Dear Editors,Urticaria is a mast cell-driven disorder characterized by the development and resolution of itchy wheals within a short period of time (usually 24 h). In cases where the wheals last longer than 24 h, they must be differentiated from other diseases, including urticarial vasculitis [1] and neutrophilic urticarial dermatosis [2]. However, some patients may present with persistent urticarial eruptions in the absence of vasculitis and neutrophilic infiltration of the lesions. Herein, we report a case of prolonged urticaria associated with eosinophilic infiltrates, that was effectively treated with dapsone.
A 55-year-old Japanese woman presented with a 2-year history of recurrent wheals on the trunk and extremities. The itchy, non-burning wheals showed a centrifugal pattern of expansion with slight residual pigmentation in the center. They disappeared during a few days, up to 7 days (Figures 1A–D). No associated systemic symptoms, hematological disorders, or medication use were observed. Laboratory investigations revealed normal peripheral eosinophil counts (98.4/µL), and elevated levels of serum IgE (274.0 IU/mL) and thyroid peroxidase antibodies (20.8 IU/mL), without detection of antinuclear antibodies, anti-BP180 antibodies or myeloperoxidase-anti-neutrophil cytoplasmic antibodies. Pressure-challenge testing failed to elicit wheals at the pressure site. A skin biopsy specimen showed perivascular and interstitial infiltration of lymphocytes and eosinophils throughout the dermis with prominent eosinophilic degranulation (Figures 1E, F). No significant vascular damages, and neutrophilic infiltration were observed. Antihistamine and antileukotriene had some effects yet with the persistence of long-lasting wheals. The addition of dapsone successfully and completely resolved the wheals.
FIGURE 1
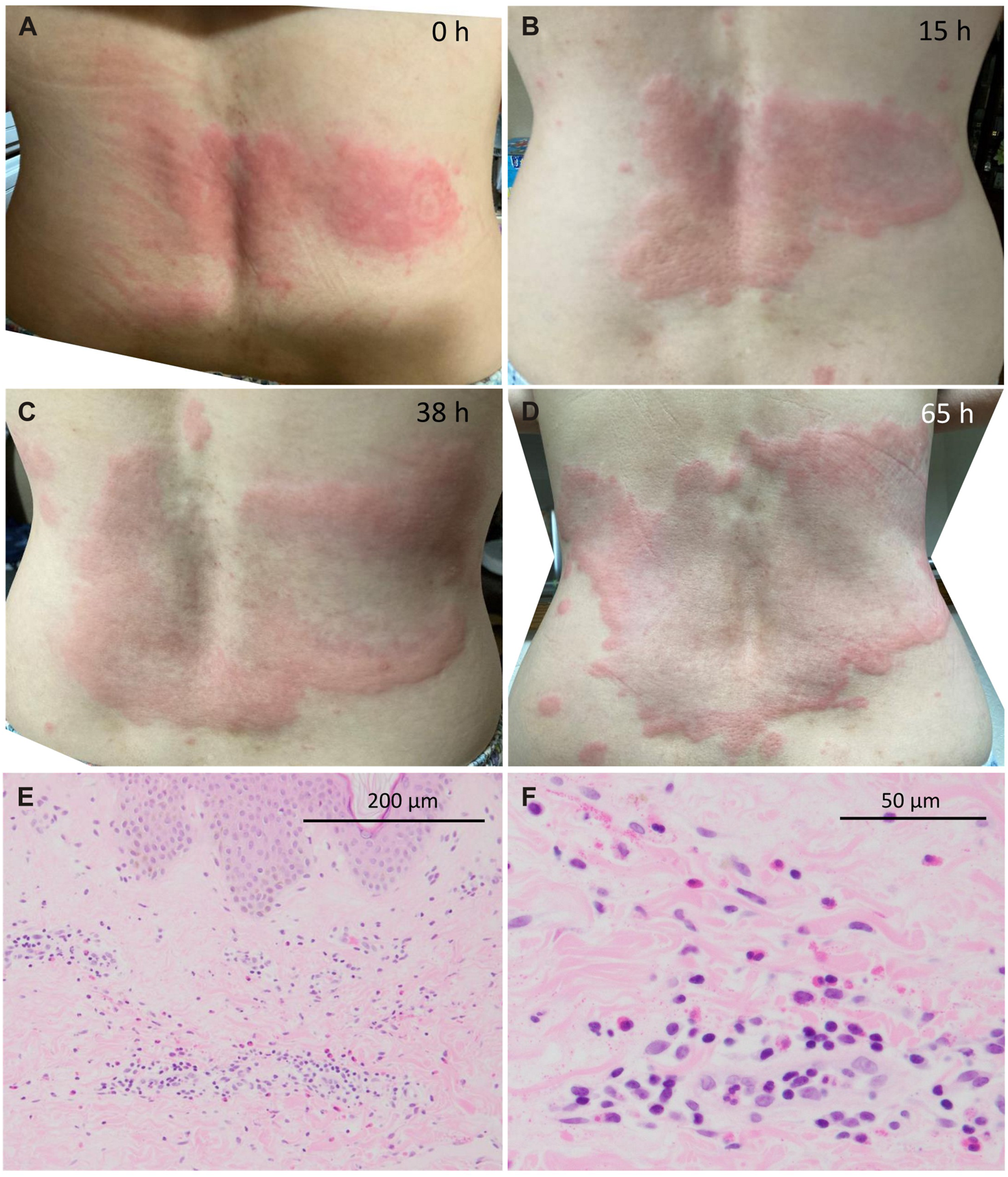
Clinical and histological findings. (A–D) A itchy, non-burning wheal on the lumbar region. The wheal expanded in a centrifugal patter with mild residual pigmentation in the center, and disappeared in 7 days. (E) A histological section of the skin lesion shows that lymphocytes and eosinophils have infiltrated in the perivascular and interstitial regions throughout the dermis. None of vacuolar alteration, mucin deposition, melanin incontinence, and basal melanosis are observed. The skin sample was obtained from the edematous and erythematous part of a wheal approximately 9 h after the appearance. (F) The infiltrated eosinophils are prominently degranulated in the absence of significant neutrophilic infiltration, endothelial swelling, nuclear dusts, and erythrocyte extravasation.
