.
In June 2021, we conducted an online questionnaire survey through Macromill Carenet, Inc., an online survey company (Tokyo, Japan). This study required no ethics approval because of its use of completely anonymized data of the study participants, with no patient contact involvement. A questionnaire, written in Japanese, was distributed to patients with AD or urticaria registered on a panel of >10 million people across Japan assembled by Macromill and recruited for the study. The target sample size was set at 270 for each disease, although no statistical hypotheses were proposed. Furthermore, the sample consisted of 50 patients in each age group (7–15, 16–25, 26–35, 36–45, and 46–64 years old) and 20 patients aged ≥65 because of low prevalence. Patients aged 7–15 years were first-born children, and their responses were provided by their parents.
The screening questionnaire stated the purposes of the survey and asked patients who had visited hospitals for AD or urticaria in the last 6 months to answer questions. Those who gave voluntary informed consent were included in the analysis. All data were anonymized by Macromill Carenet and supplied to Maruho Co., Ltd. (Osaka, Japan) for the analysis.
The questionnaire included the following items: [1] patient information, including sex, age, disease duration, NRS score for the most intense itch for the last week, and prescribed therapeutic drugs; [2] regarding expressions describing intense itch that patients experienced at least once and could not help scratching, all expressions describing experienced itch (multiple choice) and one expression that best described their itch on the list of 12 terms (single choice, hereafter referred to as the most suitable expression); [3] the body area, season, and time of day at which they often experienced intense itch and the most suitable expression describing the itch; and [4] the most suitable expression describing the itch sensation that made them happiest if improved (single choice), [5] all expressions describing the itch improved by therapeutics (multiple choice), and [6] all expressions (multiple choice) and the most suitable expression (single choice) describing the itch felt even after the skin symptoms subsided.
NRS scores were categorized as mild (0–3 points), moderate (4–6 points), and severe itch (7–10 points).
Statistical analysis
The proportion of patients who had experienced the situation in question and the proportion of the most suitable expression describing the itch that the patients selected were calculated. In the calculations, the denominators excluded patients who were ineligible for each question. The proportions were compared between the AD and urticaria groups using Fisher’s exact test. Because these comparisons were exploratory, no correction was used to adjust for multiple testing. All statistical analyses were performed using IBM SPSS Statistics 28.0 (IBM Corp, Armonk, NY, United States).
Results
Background of the respondents with AD or urticaria
Responses from 295 patients with AD and 290 patients with urticaria were included in the AD and urticaria groups, respectively. The patients’ background characteristics are shown in Table 2. More women were included in the urticaria group than in the AD group. The most common severity grade for the last week using the NRS for the most intense itch was “moderate” in the AD group, whereas it was “severe” in the urticaria group. The disease duration of the AD group ranged from 6 months to >30 years. Among the patients in the AD and urticaria groups, 288 (97.6%) and 277 (95.5%), respectively, received prescribed drugs at present.
TABLE 2
| Atopic dermatitis (n = 295) | Urticaria (n = 290) | ||||
|---|---|---|---|---|---|
| Age group (years) | 7–15 | 54 | 18.3% | 51 | 17.6% |
| 16–25 | 55 | 18.6% | 52 | 17.9% | |
| 26–35 | 55 | 18.6% | 55 | 19.0% | |
| 36–45 | 55 | 18.6% | 55 | 19.0% | |
| 46–64 | 55 | 18.6% | 55 | 19.0% | |
| ≥65 | 21 | 7.1% | 22 | 7.6% | |
| Sex | Male | 124 | 42.0% | 82 | 28.3% |
| Female | 171 | 58.0% | 208 | 71.7% | |
| Itch severity for the last week (NRS score) | 0–3 (Mild) | 87 | 29.5% | 98 | 33.8% |
| 4–6 (Moderate) | 124 | 42.0% | 90 | 31.0% | |
| 7–10 (Severe) | 84 | 28.5% | 102 | 35.2% | |
| Disease duration (years) | <5 | 48 | 16.3% | NA | - |
| 5–9 | 41 | 13.9% | NA | - | |
| 10–19 | 49 | 16.6% | NA | - | |
| 20–29 | 64 | 21.7% | NA | - | |
| ≥30 | 93 | 31.5% | NA | - | |
| Type of urticaria | Acute | NA | - | 91 | 31.4% |
| Chronic | NA | - | 199 | 68.6% | |
| Therapeutic drugs at present | Topical steroids | 263 | 89.2% | 141 | 48.6% |
| Tacrolimus ointment | 68 | 23.1% | NA | - | |
| Delgocitinib ointment | 18 | 6.1% | NA- | - | |
| Topical antihistamines | NA | - | 77 | 26.6% | |
| Oral antiallergic drugs/oral antihistamines | 94 | 31.9% | 195 | 67.2% | |
| Oral steroids | 31 | 10.5% | 45 | 15.5% | |
| Oral cyclosporine | 7 | 2.4% | NA | - | |
| Emollients | 161 | 54.6% | NA- | - | |
| Biologics | 1 | 0.3% | 5 | 1.7% | |
| Others | 10 | 3.4% | 11 | 3.8% | |
| No medication | 7 | 2.4% | 13 | 4.5% | |
Patients’ characteristics.
Data are presented as the number and percentage of patients.
Abbreviations: NA, not applicable (not set as an option); NRS, numerical rating scale.
