- Department of Dermatology, Kanazawa Medical School, Uchinada, Japan
Lichen nitidus is a chronic skin disease characterized by scattered shiny papules and is common among relatively young individuals. We report a persistent rash covering the body of a 6-year-old boy, unresponsive to prior treatments like moisturizers and topical steroids. Clinical examination revealed small yellow papules predominantly distributed on the trunk, around the eyes, and clustered around the elbow and knee fossa. Histopathological analysis showed a localized infiltrate of lymphocytes and basal epithelial cells, along with giant cells. The overlining rete ridges extended to surround the inflammatory cells, resembling a claw clutching a ball image. Topical treatment with alclometasone dipropionate ointment was more effective compared to maxacalcitol. Remarkably, after about 3 months of treatment, the rash had completely disappeared. We summarized treatments of lichen nitidus in Japan. Maxacalcitol had never been tried. In this report, we demonstrated the effectiveness of the steroid ointment compared to maxacalcitol through the clinical course.
Introduction
Lichen nitidus is a chronic dermatological condition characterized by scattered, shiny papules, typically seen in relatively young individuals. This case report details a subtype known as generalized lichen nitidus, a rare manifestation affecting the entire body area [1]. Since some treatment studies have been reported, there is a need for a standardized treatment approach.
Case report
A 6-year-old boy was referred to our hospital complaining of a skin rash covering his entire body. He had no family history of similar conditions. About 3 years ago, he developed a yellowish papular rash on his abdomen and around his eyes, which gradually spread to other parts of his body. He sought treatment from a local doctor and received moisturizers, topical steroids (hydrocortisone butyrate, Locoid ointment) as well as oral and topical antibacterial agents. Although the patient applied it only for a few days, there was no improvement, prompting his visit to our clinic. Physical examination revealed numerous small yellow papules scattered across his body (Figure 1). These papules were approximately 1 to 2 mm in size, round, and shiny, with no tendency to merge or align with pores. They were particularly concentrated around the eyes on the face, and clustered around the elbow and knee folds on the extremities. No rash was observed on the palms or soles, and the patient reported no subjective symptoms such as itching or pain. Laboratory findings showed no abnormalities. Histopathological examination revealed liquefaction degeneration. In the dermis, there was a localized infiltration of lymphocytes and giant cells. The epidermal processes at the margins extended to surround the inflammatory cells, exhibiting a characteristic “claw clutching a ball” appearance (Figure 2).
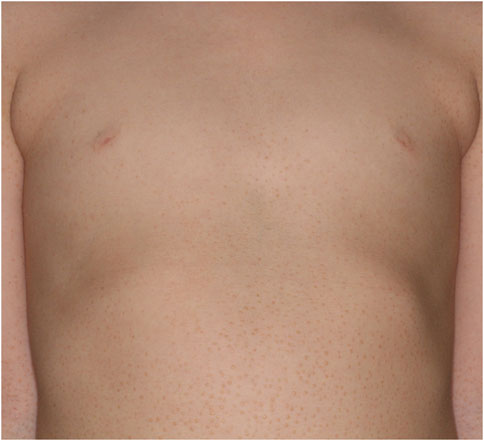
Figure 1. Clinical manifestation. Physical examination revealed numerous small yellow papules scattered across the body.
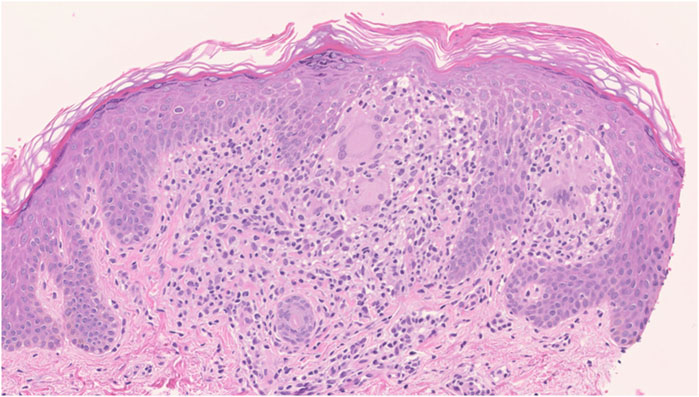
Figure 2. Histopathology. The histopathology examination shows rete ridges extending to surround inflammatory cells and giant cells, displaying a “claw clutching a ball” image.
Topical treatment was initiated, and upon obtaining consent from the patient and his parents, the medications were applied separately to the right and left sides of the patient’s body. A 25 μg/g maxacalcitol ointment (Oxarol Ointment) was applied twice a day on the right side, while a 0.1% alclometasone dipropionate ointment (ALMETA Ointment) was applied once a day on the left side. Maxacalcitol and 0.1% alclometasone dipropionate ointment were prescribed at the discretion of the outpatient dermatologist. On day 84 of the topical application, the small papules on the left side treated with alclometasone dipropionate ointment began to disappear, whereas the papules on the right side treated with maxacalcitol ointment remained unchanged (Figure 3A). Consequently, the patient was switched to topical alclometasone dipropionate ointment for the entire body. After 104 days of topical application, the rash had almost completely disappeared on both the right and left sides (Figure 3B).