The present case of prolonged urticaria needed to be distinguished from conditions in which wheals persist for more than 24 h. Delayed pressure urticaria may last up to 72 h with eosinophilic infiltration, but is induced at pressure sites. Urticarial vasculitis shows urticarial eruptions with pain and purpura that causes pigmentation upon resolution [1]. Histological features include varying degrees of vascular damage with an angiocentric inflammatory infiltrate of lymphocytes and neutrophils. In neutrophilic urticarial dermatosis, neutrophils densely infiltrate perivascular and interstitial regions [2]. These two conditions are distinct from our case based on the clinical and/or histological findings. Lastly, eosinophilic annular erythema (EAE), a subtype of Wells syndrome, is characterized by annular edematous erythema [3], which shares clinical features and histopathological findings of eosinophilic infiltrates with the present case. However, EAE lesions generally disappear in several weeks to several months [3], and histologically show vacuolar alteration, mucin deposition, melanin incontinence, or basal melanosis in addition to eosinophilic infiltration [4]. Based on the presence of recurrent wheals within a week and the absence of such histological findings in our case, EAE was excluded. Therefore, the present case was considered a persistent type of urticaria.
The predominant histological findings of eosinophilic degranulation and the good response to dapsone suggest that lesional eosinophils contributed to the formation of long-lasting wheals in our case. Dapson effectively suppresses eosinophil function by inhibiting eosinophil peroxidase. In chronic spontaneous urticaria, eosinophils are reportedly present in perivascular cellular infiltrates of the lesional skin, where eosinophils interact with mast cells via secretion of various cytokines including IL-5, eotaxin, stem cell factor, etc [5]. However, an association of lesional eosinophils with wheal prolongation has not been described. Our case suggests that prolonged urticaria may develop in association with lesional eosinophilic infiltrates, and respond well to dapsone.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was not required for the studies involving humans because the manuscript is a case report that contains no identifiable information. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
This study was supported by the Japan Science and Technology Agency (JST) CREST (JPMJCR2111).
Conflict of interest
ST has received research grant and honorarium from Tanabe-Mitsubishi.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Marzano AV Maronese CA Genovese G Ferrucci S Moltrasio C Asero R et al Urticarial vasculitis: clinical and laboratory findings with a particular emphasis on differential diagnosis. J Allergy Clin Immunol (2022) 149(4):1137–49. 10.1016/j.jaci.2022.02.007
2.
Gusdorf L Lipsker D . Neutrophilic urticarial dermatosis: an entity bridging monogenic and polygenic autoinflammatory disorders, and beyond. J Eur Acad Dermatol Venereol (2020) 34(4):685–90. 10.1111/jdv.15984
3.
Ikutama R Ogawa T Takeno K Ikeda S . A case of eosinophilic annular erythema (EAE) concomitant with autoimmune hypothyroidism. Indian Dermatol Online J (2023) 14(6):882–3. 10.4103/idoj.idoj_558_22
4.
Nakazato S Fujita Y Shinkuma S Nomura T Shimizu H . Eosinophilic annular erythema is clinically characterized by central pigmentation reflecting basal melanosis: a clinicopathological study of 10 cases. J Eur Acad Dermatol Venereol (2017) 31(11):1916–23. 10.1111/jdv.14350
5.
Giménez-Arnau AM DeMontojoye L Asero R Cugno M Kulthanan K Yanase Y et al The pathogenesis of chronic spontaneous urticaria: the role of infiltrating cells. J Allergy Clin Immunol Pract (2021) 9(6):2195–208. 10.1016/j.jaip.2021.03.033
Summary
Keywords
urticaria, eosinophil, neutrophil, vasculitis, dapsone
Citation
Munemori M and Takahagi S (2024) A case of prolonged urticaria associated with lesional eosinophilic infiltrates. J. Cutan. Immunol. Allergy 7:12675. doi: 10.3389/jcia.2024.12675
Received
10 January 2024
Accepted
21 February 2024
Published
29 February 2024
Volume
7 - 2024
Updates
Copyright
© 2024 Munemori and Takahagi.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shunsuke Takahagi, shunstk@hiroshima-u.ac.jp
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.