Expressions describing intense itch that patients cannot help scratching
The proportion of all the expressions describing intense itch that patients could not help scratching were shown in Figure 1A; Supplementary Table S2. Common terms were “muzumuzu” (creepy-crawly itch, a bit like tickling) (63%), “painful itch” (48%), and “chikuchiku” (prickly itch, like wearing a sweater right on skin) (33%) in the AD group. Many patients with AD experienced itch that was described by these terms compared with urticaria patients. In the urticaria group, common terms describing intense itch were “muzumuzu” (53%), “itch like mosquito bites” (41%), and “painful itch” (37%). The most suitable expression of intense itch was “muzumuzu” in both groups (AD, 29% vs. urticaria, 25%) (Figure 1B; Supplementary Table S2). However, the second and third expressions were different between the two groups. These were “painful itch” (21%) and “hard to describe itch” (14%) in the AD group but “itch like mosquito bites” (23%) and “painful itch” (17%) in the urticaria group. Comparing AD and urticaria, the proportions of patients who felt “itch like mosquito bites” and “burning itch” were significantly higher for urticaria than for AD, whereas “chikuchiku” was significantly higher for AD (10%) than for urticaria (4%).
FIGURE 1
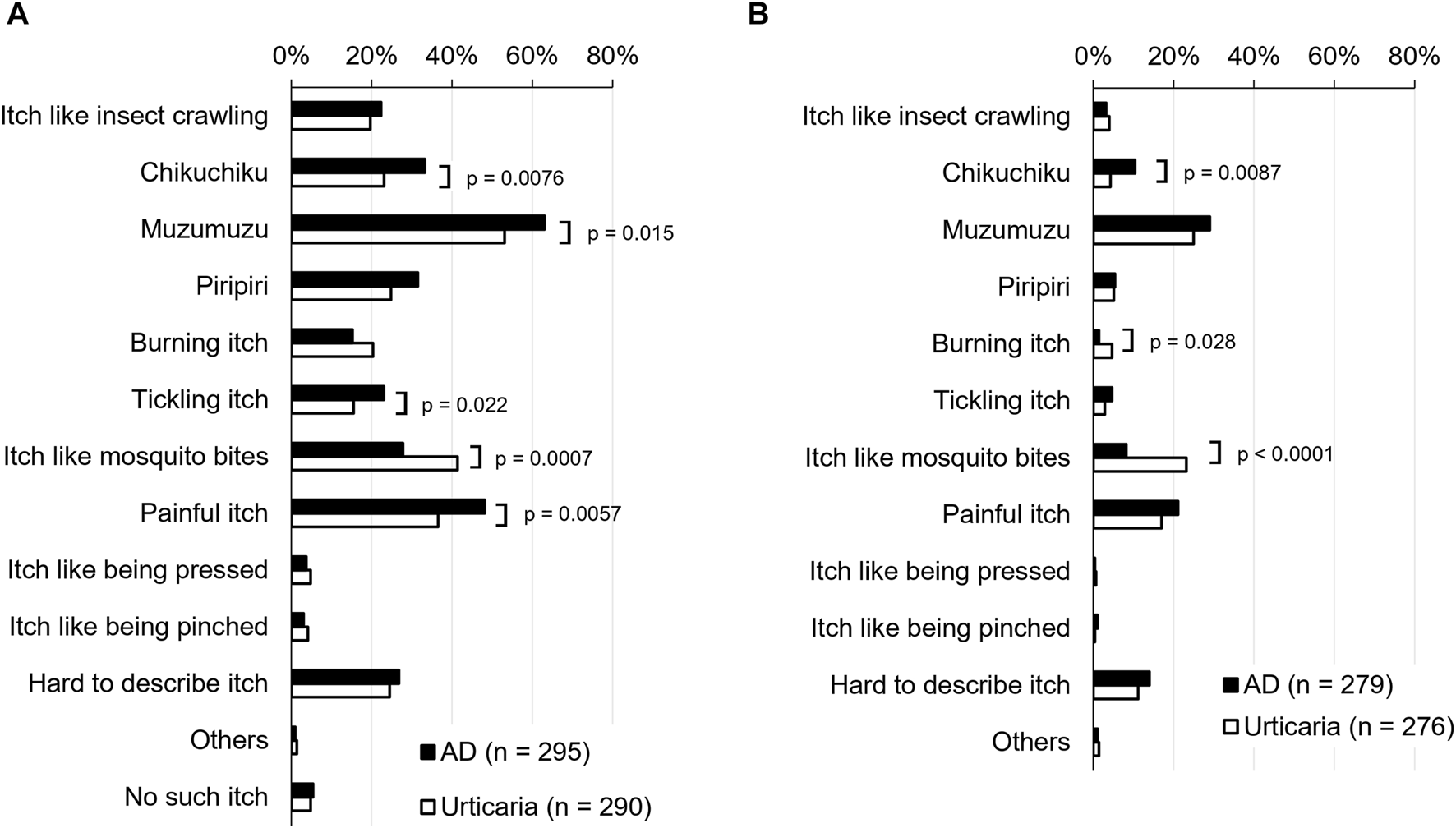
Expressions describing intense itch that patients experienced at least once and could not help scratching. (A) Proportion of all the expressions describing experienced itch (multiple choice). (B) Proportion of one expression that was the most suitable of 12 terms (single choice). AD, atopic dermatitis.
