Abstract
Facial redness in atopic dermatitis (AD) is often intractable due to factors like chronic inflammation, steroid-induced telangiectasia, and rosacea-like dermatitis from topical treatments. Pulsed-dye laser (PDL) effectively treats both vascular and non-vascular inflammatory conditions, but its use in adult AD is limited. This study presents three cases of refractory AD with significant facial erythema treated with PDL. Two women and one man had undergone five to thirteen PDL treatments at 3 weeks to 3-month intervals. Clinical response was evaluated using the Eczema Severity Score, which showed significant improvement after PDL treatments. Our cases explore the efficacy of PDL in treating refractory facial erythema in adult AD patients. Patients tolerated the procedures well without severe complications such as hyperpigmentation, hypopigmentation, or blister formation. These findings suggest that PDL effectively reduces facial redness and alleviates associated AD symptoms. PDL is expected to address both vasodilation and cutaneous inflammation as an adjunctive therapy to manage refractory facial redness in adult AD. Further cases and research are needed to fully understand PDL’s immunomodulatory effects.
Introduction
Atopic dermatitis (AD) is a chronic inflammatory skin condition characterized by pruritus, eczema, and a range of other skin symptoms. Facial redness in AD is often intractable because clinical symptoms are affected by multiple factors, such as chronic inflammation, telangiectasia due to long-term steroid use, and rosacea-like dermatitis induced by topical steroids or calcineurin inhibitors. Pulsed-dye laser (PDL) effectively treats not only vascular lesions but also non-vascular inflammatory diseases, such as acne and psoriasis [1]. In the context of AD or eczema, PDL is only reported to be effective in pediatric cases [2, 3]. Its use in adult AD remains underexplored. We herein report three cases of AD refractory to topical treatments, in which PDL was effective for facial redness and associated symptoms.
Case description
Case 1
A 51-year-old Japanese woman had had a history of AD since childhood. She had intractable facial eczema and redness that did not respond well to topical steroids. Scaly erythema with telangiectasia was observed from the cheek to the neck (Figures 1A, B). Her face was treated with PDL (Vbeam Perfecta, Candela Corporation, Marlborough, MA, USA) at a fluence of 5 to 6 J/cm2, 1.5-ms pulse duration, and spot size of 12 mm, for a total of 5 treatments with 3-month intervals (Figure 1C). Her facial redness almost completely disappeared, but her neck erythema persisted, as this area was untreated. She also stopped using topical steroids because of marked improvement of AD symptoms in the area treated with PDL. She continued PDL treatment every 3 months for a year following recovery, and the patient experienced no recurrence for more than a year even after stopping having PDL.
