Dear Editors,
Immunoglobulin A (IgA) vasculitis is an immune complex-mediated vasculitis characterized by the involvement of small blood vessels in various organ systems [1]. The most characteristic symptom is palpable purpura in the buttocks and lower extremities. Here we report a case of IgA vasculitis presenting with annular erythema on the abdomen.
A 41-year-old man was referred to our hospital due to skin lesions and joint pain on the lower extremities. The symptoms appeared 1 week before the first visit. He also presented with abdominal discomfort. Physical examination revealed palpable purpura on the dorsal foot and lower extremities (Figure 1A). Purpura and pigmentation were also observed on the abdomen and back. The patient had no underlying diseases. There was no history of antecedent infections or recent medications. Laboratory tests showed elevated serum levels of C-reactive protein (15.03 mg/dL [normal, 0.00–0.14 mg/dL]), erythrocyte sedimentation rate (37 mm [normal, <2–10 mm]), C3 (158 mg/dL [normal, 73–138 mg/dL]), C4 (33 mg/dL [normal, 11–31 mg/dL]), CH50 (63.1 U/mL [normal, 30.0–46.0 U/mL]), and anti-streptolysin O antibody (202 U/mL [normal, <186 U/mL]). White blood cell count, renal function, and serum IgA were within normal range. A urinary test showed hematuria and proteinuria. Histopathological findings of palpable purpura on the left lower extremity showed subepidermal bullae and inflammatory infiltration in the upper dermis (Figure 1B). Erythrocyte extravasation and infiltration of neutrophils and lymphocytes with nuclear dusts of neutrophils were observed around the small vessels in the upper dermis (Figure 1C). Direct immunofluorescence did not detect any immunoglobulin or complement deposition. Skin lesions resolved spontaneously at rest. However, macular erythema with purpura was observed on the abdomen 6 days after the first visit (Figure 1D). The next day, macular erythema disappeared and annular erythema with purpura appeared (Figure 1E). Although abdominal pain was not observed, the fecal occult blood test was positive. Histopathological findings from annular erythema with purpura on the abdomen revealed leukocytoclastic vasculitis. Direct immunofluorescence detected granular IgA deposition in the superficial dermal vessels (Figure 1F). A diagnosis of IgA vasculitis was made. Annular erythema disappeared spontaneously in 3 days. Urinary findings and abdominal discomfort also resolved without any specific treatment. Persistent joint pain had been treated with nonsteroidal anti-inflammatory drugs.
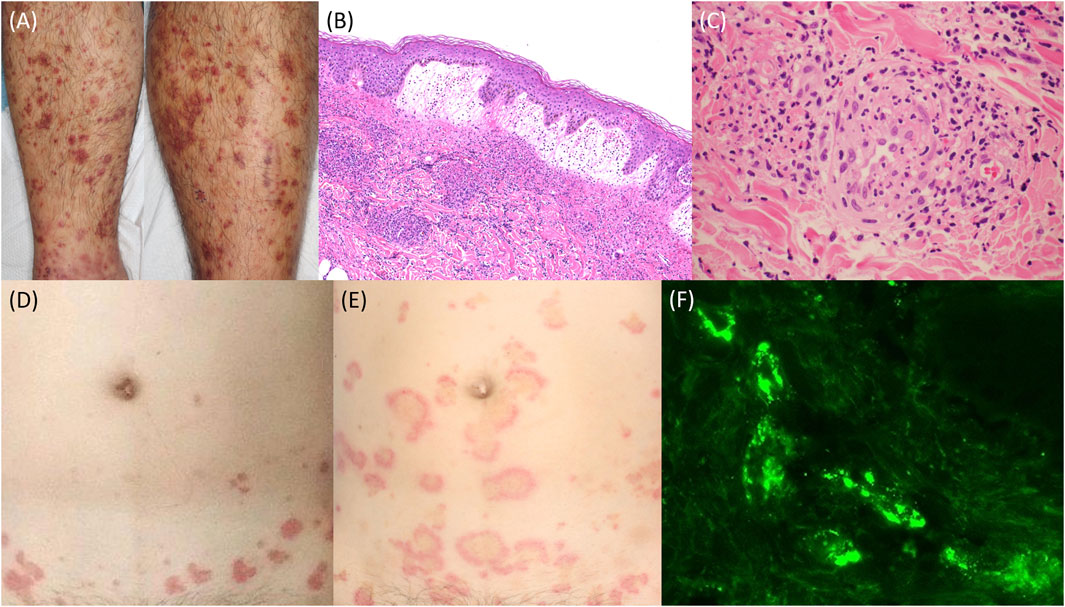
Figure 1. (A) Palpable purpura on the lower extremities. (B) Histopathology showing subepidermal bullae and inflammatory infiltration in the upper dermis (hematoxylin and eosin staining; ×100). (C) Histopathology showing leukocytoclastic vasculitis (hematoxylin and eosin staining; ×400). (D) Macular erythema on the abdomen. (E) Annular erythema on the abdomen. (F) Direct immunofluorescence showing granular IgA deposition in the superficial dermal vessels.