The mean number of expressions describing intense itch selected by AD patients was 2.1 for children aged 7–15 years (n = 54) and 3.2 for those ≥16 years (n = 241). Therefore, children aged 7–15 years experienced itch at an overall lower proportion of patients than those aged ≥16 years in the AD group (Supplementary Figure S1A). In contrast, the mean number of expressions selected by patients with urticaria was 2.5 for those aged 7–15 years (n = 51) and 2.7 for those ≥16 years (n = 239), suggesting similar number regardless of age (Supplementary Figure S1B).
The mean number of expressions describing intense itch increased with severity for the last week as per grading using the NRS. The mean numbers for mild, moderate, and severe grades were 2.3, 3.0, and 3.7, respectively, in the AD group and 2.2, 2.7, and 3.2, respectively, in the urticaria group. Overall, the most suitable expressions describing intense itch were similar regardless of NRS severity (Supplementary Figure S2).
Comparisons with body area, season, and time of day in which patients often experienced intense itch
The most predominant area, season, and time of day in which patients with AD and urticaria most frequently feel an intense itch were almost similar between the AD and urticaria groups (Supplementary Figure S3). However, the most suitable expression varied with body area, season, and time of day in AD. Of the most suitable expressions for frequent itch areas, “painful itch” for hands (31%) and legs/knees (35%) and “muzumuzu” for arms/elbows (30%) were selected more in the AD group. In the urticaria group, “itch like mosquito bites” and “muzumuzu” were selected more commonly for the above most frequent areas with intense itch (Supplementary Table S3).
Among the most suitable expressions describing itch for season in the AD group, “muzumuzu” was most common in spring, autumn, and all seasons, and “painful itch” was most common in summer and winter. In the urticaria group, “muzumuzu” was most common in spring and summer, “itch like mosquito bites” in winter and all seasons, and “chikuchiku” in autumn (Supplementary Table S4).
Of the most suitable expressions describing itch in the evening and at bedtime, “muzumuzu” was selected most frequently for both AD (32%) and urticaria (34%). Also at night, “muzumuzu” was the most frequent in the AD group (37%) (Supplementary Table S5).
Expressions describing itch in association with treatment
Expressions describing itch that would make patients happiest if improved were “painful itch” (27%) and “muzumuzu” (23%) in AD patients and “muzumuzu” (23%), “itch like mosquito bites” (22%), and “painful itch” (19%) in urticaria patients (Figure 2; Supplementary Table S6). The proportion of AD patients who selected “painful itch” was significantly higher than that of urticaria patients. The proportion of urticaria patients who selected “itch like mosquito bites” was significantly higher than that of AD patients.
FIGURE 2
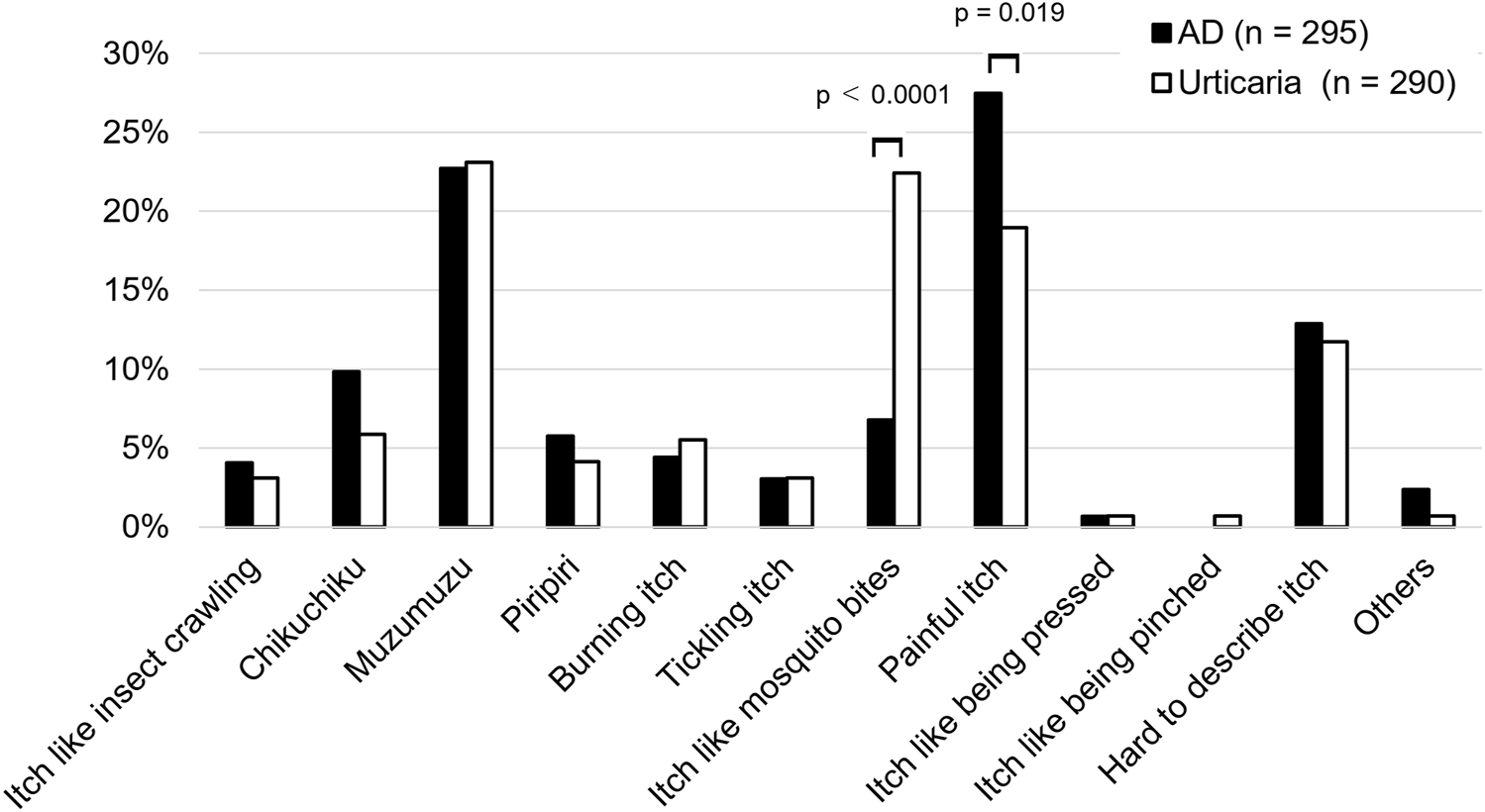
Expressions describing the itch that would make patients happiest if improved (single choice). Data are presented as the proportion of patients. AD, atopic dermatitis.
