Dear Editors,
A 50-year-old Japanese woman presented with a 3-month history of itching, pain, swelling, and raised yellowish lesions on her eyebrows. She had a history of permanent makeup (PMU) placement on her eyebrows 9 years prior. Initial examination revealed distinct, slightly elevated yellow-brown plaques and significant hair loss in the affected area (Figure 1A). Histological examination of a skin biopsy from the right eyebrow showed epithelioid granulomas with dark-brown pigments and lymphocytic infiltration, along with multinucleated giant cells without necrosis (Figures 1B, C). Given the frequent use of iron oxide in PMU inks, we performed supplementary staining using Berlin blue, which was positive around the deposited material (Figure 1D).
FIGURE 1
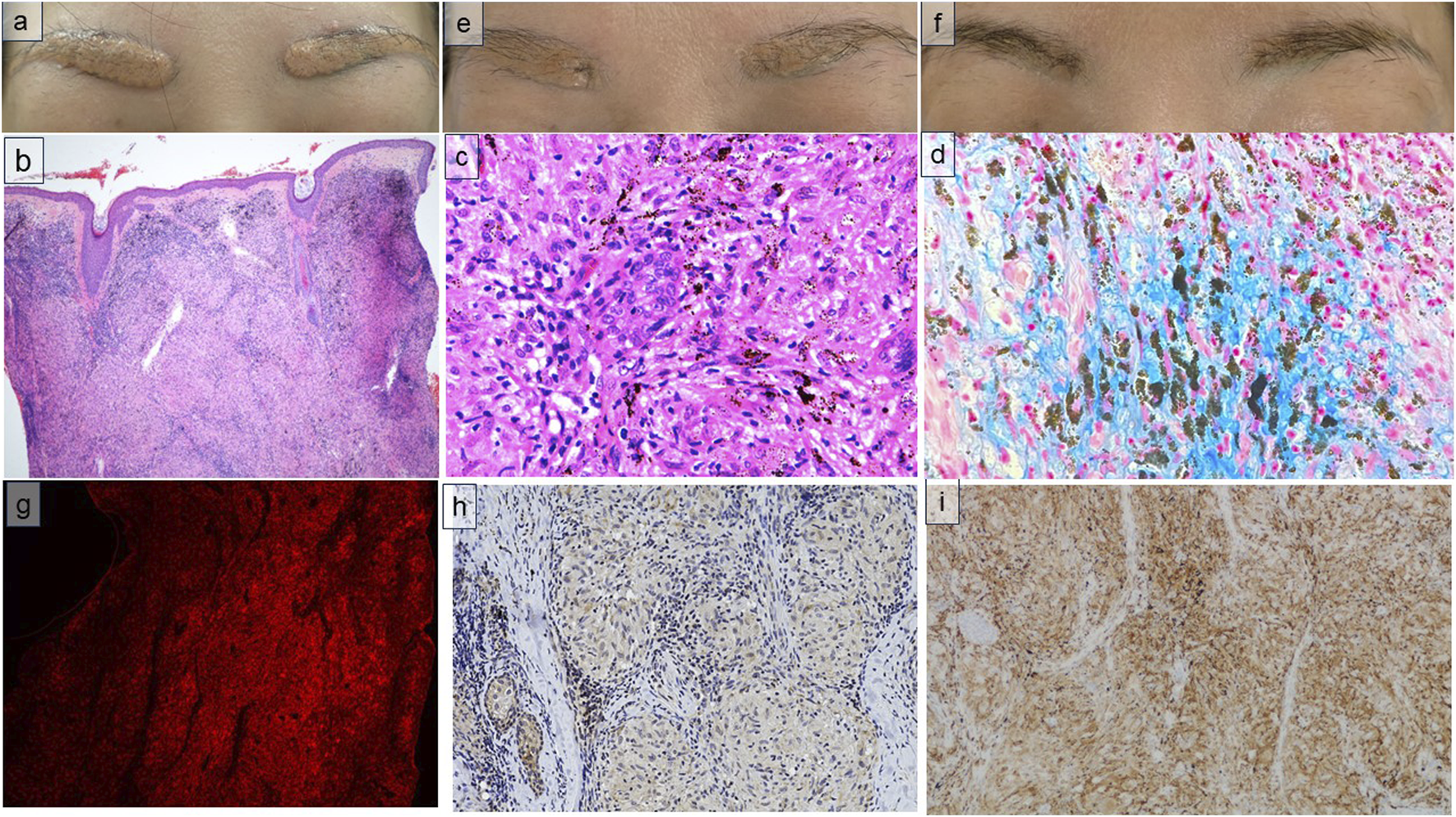
(A) The patient presented with a distinct, slightly elevated, yellow-brown plaque on her eyebrows. (B) Epithelioid granulomas in the dermis, with scattered dark-brown colorants, were observed on hematoxylin and eosin (H.E.) staining (H.E. × 40). (C) Lymphocytic infiltration surrounding the granulomas and multinucleated giant cells without necrosis were observed (H.E. × 200). (D) Berlin blue staining was positive around the deposited material (H.E. × 100). (E) After four steroid injections, the raised yellow-brown lesion flattened partially, and some hair regrowth was observed. (F) After six steroid injections, the lesions flattened almost completely, and hair loss improved. (G) Immunofluorescence staining represents Iba1+ (ionized calcium-binding adapter molecule 1) (GeneTex, Cat. No. GTX100042, Opal™ 570, × 40) cells for identification of both M1 and M2 macrophages. (H) Immunohistochemical staining represents iNOS+ (GeneTex,Cat.No.GTX15323, Brown stain, ×100) cells for identification of M1 macrophages. (I) Immunohistochemical staining represents CD163+ (Leica, 10D6 Cat. No. PA0090; Brown stain, ×100) cells for identification of M2 macrophages.