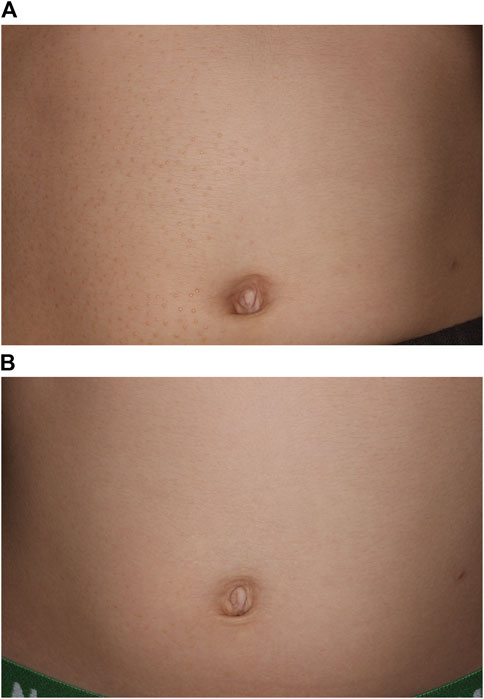
Figure 3. Clinical manifestation after treatment with topical steroid or maxacalcitol ointment. (A) After 84 days of topical application, the papules treated with alclometasone dipropionate ointment on the left side tended to disappear, while those treated with maxacalcitol ointment on the right side remained unchanged. (B) After 104 days of topical application with alclometasone dipropionate ointment, the papules had completely disappeared on both the right and left sides.
Discussion
Lichen nitidus is a chronic dermatological condition characterized by the presence of multiple, scattered, shiny papules, typically affecting relatively young individuals. While it is generally asymptomatic, some cases may present with pruritus and the Köbner phenomenon, although these occurrences are sporadic. Generalized lichen nitidus refers to variants where skin eruptions are distributed widely across the body.
Several treatment approaches have been reported for generalized lichen nitidus. The primary treatment modality often cited is topical steroids. However, alternative therapies have shown effectiveness as well. These include natural sunlight therapy, narrow-band ultraviolet B treatment, enoxaparin sodium, pimecrolimus 1% cream, astemizole, 0.03% tacrolimus ointment, PUVA (psoralen combined with ultraviolet A therapy), interferon alpha, cetirizine dihydrochloride/levamisole combination, and systemic isotretinoin [2–15]. There have been no reported instances of treatment using maxacalcitol ointment.
Based on available data, 37 cases of generalized lichen nitidus have been documented in Japan. The age range of affected patients ranged from 4 to 60 years (mean 19.6 years). Among the cases, 9 out of 24 patients experienced pruritus, while the Köbner phenomenon was observed in 7 out of 37 patients. Treatment strategies predominantly involved the use of topical steroids, administered in 27 patients, some of whom also received oral tranilast. Improvement was noted in 21 of these cases. Other therapeutic approaches included urea, narrowband-UVB therapy, cephalantin, Jumihaidokuto (a Kampo medicine), and a 10% salicylic acid-containing ointment, all of which yielded positive results. Interestingly, there were 3 cases where no treatment was administered, yet all showed improvement. In our case, we observed improvement in the skin rash at sites treated with topical steroids, while no change was noted in areas treated with topical maxacalcitol ointment. This clear disparity in treatment outcomes between topical steroids and maxacalcitol ointment underscores the effectiveness of the former in managing generalized lichen nitidus.
While some reported cases have shown mild improvement with topical steroids, our experience underscores the efficacy of topical steroids as the initial treatment choice for generalized lichen nitidus. This case demonstrates successful management of the condition in a child using topical steroids, particularly alclometasone dipropionate ointment, compared to maxacalcitol ointment. Nonetheless, further research and additional case studies are necessary to establish standardized treatment protocols for this rare subtype of lichen nitidus.