AD patients commonly (≥60%) selected “painful itch” and “muzumuzu” as intense itch that improved with treatment. In urticaria patients, “hard to describe itch,” “chikuchiku,” “itch like mosquito bites,” “painful itch,” and “muzumuzu” were commonly selected (Supplementary Table S7).
Many patients experienced itch even after skin symptoms had subsided. However, a significant difference in proportion was observed between the AD (161/295 patients, 55%) and urticaria (120/290 patients, 41%) groups (p = 0.0016) (Figure 3). The proportion of patients by itch severity for the last week was higher in patients with more severe disease, regardless of the disease (Figure 3). The most common expressions describing itch that AD patients experienced even after skin conditions subsided were “muzumuzu” (63%) and “painful itch” (33%) (Figure 4A; Supplementary Table S8). The most suitable expressions selected were “muzumuzu” (36%), “painful itch” (13%), and “hard to describe itch” (13%) (Figure 4B; Supplementary Table S8). In urticaria patients, the most common types of itch were “muzumuzu,” (54%) “itch like mosquito bites,” (35%) and “painful itch” (32%) (Figure 4A; Supplementary Table S8). The most suitable expressions describing itch in urticaria were also “muzumuzu,” (24%) “itch like mosquito bites,” (17%) and “painful itch” (16%) (Figure 4B; Supplementary Table S8). Comparing the most suitable expressions describing itch, the proportion of patients with AD who selected “muzumuzu” was significantly higher than those with urticaria. However, the proportion of urticaria patients who selected “itch like mosquito bites” was significantly higher than that of AD patients.
FIGURE 3
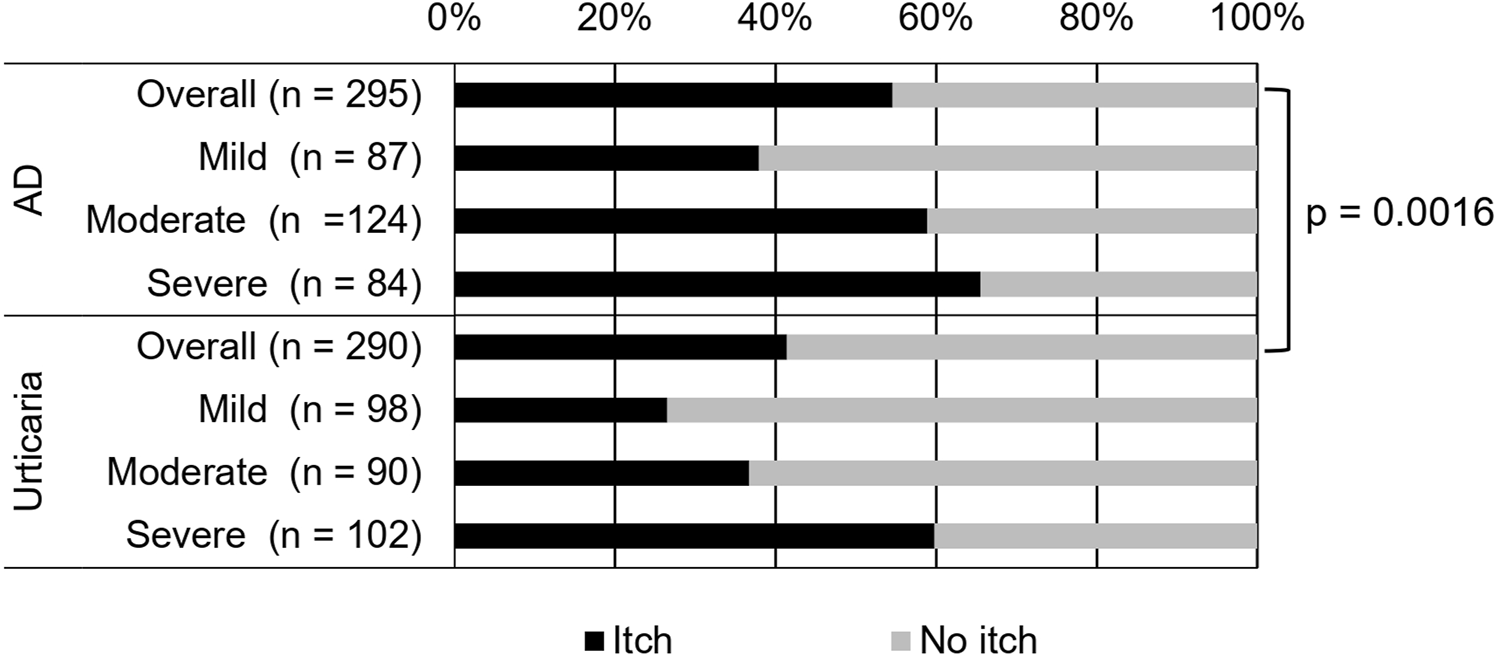
Proportion of patients with an itch symptom even after skin symptoms subsided. The overall proportion and the proportion of patients by itch severity for the last week are shown. AD, atopic dermatitis.
