- 1Department of Dermatology, Osaka University Graduate School of Medicine, Osaka, Japan
- 2Osaka Habikino Medical Center, Osaka, Japan
Dear Editors,
A 53-year-old female patient developed erythema and pruritus on her palms and arms a month before visiting our hospital. Subsequently, she received antiallergic medications and topical steroids; however, her condition did not improve. Erythema with ulceration was observed on her right arm, erythema with crusting on the posterior nail fold, and an inverted Gottron’s sign on her palms (Figures 1A–C). Owing to the concurrent emergence of muscular symptoms, she was referred to our hospital for further evaluation for dermatomyositis. The diagnosis of dermatomyositis positive for melanoma differentiation antigen 5 (MDA5) antibody was confirmed by the observation of high anti-MDA5 antibody levels (3,400; normal < 32). Computed tomography (CT) revealed the absence of active pneumonia. However, elevated C-reactive protein (CRP) (3.03 mg/dL) and ferritin (705 ng/mL) levels were regarded as risk factors for a poor prognosis. The histopathologic findings were consistent with dermatomyositis, with epidermal thinning, fluid degeneration, and cellular infiltration of the upper dermis. The T-SPOT test was negative.
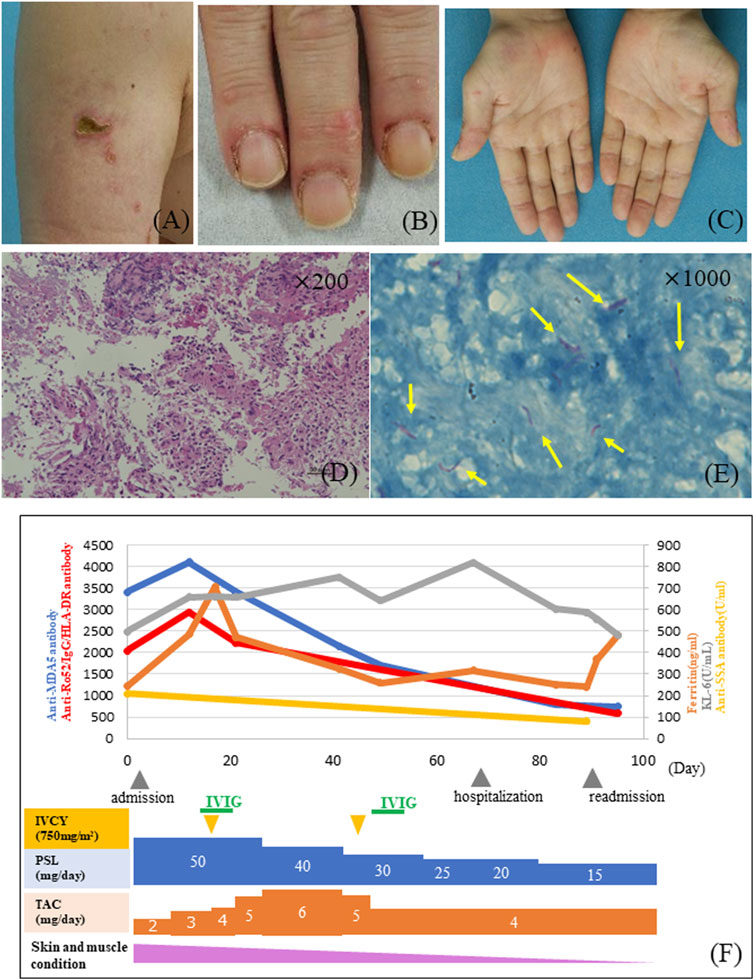
FIGURE 1. (A) Erythema with ulceration on the right upper arm at the time of the initial visit to our clinic. (B) Erythema on the posterior nail fold. (C) Gottron’s sign on the palms. (D) The histopathological analysis revealed the presence of epithelial and Langhans giant cells within the dermal layers of the subcutaneous mass (HE × 200). (E) Scattered reddish bacilli (Ziehl-Neelsen × 1,000). (F) The therapeutic regimen involved the administration of prednisolone (PSL) 50 mg (1 mg/kg/day), tacrolimus (TAC) with a targeted trough range of 10–15 ng/mL, and intravenous pulse cyclophosphamide (IVCY) at a dosage of 750 mg/m2 × 2. During the course of the study, the patient also underwent intravenous immunoglobulin (IVIG) therapy twice. Following a month’s treatment, an elevation in CRP levels to 10.69 mg/dL was observed, alongside a trend of decreasing anti-Ro52/IgG/HLA-DR complex antibody titers. Coexisting diagnoses encompassed pulmonary tuberculosis and scrofuloderma in this patient.
