Dear Editors,
This report describes a case of cold urticaria with positive results of cold stimulation test (CST) only on the lower legs.
A 16-year-old woman with no family history noticed wheals with itch appearing on the skin exposed to cold, such as wind from a fan and airflow when riding a bicycle 6 months ago. Initially, the lesions appeared mainly on the face and forearms and slightly on the lower legs; however, 3 months ago, they appeared mostly on the lower legs. After the diagnosis of cold urticaria (CU) was made, bilastine (20 mg/day) and syo-seiryu-to, a Chinese herbal medicine, (2.6 g/day) were administered. Wheals repeatedly appeared despite these drugs and the patient was referred to our hospital.
Multiple wheals with itch, which were various-sized and mainly punctate wheals, were observed on the left lower leg at the first visit (Figure 1A). Laboratory data showed an increased level of IgE (1,470 IU/mL; normal, <173 IU/mL), positive anti-SSA/Ro antibodies (titer: 25.6; normal, <10), positive antinuclear antibodies (ANA) (titer: 160; normal, <40), and positive cold agglutinin (CA) (titer: 256; normal, <256), but negative for cryoglobulin and anti-mycoplasma antibodies. Serum levels of IgE (1,470 IU/mL; normal, <173) and IgM (225 mg/dL; normal 35–220) were elevated, but those of IgG (1,508 mg/dL; normal, 870–1700) and IgA (144 mg/dL; normal, 110–510) were within normal ranges. Other blood tests including hemoglobin concentration (13.5 g/dL; normal, 13.7–16.8), C-reactive protein (0.02 mg/dL; normal, <0.3) and the pattern of immunoelectrophoresis and urine tests revealed no abnormalities. As this patient showed neither anemia nor jaundice, autoimmune hemolytic anemia was neglected. After 5 months, the CA titer was reduced to 128, and the ANA titer was 80.
FIGURE 1
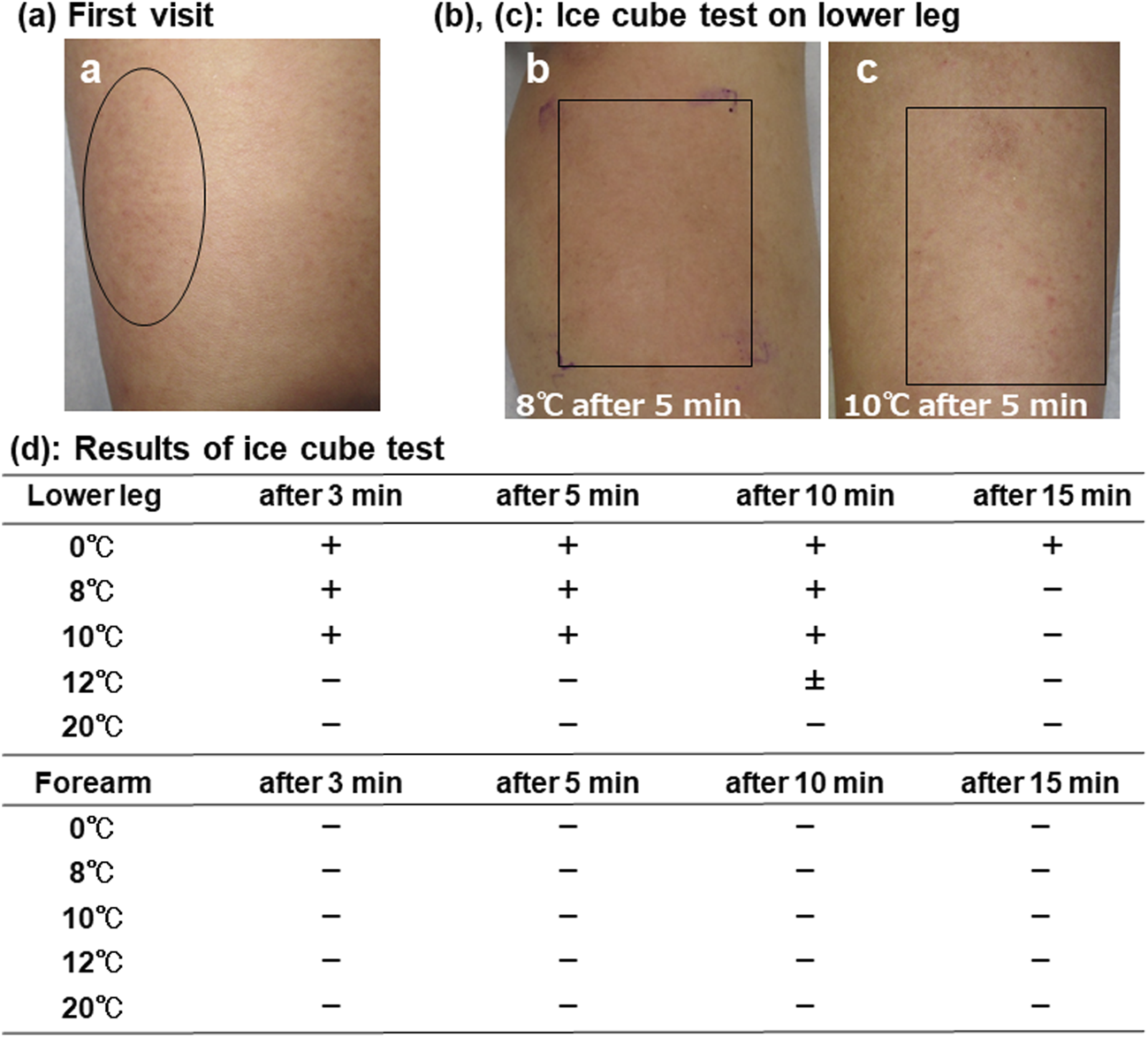
Clinical finding of the left lower leg at the first visit (A). Multiple wheals, mainly punctate wheals, were identified by a circle. The findings of left lower leg in ice cube test for 5 min at 8°C (B) and 10°C (C) after 5 min. There were multiple wheals, mainly punctate wheals, identified by squares. The results of ice cube test (D).