Physical examination, including a chest radiograph, and laboratory tests such as angiotensin-converting enzyme and soluble interleukin-2 receptor, revealed no abnormal findings. Based on clinical and histopathological findings, the patient was diagnosed with a sarcoidal foreign body reaction to PMU tattoo ink. Various treatments for sarcoidal foreign body reactions to PMU ink are effective, including topical, oral, and intralesional steroids, tacrolimus, minocycline, doxycycline, and methotrexate [1]. The patient had already been applying a topical steroid, with no obvious improvements. Therefore, we administered monthly steroid injections in the eyebrows using a solution (10 mg/mL) comprised of triamcinolone acetonide and 1% lidocaine hydrochloride. Itching improved within 2 weeks of the first steroid injection. After the fourth injection, the flat yellowbrown raised lesion partially flattened, and some hair regrowth was observed (Figure 1E). After six injections, the lesions had almost completely flattened, hair loss had improved, and the patient expressed satisfaction with the aesthetic outcome (Figure 1F). However, itching recurred after the injections were stopped. Therefore, injections were continued every 2–3 months to prevent relapse of itching.
Although several cases of granulomatous reactions due to PMU placement in the eyebrows have been reported, distinguishing between the initial manifestation of sarcoidosis and a sarcoidal foreign body reaction is difficult. Even patients who exhibit localized sarcoidal reactions, as in the present case, are thought to have a predisposition to sarcoidosis. Therefore, this patient should be closely followed for the development of sarcoidosis [2].
In the present case, the patient developed a sarcoid-like foreign body reaction 9 years after a PMU procedure using blonde ink. While the composition of the ink is unknown, positive results on Berlin blue staining suggest that the ink contained iron oxides. The mechanism for this long latency period is thought to involve the gradual degradation of ink components. Chronic sun exposure may cause the ink components to break down slowly, generating highly reactive byproducts, which may function as new antigens, potentially triggering a granulomatous reaction. It is important to note that the eyebrow area is difficult to protect with sunscreen. In this case, the difficulty in applying sunscreen to the eyebrow area supports the hypothesis that sun exposure played a significant role in the development of the reaction [1].
Recent studies have identified the roles of M1 and M2 macrophages in inflammation promotion and tissue repair/inflammation suppression, respectively. Previous studies have associated sarcoidosis with a significant increase in M2 macrophages [3]. In the present case, we performed ionized calcium-binding adapter molecule 1 (Iba1) immunostaining to identify both M1 and M2 macrophages, along with immunostaining for inducible nitric oxide synthase (iNOS) and CD163 as M1 and M2 macrophage markers, respectively [4]. We observed a higher density of CD163-positive cells compared to iNOS-positive cells, indicating an increase in M2 macrophages (Figures 1G–I). It is hypothesized that in granuloma formation, an initial Type 1 T helper immune response involving M1 macrophages occurs, with a transition from M1 to M2 macrophages [5]. Given the predominance of M2 macrophages in the present case, the transition to the resolution phase of inflammation might have been underway.
In summary, we successfully treated sarcoidal foreign body reactions due to PMU with local steroid injections. We identified the involvement of M2 macrophages in the observed reaction to PMU, and this contribution has not been previously reported. Thus, our findings provide new insights into the mechanisms underlying PMU-associated sarcoidal reactions.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
Ethical approval was not required for the studies involving humans because this study presents a single case report. The studies were conducted in accordance with the local legislation and institutional requirements. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YF contributed to the presentation and writing of the manuscript. AF was responsible for patient treatment, supervised the manuscript, and is the corresponding author. SaM assisted AF in patient treatment. KK is the dermatologist at the clinic who first examined the patient. ShM performed the final review to assess the suitability of the manuscript for submission. All authors contributed to the article and approved the submitted version.
Funding
The authors declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Kluger N . Sarcoidosis on tattoos: a review of the literature from 1939 to 2011. Sarcoidosis Vasc Diffuse Lung Dis (2013) 30:86–102.
2.
Yamamoto T . Infiltrative scar and scar sarcoidosis as a cutaneous manifestation of systemic sarcoidosis. J Dermatol (2022) 132:1665–70. 10.14924/dermatol.132.1665
3.
Shamaei M Mortaz E Pourabdollah M Garssen J Tabarsi P Velayati A et al Evidence for M2 macrophages in granulomas from pulmonary sarcoidosis: a new aspect of macrophage heterogeneity. Hum Immunol (2018) 79:63–9. 10.1016/j.humimm.2017.10.009
4.
Lisi L Ciotti GMP Braun D Kalinin S Currò D Dello RC et al Expression of iNOS, CD163 and ARG-1 taken as M1 and M2 markers of microglial polarization in human glioblastoma and the surrounding normal parenchyma. Neurosci Lett (2017) 645:106–12. 10.1016/j.neulet.2017.02.076
5.
Asai J . What is new in the histogenesis of granulomatous skin diseases?J Dermatol (2017) 44:297–303. 10.1111/1346-8138.13662
Summary
Keywords
CD68, CD163, M1 macrophage, M2 macrophage, permanent makeup
Citation
Furukawa Y, Fukunaga A, Munemoto S, Konishi K and Moriwaki S (2024) A case of sarcoidal foreign body reaction to permanent makeup: the involvement of M2 macrophages. J. Cutan. Immunol. Allergy 7:13728. doi: 10.3389/jcia.2024.13728
Received
02 September 2024
Accepted
24 September 2024
Published
08 October 2024
Volume
7 - 2024
Updates
Copyright
© 2024 Furukawa, Fukunaga, Munemoto, Konishi and Moriwaki.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Atsushi Fukunaga, atsushi.fukunaga@ompu.ac.jp
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.