The patient received prednisolone (PSL) at a dose of 50 mg (1 mg/kg/day), tacrolimus (TAC) maintained at trough levels of 10–15 ng/mL, and intravenous pulse cyclophosphamide (IVCY) at 750 mg/m2. After the first IVCY, the anti-MDA5 antibody titer was high, suggesting that the disease was still present. Therefore, IVCY was administered twice. One month later, the CRP level (10.69 mg/dL) was elevated, accompanied by fever and muscle pain in the extremities, but the anti-MDA5 antibody level (800) was not elevated. Furthermore, the anti-Ro52/IgG/HLA-DR complex antibody titer was measured as previously described [1], longitudinally from admission, and exhibited a consistent downward trend (Figure 1F). The CT images displayed areas of ground-glass opacities and nodular shadows. Concurrently, a painless subcutaneous mass appeared in the head and neck region, prompting a biopsy. The histopathological analysis revealed the presence of epithelial and Langhans giant cells within the dermal layers (Figures 1D, E). Red bacilli were visible on Ziehl-Neelsen staining. Culture and PCR analyses of both the sputum and subcutaneous masses confirmed the presence of Mycobacterium tuberculosis. These results led to a diagnosis of pulmonary tuberculosis and cutaneous adenopathy. Tuberculosis improved after treatment with a combination of four drugs: isoniazid, rifabutin, levofloxacin, and pyrazinamide. Thereafter, the fever resolved, the cervical mass shrank, and the muscle pain in the extremities improved.
In this case, enlargement of the cervical lymph nodes suggested that the tuberculosis bacilli had lymphatically spread from the lungs to the skin. Extrapulmonary tuberculosis is more likely to occur when cellular immunity is inadequate [2], and this complication should be noted when many immunosuppressive agents are administered.
In cases of anti-MDA5 antibody-positive dermatomyositis, it has been established that the anti-MDA5 antibody titer, KL-6 levels, ferritin levels, and CRP levels are recognized to exhibit a correlation with the disease severity [3, 4]. More recently, several findings have emerged regarding the relationship between anti-SSA/Ro52 antibodies, with reports of significantly higher mortality in patients with double-positive anti-MDA5 and anti-Ro52 antibodies [5]. This case was double positive for anti-MDA5 and anti-SSA/Ro52 antibodies and elevated ferritin levels (max 701), which may be a poor prognosis group and require strong immunosuppressive treatment. For these patients with poor prognoses, the use of immunosuppressive drugs is necessary, but care should be taken to avoid the development of infections.
Furthermore, we previously found that changes in anti-Ro52/IgG/HLA-DR complex antibody titers were correlated with the severity of myositis, including interstitial lung disease, in anti-MDA5 antibody-positive patients [1]. In this case, the anti-Ro52/IgG/HLA-DR complex antibody titer, which was high on admission, decreased at the onset of tuberculosis, indicating that measurement of the anti-Ro52/IgG/HLA-DR complex antibody titer is also useful in differentiating interstitial pneumonia caused by dermatomyositis from an infection that occurs during its treatment.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Prof. Yoshitaka Isaka/Nephrology. The studies were conducted in accordance with the local legislation and institutional requirements. The human samples used in this study were acquired from a by-product of routine care or industry. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
NA conducted the experiments, YH, KT, NA, and IU-H wrote the manuscript, and YH, KT, CY, YI, IU-H, AT, YKi, YKa, and MF involved in the medical treatment. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Arase, N, Tsuji, H, Takamatsu, H, Jin, H, Konaka, H, Hamaguchi, Y, et al. Cell surface-expressed Ro52/IgG/HLA-DR complex is targeted by autoantibodies in patients with inflammatory myopathies. J Autoimmun (2022) 126:102774. doi:10.1016/j.jaut.2021.102774
2. Caccamo, N, Guggino, G, Joosten, SA, Gelsomino, G, Di Carlo, PD, Titone, L, et al. Multifunctional CD4(+) T cells correlate with active Mycobacterium tuberculosis infection. Eur J Immunol (2010) 40:2211–20. doi:10.1002/eji.201040455
3. Sato, S, Masui, K, Nishina, N, Kawaguchi, Y, Kawakami, A, Tamura, M, et al. Initial predictors of poor survival in myositis-associated interstitial lung disease: a multicentre cohort of 497 patients. Rheumatology (Oxford) (2018) 57:1212–21. doi:10.1093/rheumatology/key060
4. Nishioka, A, Tsunoda, S, Abe, T, Yoshikawa, T, Takata, M, Kitano, M, et al. Serum neopterin as well as ferritin, soluble interleukin-2 receptor, KL-6 and anti-MDA5 antibody titer provide markers of the response to therapy in patients with interstitial lung disease complicating anti-MDA5 antibody-positive dermatomyositis. Mod Rheumatol (2019) 29:814–20. doi:10.1080/14397595.2018.1548918
Keywords: anti-MDA5, dermatomyositis, Ro52/IgG/HLA-DR, interstitial pneumonia, tuberculosis
Citation: Hatano Y, Tonomura K, Yamashita C, Arase N, Ishitsuka Y, Ueda-Hayakawa I, Tanemura A, Kimura Y, Kataoka Y and Fujimoto M (2024) A case of anti-melanoma differentiation antigen 5 antibody-positive dermatomyositis in which monitoring of Ro52/IgG/HLA-DR complex antibody titer was useful to exclude interstitial pneumonia. J. Cutan. Immunol. Allergy 7:12630. doi: 10.3389/jcia.2024.12630
Received: 28 December 2023; Accepted: 25 January 2024;
Published: 06 February 2024.
Copyright © 2024 Hatano, Tonomura, Yamashita, Arase, Ishitsuka, Ueda-Hayakawa, Tanemura, Kimura, Kataoka and Fujimoto. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kyoko Tonomura, a3lva290b25vbXVyYTA1MzBAZ21haWwuY29t
 Yoko Hatano1
Yoko Hatano1 Kyoko Tonomura
Kyoko Tonomura Yoko Kataoka
Yoko Kataoka Manabu Fujimoto
Manabu Fujimoto