FIGURE 1
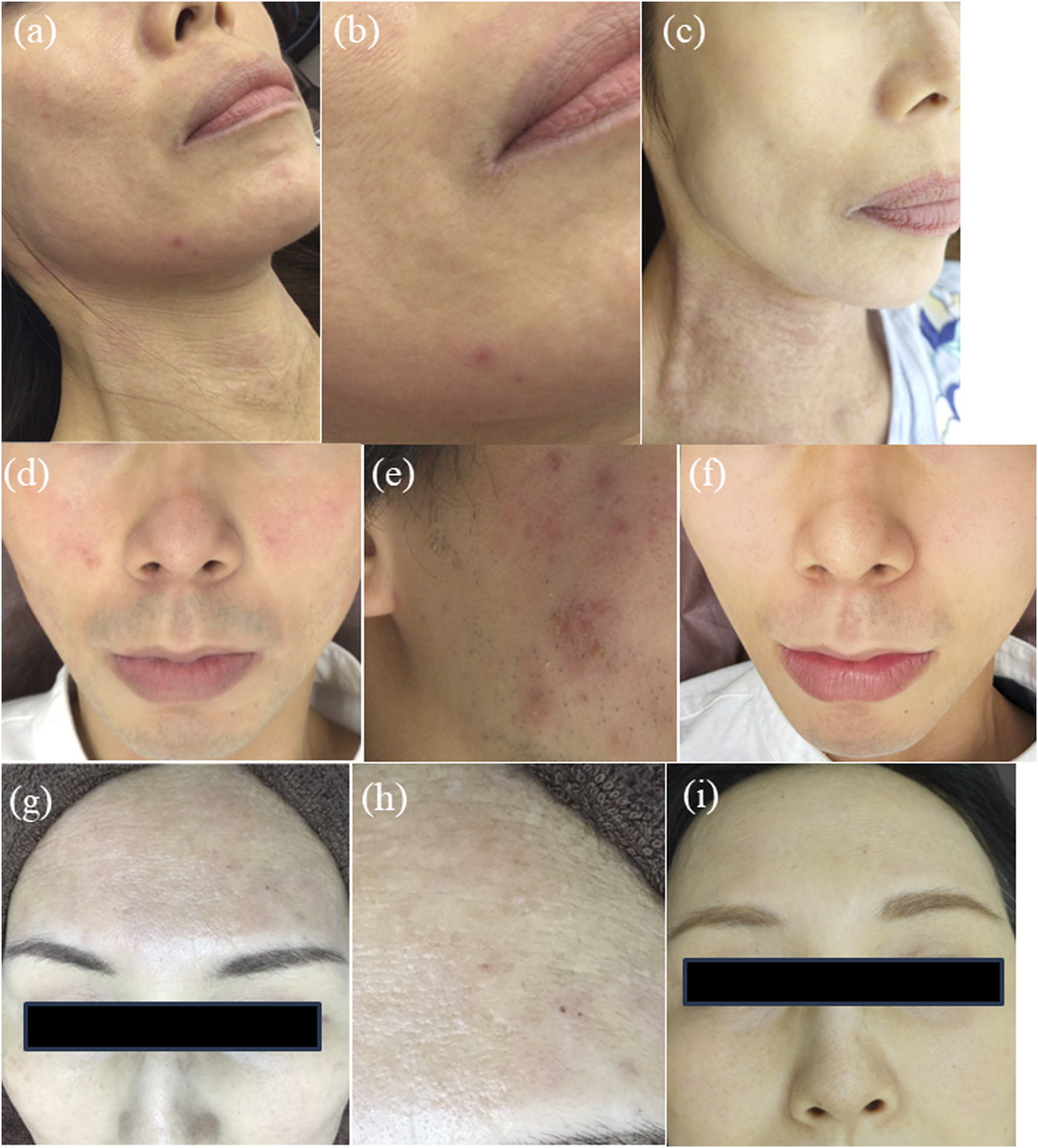
Clinical features of Case 1 (A–C), Case 2 (D–F) and Case 3 (G–I). (A) Scaly erythema with telangiectasia from her cheeks to neck. (B) A magnified image shows skin roughness and lichenification. (C) Facial redness and skin roughness were improved after five treatments of PDL although lichenification remained on the neck which was not treated with PDL. (D) Facial redness, acne breakouts, and post inflammatory erythema on both cheeks. (E) Erythema with excoriation and weeping on his right cheek (F) The skin lesions were almost cleared after 10 treatments of PDL. (G) Scaly erythema and telangiectasia on her forehead and both cheeks. (H) A magnified image shows skin roughness and excoriation. (I) The facial lesions were almost cleared after 13 treatments of PDL.
Case 2
A 30-year-old Japanese man with a long history of AD and acne presented with recurrent facial redness, excoriation, weeping itching, and acne breakouts (Figures 1D, E). His acne was settled with 5 months use of isotretinoin, but he continued to show residual facial redness and intermittent flares of itch. His face was treated with PDL at a fluence of 4.5 to 5 J/cm2, 1.5-ms pulse duration, and 10-mm spot size for a total of 10 treatments with a monthly interval (Figure 1F). After PDL treatment, his facial redness subsided, and episodes of facial itching were much less frequent after treatment. He has been treated with monthly PDL as maintenance therapy, and he has not shown exacerbation in facial redness or scaly erythema.
Case 3
A 57-year-old Japanese woman presented with prolonged facial redness and typical AD symptoms, such as itching and scaly erythema. Diffuse facial erythema was noted, with focal scaling and skin roughness (Figures 1G, H). She was started on topical ivermectin with PDL at a fluence of 4.5 5 J/cm2, 1.5-ms pulse duration, and spot size of 10–12 mm, for a total of 13 treatments at 3-week intervals (Figure 1I). Her facial erythema faded and flares of AD symptoms on the face became less frequent after treatment. Figure 1I shows the latest manifestation, and there has been no significant flare-up during the follow-up period.
All patients tolerated the PDL procedures without the need for topical anesthesia, and no severe complications such as hyperpigmentation, hypopigmentation, or blister formation were observed. Clinical response was evaluated using the Eczema Severity Score (ESS) by two dermatologists. The ESS, based on a modification of the Eczema Area and Severity Index (EASI), assesses six clinical signs (erythema, edema/induration/papulation, excoriations, oozing/weeping/crusting, scaling, and lichenification), each scored from 0 to 3, with a maximum score of 18. The localized ESS for facial symptoms significantly decreased after 5 to 10 PDL sessions: Case 1, 11/2; Case 2, 6/1; and Case 3, 8/3.