Oral medications were discontinued for 3 days before CST. CST was performed by putting ice water in a thin plastic bag (0°C) on the lower legs and forearms for 5 min. Consequently, wheals with itch appeared only on the lower legs, not on the forearms. To determine the trigger thresholds of wheal appearance, temperatures in plastic bags were changed to 8, 10, 12, and 20°C, respectively. The lower leg remained positive at 8°C (Figure 1B) and 10°C (Figure 1C), and slightly positive at 12°C, but not at 20°C.
Based on these observations, the patient was judged as having localized CU at 10°C–12°C with the borderline temperature to cause wheals (Figure 1D). In this patient, clinical symptoms and CST-induced eruptions were mainly punctate wheals. It is well known that punctate wheals often appear in systemic cold urticaria. However, both punctate and bigger wheals can be observed in localized cold urticaria. The patient avoided cold environments and resumed taking the medication, resulting in a significantly reduced incidence of wheal appearance after 3 months.
Localized CU occurs at the skin areas that are cooled [1]. CST is usually performed on the flexor sites of the forearms [1]. In this report, we describe a case of CU that first appeared on the face, forearms, and slightly on the lower legs, and then exclusively on the lower legs. A few cases with CU limited to the face [2], knee [3], or extremities [4] have been reported. In our case, the CST was positive on the lower legs, but not on the forearms. Although the mechanism by which wheals are not induced by cold exposure on the forearms is unknown, it might be involved in different skin sensitivities to cold exposure, such as desensitization by repeated cold stimulation. Our case initially showed wheals mainly on the face and forearms, but the forearm skin could no longer react to repeated cold stimulation, resulting in the absence of wheals.
It has been reported that CA and cryoglobulins may be associated with the course and possibly the pathogenesis in a subpopulation of CU [5]. In this case, CA was positive and cryoglobulin was negative at the first visit, and CA was negative after 5 months.
The symptoms of CU improved after 3 months. Thus, CA can be related to the pathogenesis of CU. However, as this patient avoided the cold exposure and resumed oral administration of bilastine and syo-seiryu-to for 5 months, it is difficult to evaluate the relationship between CA and the pathogenesis of CU. CU may be driven by other unidentified mechanisms.
In conclusion, because skin responsiveness to cold exposure might depend on the sites of the body, it is preferable to perform CST not only on the forearms but also on other sites of the body.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was not required for the studies involving humans because the manuscript is a single case report. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
MS and TF contributed to acquiring the data, and HH wrote the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Zuberbier T Abdul Latiff AH Abuzakouk M Aquilina S Asero R Baker D et al The international EAACI/GA2LEN/EuroGuiDerm/APAAACI guideline for the definition, classification, diagnosis, and management of urticaria. Allergy (2022) 77(3):734–66. 10.1111/all.15090
2.
Sciallis GF 2nd Krych EH . Localized cold urticaria to the face in a pediatric patient: a case report and literature review. Pediatr Dermatol (2010) 27(3):266–9. 10.1111/j.1525-1470.2010.01134.x
3.
Jagadevan M Mohanakrishnan B Balaji G Munisamy M Murugesan S . Report of a case of cold urticaria following cryotherapy - need for screening for untoward effects of cryotherapy in physical therapy clinical practice. J Orthop Case Rep (2021) 11(10):41–4. 10.13107/jocr.2021.v11.i10.2460
4.
Czarnetzki BM Frosch PJ Sprekeler R . Localized cold reflex urticaria. Br J Dermatol (1981) 104(1):83–7. 10.1111/j.1365-2133.1981.tb01716.x
5.
Bizjak M Košnik M Terhorst-Molawi D Dinevski D Maurer M . Cold agglutinins and cryoglobulins associate with clinical and laboratory parameters of cold urticaria. Front Immunol (2021) 12:665491. 10.3389/fimmu.2021.665491
Summary
Keywords
urticaria, cold urticaria, cold stimulation test, localized cold urticaria, cold agglutinin
Citation
Hachiken H, Furukawa T and Seishima M (2024) Localized cold urticaria with positive cold stimulation test only on lower legs. J. Cutan. Immunol. Allergy 7:12689. doi: 10.3389/jcia.2024.12689
Received
14 January 2024
Accepted
27 February 2024
Published
08 March 2024
Volume
7 - 2024
Updates
Copyright
© 2024 Hachiken, Furukawa and Seishima.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mariko Seishima, marikoseishima@yahoo.co.jp
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.