FIGURE 4
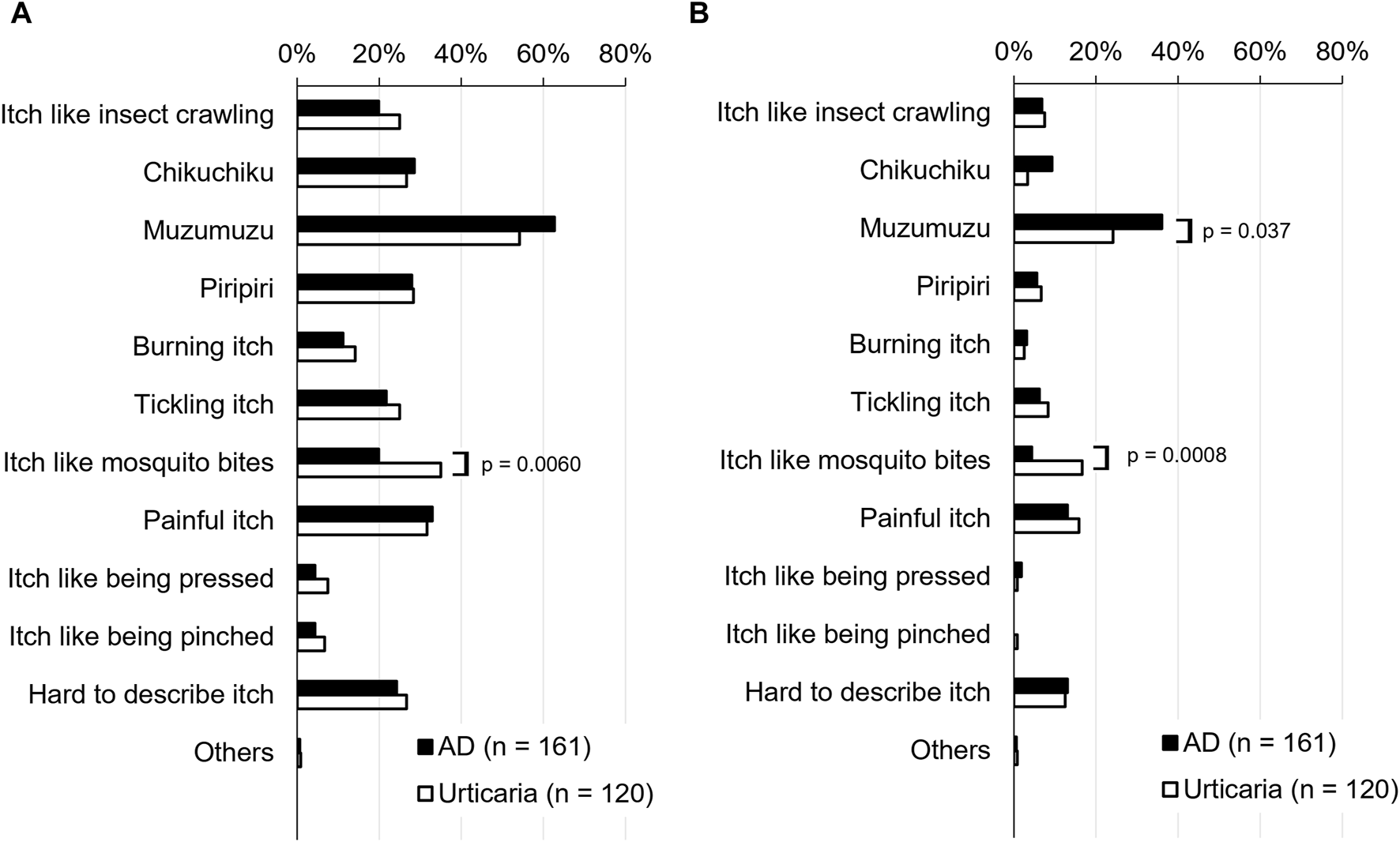
Expressions describing itch felt after skin symptoms subsided. (A) Proportion of all the expressions describing experienced itch (multiple choice). (B) Proportion of one expression that was the most suitable of 12 terms (single choice). AD, atopic dermatitis.