Annular erythema is a rare symptom of leukocytoclastic vasculitis. To the best of our knowledge, there has been only one case report of annular IgA vasculitis [2]. In IgA vasculitis, skin lesions are the initial symptom and purpura is the most crucial diagnostic factor. However, the eruption can start as erythematous macular or urticarial lesions, which then progress to blanching papules, and eventually develop into palpable purpura [3]. Vesicular eruptions, haemorrhagic bullae, and erythema multiforme-like lesions can also be observed [3]. There are several theories to explain the development of annular lesions; a local zone of central tissue anergy, oscillations in inflammatory mediators, and the spread of inflammation along the cutaneous vascular network [4]. It is also speculated that mild symptoms of vascular damage resolved spontaneously showing central healing without purpura or pigmentation. In annular erythema, the differential diagnosis includes several entities. Clinicians should pay attention to the possibility of IgA vasculitis in patients with annular erythema. In our case, IgA deposition was observed in annular erythema, while that was not in palpable purpura. A skin biopsy should be taken from early lesions to avoid a delayed diagnosis.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
ShK and KK wrote the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
References
1. Roache-Robinson, P, Killeen, RB, and Hotwagner, DT. IgA vasculitis (Henoch-Schonlein purpura). Treasure Island (FL): StatPearls (2024).
2. Belfeki, N, Ghriss, N, Kammoun, S, Zayet, S, Moini, C, and Terrier, B. Annular leukocytoclastic vasculitis: a new feature of IgA vasculitis. Eur J Case Rep Intern Med (2024) 11(5):004278. doi:10.12890/2024_004278
3. Di Ludovico, A, Rinaldi, M, Lauriola, F, Ciarelli, F, La Bella, S, Gualdi, G, et al. The diagnostic role of skin manifestations in rheumatic diseases in children: a critical review of paediatric vasculitis. Int J Mol Sci (2024) 25(13):7323. doi:10.3390/ijms25137323
Keywords: adult-onset, annular erythema, annular IgA vasculitis, IgA vasculitis, palpable purpura
Citation: Kobayashi S, Kamiya K, Fukuizumi S, Kado S, Okada H, Sato A and Komine M (2024) A case of immunoglobulin A vasculitis presenting with annular erythema. J. Cutan. Immunol. Allergy 7:13967. doi: 10.3389/jcia.2024.13967
Received: 22 October 2024; Accepted: 08 November 2024;
Published: 15 November 2024.
Copyright © 2024 Kobayashi, Kamiya, Fukuizumi, Kado, Okada, Sato and Komine. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Koji Kamiya, bTAxMDIza2tAamljaGkuYWMuanA=
 Shuhei Kobayashi
Shuhei Kobayashi Koji Kamiya
Koji Kamiya