Discussion
Facial redness in AD is multifactorial, encompassing steroid-induced telangiectasia, rosacea-like dermatitis, contact dermatitis due to skin care products, and chronic inflammation due to AD itself. In our three cases, previous topical treatment improved itch and skin roughness but did not significantly reduce facial redness, suggesting the existence of underlying telangiectasia or rosacea. Multiple sessions of PDL almost cleared facial redness in the three cases, which is in line with the efficacy of PDL in treating facial redness induced by telangiectasia and rosacea [4, 5]. Unexpectedly, PDL also reduced the number of flares in AD symptoms, such as itching, scaling, and skin roughness, suggesting that PDL may normalize skin inflammation. PDL has been shown to be effective in inflammatory skin diseases, such as acne, localized plaque-type psoriasis, and nail psoriasis [1]. Sidewell et al. reported that PDL was effective in treating eczema overlying port-wine stain. A subsequent study showed that PDL was also effective in treating small areas of chronic localized eczema, mainly on the extremities, in children with AD. Considering the efficacy of PDL in acne, psoriasis, and eczema reported in previous literature, PDL is likely to show an anti-inflammatory effect in facial erythema associated with AD, together with its role in treating vascular dilation.
PDL emits light at 585 nm, primarily absorbed by oxygenated hemoglobin, leading to selective photothermolysis of capillaries and endothelial cells [6]. This process induces dermal connective tissue damage, edema formation, and subsequent release of cytokines and growth factors, promoting collagen production. Additionally, PDL irradiation leads to an increase in lymphocytes in the skin after 5 weeks [7]. PDL may have a potential immunological effect beyond photothermolysis. Ultraviolet light therapy is known as a treatment of psoriasis and atopic dermatitis due to its immunosuppressive effects [8], but it is currently unknown whether PDL exhibits similar effects. Further research is needed to fully understand PDL’s immunomodulatory effects.
Our cases suggest that PDL could be an effective therapy to control facial redness in adult AD in two ways: by suppressing vascular dilation and by soothing skin inflammation. In our cases, PDL was effective for managing both facial redness and other AD-related symptoms, such as itching, scaling, and skin roughness, suggesting that PDL could be an adjunct to control facial redness in AD that is resistant to topical therapies.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YK contributed to the design of the study, investigation, acquisition and analysis of data, and drafting of the manuscript. SN contributed to the conception and design of the study, acquisition and analysis of data and critical manuscript revision. S-iM critically revised the manuscript for important intellectual content. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Erceg A de Jong EM van de Kerkhof PC Seyger MM . The efficacy of pulsed dye laser treatment for inflammatory skin diseases: a systematic review. J Am Acad Dermatol (2013) 69:609–15. 10.1016/j.jaad.2013.03.029
2.
Syed S Weibel L Kennedy H Harper JI . A pilot study showing pulsed-dye laser treatment improves localized areas of chronic atopic dermatitis. Clin Exp Dermatol (2008) 33:243–8. 10.1111/j.1365-2230.2007.02644.x
3.
Sidwell RU Syed S Harper JI . Port-wine stains and eczema. Br J Dermatol (2001) 144:1269–70. 10.1046/j.1365-2133.2001.04250.x
4.
Tan SR Tope WD . Pulsed dye laser treatment of rosacea improves erythema, symptomatology, and quality of life. J Am Acad Dermatol (2004) 51:592–9. 10.1016/j.jaad.2004.04.010
5.
Bernstein EF Kligman A . Rosacea treatment using the new-generation, high-energy, 595 nm, long pulse-duration pulsed-dye laser. Lasers Surg Med (2008) 40:233–9. 10.1002/lsm.20621
6.
Anderson RR Parrish JA . Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science (1983) 220:524–7. 10.1126/science.6836297
7.
Omi T Kawana S Sato S Takezaki S Honda M Igarashi T et al Cutaneous immunological activation elicited by a low-fluence pulsed dye laser. Br J Dermatol (2005) 153:57–62. 10.1111/j.1365-2133.2005.06971.x
8.
Kemény L Varga E Novak Z . Advances in phototherapy for psoriasis and atopic dermatitis. Expert Rev Clin Immunol (2019) 15:1205–14. 10.1080/1744666x.2020.1672537
Summary
Keywords
atopic dermatitis, pulsed dye laser, laser, facial redness, telangiectasia
Citation
Kuriyama Y, Motegi S-i and Noda S (2024) Case report: Effectiveness of pulsed dye laser in facial redness of atopic dermatitis: a report of three cases. J. Cutan. Immunol. Allergy 7:13514. doi: 10.3389/jcia.2024.13514
Received
10 July 2024
Accepted
21 August 2024
Published
30 August 2024
Volume
7 - 2024
Updates
Copyright
© 2024 Kuriyama, Motegi and Noda.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuko Kuriyama, kuriyamayuko@gunma-u.ac.jp
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.