Discussion
Japanese is a language that extensively uses mimetic words (ideophones), which are also often used to express itch sensations [8]; for example, “muzumuzu,” “chikuchiku,” and “piripiri.” Although it is difficult to correctly translate them into English, we have shown English explanations in Table 1.
Patients with AD and urticaria used various expressions describing the itch sensations they experienced, and the itch sensations felt by patients were not homogeneous or uniform. The primary terms for itch sensations were “muzumuzu” and “painful” in AD patients, and “muzumuzu,” “itch like mosquito bites,” and “painful itch” in urticaria patients. In this study, we found significant differences in the proportion of AD and urticaria patients using the expressions “muzumuzu,” “painful itch,” “chikuchiku,” “tickling itch” (AD > urticaria), and “itch like mosquito bites” (AD < urticaria). Thus, the expressions describing itch sensations selected in AD and urticaria patients are different, raising the possibility that differences in itch quality are classified by the terminology used to describe it.
Huet et al. indicated that in a web study of 170 patients with AD aged ≥14 years, burning itch and stinging (about 60% each) were the most common symptoms associated with pruritis, suggesting a neuropathic component [6]. Similarly, our present study shows that almost half of the AD patients experienced “painful itch,” which was significantly more frequent than urticaria patients. Furthermore, this type of itch sensation would make patients happiest if improved. Our results are consistent with recent studies demonstrating that pain in AD patients is a major component of the disease burden [9].
The most frequently selected “muzumuzu” itch feels like crawling skin. Huet et al. reported that crawling skin was a minor type in itch, ranking fifth out of eight major types of itch in French patients with AD [6]. However, previous Japanese studies on the quality of the itch experienced in AD [10] and urticaria [11] revealed that patients with these conditions describe the itch using more expressions related to crawling skin than expressions related to painful itch such as “chikuchiku,” “piripiri,” “burning,” and “stinging.” This finding is consistent with our results. Yosipovitch et al. also reported that crawling skin was most common in patients with AD of Chinese descent living in Singapore, followed by tickling, which was more common than burning itch or stinging [5]. Since these reports and our study did not assess the same itch descriptions, direct comparisons are difficult. However, itch sensations expressed with “muzumuzu” itch and crawling skin may be more specific to Asians.
The body area where AD patients most often experienced intense itch was the hands. In AD, hand eczema is intractable and may trigger severe itch, and consideration of this data is important for therapeutic intervention. Regarding the season and the time of day, half of the patients with AD and urticaria felt intense itch in the evening, at bedtime, and at night. In AD patients, “muzumuzu” was often felt on the arms, elbows, hands, head, neck, and back, in spring and autumn, in the evening, at bedtime, and at night. However, a “painful itch” was often felt on the hands, legs, and knees during the day in summer and winter.
The type of itch that would make patients happiest if improved was different between the diseases. “Painful itch” and “muzumuzu” accounted for about 30% and 20%, respectively, of AD patients. In contrast, “muzumuzu,” “itch like mosquito bites,” and “painful itch” were each reported by 20% of urticaria patients. Thus, the types of itch that patients hope to improve varied from patient to patient. Therefore, treatment satisfaction would be improved by paying attention to the kind of itch each patient hopes to improve.
Notably, 55% of patients with AD and 41% of patients with urticaria answered that they sometimes felt itch even after skin symptoms had subsided. The higher the itch severity, the higher the percentage of patients who felt itch. In both diseases, “muzumuzu” was the most suitable expression for describing the itch felt even after disappearance of skin symptoms. Whether differences in the pruritogen affect the quality of the itch sensation is an interesting question, but direct evidence remains lacking. Hence, the type (s) of pruritogens that induce the “muzumuzu” feeling remain unclear. We found that “muzumuzu” was predominantly selected by patients with both histaminergic (urticaria) and nonhistaminergic (atopic dermatitis) diseases, indicating that multiple factors can induce this sensation. Thus, “muzumuzu” is a type of itch independent of skin inflammation and might be associated with neural sensitization [12]. Peripheral sensitization is caused by cytokines or the deactivation of an inhibitory system for mechanical itch [13–16], and central sensitization is mediated by spinal glial cells activation, neuroinflammation, and cytokine production to maintain central sensitization, leading to chronic itch [17]. As remnant itch can lead to a relapse of skin rash due to scratching, treatment for itch is important after skin symptoms subside. Because “muzumuzu” tends to persist, it would be helpful to continue treatment in patients who continue to have this feeling.
Nevertheless, while “muzumuzu” was the most predominantly selected expression among both patient groups, the other expressions selected differed between respondents with these pruritic skin diseases. “Painful itch” and “chikuchiku” were prominent choices in the AD group. Conversely, “itch like mosquito bites” was deemed more characteristic of urticaria, indicating that this particular sensation may be specific to histaminergic itch. Furthermore, the second most predominant itch descriptions felt after skin symptoms had subsided also differed between these pruritic skin diseases. Therefore, we believe that different pruritogens affect the quality of the itch sensation, as reflected by the expressions selected to describe it.
The emergence of many new drugs for AD has made it possible to treat itch more effectively. To select treatment for each patient, it may be worth focusing on itch expressions patients use and the treatment responsiveness of these patients. Establishing effective treatments in the future for each itch type will enable treatments more suitable for each patient.