In conclusion, this case report highlights the challenges encountered in managing generalized lichen nitidus, a rare subtype of lichen nitidus characterized by widespread skin involvement. Despite previous treatments failing to yield improvement, our patient experienced significant resolution of symptoms with topical alclometasone dipropionate ointment, demonstrating its efficacy in managing this condition. Conversely, maxacalcitol ointment showed limited effectiveness, emphasizing the superiority of topical steroids in treating generalized lichen nitidus. The disparity in treatment outcomes observed in this case underscores the need for further research to establish standardized treatment protocols for this rare dermatological condition. While various treatment modalities have been explored, including alternative therapies and systemic agents, our experience supports the use of topical steroids as the initial treatment choice. However, additional studies and case reports are essential to validate these findings and optimize therapeutic strategies for patients with generalized lichen nitidus. In summary, this case report contributes to the growing body of evidence regarding the management of generalized lichen nitidus and emphasizes the importance of tailored treatment approaches guided by clinical response. By sharing our experience, we aim to enhance understanding and improve outcomes for patients afflicted with this challenging dermatological condition.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
All authors participated in the design, interpretation of the studies and analysis of the data and review of the manuscript; AS and FT wrote the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Synakiewicz, J, Polanska, A, Bowszyc-Dmochowska, M, Żaba, RW, Adamski, Z, Reich, A, et al. Generalized lichen nitidus: a case report and review of the literature. Postepy Dermatol Alergol (2016) 33(6):488–90. doi:10.5114/ada.2016.63890
2. Berman, H, Truong, A, and Cheng, CE. Pediatric generalized lichen nitidus treated with natural sunlight therapy. Pediatr Dermatol (2019) 36(5):690–2. doi:10.1111/pde.13915
3. Bilgili, SG, Karadag, AS, Calka, O, Ozdemir, S, and Kosem, M. A case of generalized lichen nitidus successfully treated with narrow-band ultraviolet B treatment. Photodermatol Photoimmunol Photomed (2013) 29(4):215–7. doi:10.1111/phpp.12037
4. Cholongitas, E, Kokolakis, G, Giannikaki, E, and Ioannidou, D. Persistent generalized lichen nitidus successfully treated with enoxaparin sodium. Am J Clin Dermatol (2008) 9(5):349–50. doi:10.2165/00128071-200809050-00012
5. Do, MO, Kim, MJ, Kim, SH, Myung, KB, and Choi, YW. Generalized lichen nitidus successfully treated with narrow-band UVB phototherapy: two cases report. J Korean Med Sci (2007) 22(1):163–6. doi:10.3346/jkms.2007.22.1.163
6. Farshi, S, and Mansouri, P. Letter: generalized lichen nitidus successfully treated with pimecrolimus 1 percent cream. Dermatol Online J (2011) 17(7):11. doi:10.5070/d365p7c1s7
7. Kim, YC, and Shim, SD. Two cases of generalized lichen nitidus treated successfully with narrow-band UV-B phototherapy. Int J Dermatol (2006) 45(5):615–7. doi:10.1111/j.1365-4632.2004.02596.x
8. Nakamizo, S, Kabashima, K, Matsuyoshi, N, Takahashi, K, and Miyachi, Y. Generalized lichen nitidus successfully treated with narrowband UVB phototherapy. Eur J Dermatol (2010) 20(6):816–7. doi:10.1684/ejd.2010.1057
9. Ocampo, J, and Torne, R. Generalized lichen nitidus. Report of two cases treated with astemizol. Int J Dermatol (1989) 28(1):49–51. doi:10.1111/j.1365-4362.1989.tb01313.x
10. Park, J, Kim, JI, Kim, DW, Hwang, SR, Roh, SG, Kim, HU, et al. Persistent generalized lichen nitidus successfully treated with 0.03% tacrolimus ointment. Eur J Dermatol (2013) 23(6):918–9. doi:10.1684/ejd.2013.2200
11. Park, JH, Choi, YL, Kim, WS, Lee, DY, Yang, JM, Lee, ES, et al. Treatment of generalized lichen nitidus with narrowband ultraviolet B. J Am Acad Dermatol (2006) 54(3):545–6. doi:10.1016/j.jaad.2005.01.137
12. Randle, HW, and Sander, HM. Treatment of generalized lichen nitidus with PUVA. Int J Dermatol (1986) 25(5):330–1. doi:10.1111/j.1365-4362.1986.tb02260.x
13. Scheler, M, Proelss, J, Brauninger, W, Bieber, T, and Wenzel, J. Generalized lichen nitidus with involvement of the palms following interferon alpha treatment. Dermatology (2007) 215(3):236–9. doi:10.1159/000106582
14. Sehgal, VN, Jain, S, Kumar, S, Bhattacharya, SN, and Singh, N. Generalized lichen nitidus in a child's response to cetirizine dihydrochloride/levamisol. Australas J Dermatol (1998) 39(1):60. Available from: https://www.ncbi.nlm.nih.gov/pubmed/9529696.
Keywords: comparative treatment course, generalized lichen nitidus, topical steroids, maxacalcitol, lichen nitidus
Citation: Taga F, Ono H, Shimada Y and Shimizu A (2024) Case report: Comparative treatment course of generalized lichen nitidus: effectiveness of topical steroids versus maxacalcitol. J. Cutan. Immunol. Allergy 7:13665. doi: 10.3389/jcia.2024.13665
Received: 16 August 2024; Accepted: 24 September 2024;
Published: 07 October 2024.
Copyright © 2024 Taga, Ono, Shimada and Shimizu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Akira Shimizu, YXNoaW1penVAa2FuYXphd2EtbWVkLmFjLmpw
 Fumiaki Taga
Fumiaki Taga Akira Shimizu
Akira Shimizu