The major limitation of this study was the use of an online questionnaire survey that could not accurately capture the diagnosis and disease severity or contrast expressions describing itch with feelings related to skin lesions. We collected the itch terms that patients have experienced to try to gain a comprehensive understanding. However, the terms to describe itch in pediatric patients aged ≤15 years were fewer than in the other age groups. This may be because describing their sensations is difficult, in addition to having fewer itch experiences.
In conclusion, while various itch characterizations have been made around the world, this online questionnaire survey revealed the characteristics of itch in Japanese patients with AD or urticaria. Although a further study is needed on the simultaneous evaluation of symptoms and itch expression, on the evaluation of treatment responsiveness based on itch expression, these findings may lead to a better understanding of itch symptoms and improved treatment outcomes.
Statements
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
Institutional review board approval was not required because the study used completely anonymized data of the study patients and did not involve direct patient contact. However, voluntary informed consent was obtained from all study participants.
Author contributions
All authors contributed conception and design of study, analysis and interpretation of data, and revising and finalization of the manuscript. TA, TE, YOhs, YOhy, MT, and HM acquired data and drafted the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to thank Hideya Uratsuji PhD, of Maruho Co., Ltd., for the study design and implementation, Tomomi Ohara MS, of Maruho Co., Ltd., for helping data analysis, and Takahiko Murata PhD, of WysiWyg Co. Ltd., for medical writing assistance.
Conflict of interest
NI, SKo, MS-H, YF, and MF have received honoraria for lecture from Maruho. TA has received a research grant from Japan Society for the Promotion of Science and honoraria from Maruho and Santen Pharmaceutical. KI has received a research grant for his institution and honoraria from Maruho. YI has received research grants for his institution from Maruho, Sato Pharmaceutical, Torii Pharmaceutical, Taiho Pharmaceutical, Otsuka Pharmaceutical, Eisai, Kaken Pharmaceutical, Mitsubishi Tanabe Pharma, Eli Lilly Japan, Kyowa Kirin, Shiseido Japan, Boehringer Ingelheim, UCB Japan, Sanofi, and Janssen Pharmaceutical, a scholarship grant from Maruho, and honoraria from Maruho, Daiichi Sankyo, AbbVie, Eli Lilly Japan, Sanofi, Pfizer Japan, Mitsubishi Tanabe Pharma, Torii Pharmaceutical, Kaken Pharmaceutical, Otsuka Pharmaceutical, Pierre Fabre Dermo-Cosmé tique Japon, Sun Pharma Japan, Leo pharma Japan, Taiho Pharmaceutical, Sumitomo Pharma, Toray Industries, Japanese Society of Allergology, and KYORIN Pharmaceutical. HI has received research grants for his institution from Maruho, Otsuka Pharmaceutical, and Torii Pharmaceutical. TE has received honoraria from Maruho, Sanofi, and Otsuka Pharmaceutical. YOhs has received a scholarship grant and an advisory fee from Maruho, and honoraria from Maruho, KYORIN Pharmaceutical, and Torii Pharmaceutical. YOhy has received a research grant for his institution, a scholarship grant, a consulting fee, and honoraria from Maruho. TO have collaboration contracts with Maruho and Torii Pharmaceutical and has received honoraria from Maruho, Mitsubishi Tanabe Pharma, and Torii Pharmaceutical. YK has received research grants for her institution from Maruho, Eli Lilly Japan, Sanofi, AbbVie, Pfizer Japan, Otsuka Pharmaceutical, Leo Pharma Japan, Taiho Pharmaceutical, and Amgen and honoraria from Maruho, Sanofi, AbbVie, and Pfizer Japan. SKa has received a research grant for his institution from Maruho and honoraria from Maruho, Eli Lilly Japan, and AbbVie. HK has received a research grant for his institution, a scholarship grant, and honoraria from Maruho. MT has received a scholarship grant and honoraria for lecture from Maruho. TN has received a research grant for his institution from Maruho and honoraria from Maruho, Sanofi, Eli Lilly Japan, and AbbVie. MN has received research grants for her institution from Maruho and Sanofi, honoraria for lectures from Maruho, Torii Pharmaceutical, Sanofi, AbbVie, KYORIN Pharmaceutical, Sumitomo Pharma, Miyarisan Pharmaceutical, Meiji Seika Pharma, Otsuka Pharmaceutical, CSL Behring, and Novartis Pharma, and payment for expert testimony from Sanofi. SH has received honoraria from Maruho, Torii Pharmaceutical, and AbbVie. HM has received a research grant for his institution and an advisory fee from Maruho and honoraria from Maruho, Sanofi, AbbVie, Pfizer Japan, Mitsubishi Tanabe Pharma, Taiho Pharmaceutical, KYORIN Pharmaceutical, Eli Lilly Japan, and Otsuka Pharmaceutical.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The authors declare that this study received funding from Maruho Co., Ltd. The funder had the following involvement with the study: funding the Atopic Itch Consensus Meeting, the study design, implementation, data analysis of the web questionnaire survey, and the manuscript preparation.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontierspartnerships.org/articles/10.3389/jcia.2024.12578/full#supplementary-material
Abbreviations
AD, atopic dermatitis; NRS, numerical rating scale.
References
1.
Silverberg JI Gelfand JM Margolis DJ Boguniewicz M Fonacier L Grayson MH et al Patient burden and quality of life in atopic dermatitis in US adults: a population-based cross-sectional study. Ann Allergy Asthma Immunol (2018) 121(3):340–7. 10.1016/j.anai.2018.07.006
2.
Xu X van Galen LS Koh MJA Bajpai R Thng S Yew YW et al Factors influencing quality of life in children with atopic dermatitis and their caregivers: a cross-sectional study. Sci Rep (2019) 9(1):15990. 10.1038/s41598-019-51129-5
3.
Chovatiya R Lei D Ahmed A Chavda R Gabriel S Silverberg JI . Clinical phenotyping of atopic dermatitis using combined itch and lesional severity: a prospective observational study. Ann Allergy Asthma Immunol (2021) 127(1):83–90.e2. 10.1016/j.anai.2021.03.019
4.
Darsow U Scharein E Simon D Walter G Bromm B Ring J . New aspects of itch pathophysiology: component analysis of atopic itch using the 'Eppendorf Itch Questionnaire. Int Arch Allergy Immunol (2001) 124(1-3):326–31. 10.1159/000053748
5.
Yosipovitch G Goon AT Wee J Chan YH Zucker I Goh CL . Itch characteristics in Chinese patients with atopic dermatitis using a new questionnaire for the assessment of pruritus. Int J Dermatol (2002) 41(4):212–6. 10.1046/j.1365-4362.2002.01460.x
6.
Huet F Faffa MS Poizeau F Merhand S Misery L Brenaut E . Characteristics of pruritus in relation to self-assessed severity of atopic dermatitis. Acta Derm Venereol (2019) 99(3):279–83. 10.2340/00015555-3053
7.
Brenaut E Garlantezec R Talour K Misery L . Itch characteristics in five dermatoses: non-atopic eczema, atopic dermatitis, urticaria, psoriasis and scabies. Acta Derm Venereol (2013) 93(5):573–4. 10.2340/00015555-1599
8.
Kim-Dufor DH Poulaliou A Misery L . The need for linguistically and culturally adapted standard questionnaires to assess itch: a preliminary study. Acta Derm Venereol (2017) 97(8):991–2. 10.2340/00015555-2693
9.
Vakharia PP Chopra R Sacotte R Patel KR Singam V Patel N et al Burden of skin pain in atopic dermatitis. Ann Allergy Asthma Immunol (2017) 119(6):548–52. 10.1016/j.anai.2017.09.076
10.
Aoki T Okada S . Itch in atopic dermatitis and renal insufficiency. In: Archives of the 11th International Symposium on itch (2001). p. 38–40.
11.
Hide M . Itch of urticaria. Jpn J Dermatol (2005) 115(14):2357–62. (in Japanese).
12.
Yosipovitch G Berger T Fassett MS . Neuroimmune interactions in chronic itch of atopic dermatitis. J Eur Acad Dermatol Venereol (2020) 34(2):239–50. 10.1111/jdv.15973
13.
Feng J Luo J Yang P Du J Kim BS Hu H . Piezo2 channel-Merkel cell signaling modulates the conversion of touch to itch. Science (2018) 360(6388):530–3. 10.1126/science.aar5703
14.
Trier AM Mack MR Fredman A Tamari M Ver Heul AM Zhao Y et al IL-33 signaling in sensory neurons promotes dry skin itch. J Allergy Clin Immunol (2022) 149(4):1473–80.e6. 10.1016/j.jaci.2021.09.014
15.
Komiya E Tominaga M Hatano R Kamikubo Y Toyama S Sakairi H et al Peripheral endomorphins drive mechanical alloknesis under the enzymatic control of CD26/DPPIV. J Allergy Clin Immunol (2022) 149(3):1085–96. 10.1016/j.jaci.2021.08.003
16.
Miron Y Miller PE Hughes C Indersmitten T Lerner EA Cevikbas F . Mechanistic insights into the antipruritic effects of lebrikizumab, an anti-IL-13 mAb. J Allergy Clin Immunol (2022) 150(3):690–700. 10.1016/j.jaci.2022.01.028
17.
Shiratori-Hayashi M Tsuda M . Spinal glial cells in itch modulation. Pharmacol Res Perspect (2021) 9(6):e00754. 10.1002/prp2.754
Summary
Keywords
verbal expressions, itch, atopic dermatitis, urticaria, questionnaire survey
Citation
Ohya Y, Ebata T, Ohshima Y, Andoh T, Tominaga M, Kataoka Y, Fukui Y, Ebihara N, Hasegawa S, Kobayashi S, Morisawa Y, Inoue N, Narita M, Kaneko S, Igawa K, Nakahara T, Ishiuji Y, Okada T, Fujii M, Kawasaki H, Irie H, Shiratori-Hayashi M and Murota H (2024) Verbal expressions describing itch quality in atopic dermatitis and urticaria: an online questionnaire survey in Japan. J. Cutan. Immunol. Allergy 7:12578. doi: 10.3389/jcia.2024.12578
Received
18 December 2023
Accepted
03 April 2024
Published
15 April 2024
Volume
7 - 2024
Updates
Copyright
© 2024 Ohya, Ebata, Ohshima, Andoh, Tominaga, Kataoka, Fukui, Ebihara, Hasegawa, Kobayashi, Morisawa, Inoue, Narita, Kaneko, Igawa, Nakahara, Ishiuji, Okada, Fujii, Kawasaki, Irie, Shiratori-Hayashi and Murota.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hiroyuki Murota, h-murota@nagasaki-u.ac.jp
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.