Dear Editors,
Erythema elevatum diutinum (EED) is a rare and chronic cutaneous leukocytoclastic vasculitis [1]. The cause of EED still remains unknown, but immune complex deposition in dermal blood vessels is thought to be associated with the onset of the disease [1]. Here, we report a rare case of EED associated with immunoglobulin A (IgA) vasculitis.
A 72-year-old man presented with arthralgia and palpable purpura on his lower extremities (Figure 1A). There was no history of any antecedent infections, but he had a history of IgA nephropathy and rheumatoid arthritis (RA), which had been treated with oral prednisolone 2 mg/day for 2 months. Laboratory tests showed elevated serum levels of white blood cell count (10,700/µL [normal, 3,300–8,600/µL]), C-reactive protein (3.16 mg/dL [normal, 0.00–0.14 mg/dL]), creatinine (4.01 mg/dL [normal, 0.65–1.07 mg/dL]), and IgA (532 mg/dL [normal, 93–393 mg/dL]). A urinary test showed hematuria and proteinuria. Histopathological findings from palpable purpura on the left lower extremity showed inflammatory infiltration in the upper dermis (Figure 1B). Infiltration of neutrophils and lymphocytes with nuclear dusts of neutrophils was observed around the small vessels in the upper dermis (Figure 1C). Direct immunofluorescence did not detect any immunoglobulin or complement deposition. A diagnosis of IgA vasculitis was made based on the EULAR/PRINTO/PRES classification criteria. The dose of oral prednisolone was increased to 5 mg/day and his symptoms improved for 10 days. However, 1 month later, crusty red–to-violet nodules appeared on his fingers and elbow (Figure 1D). Histopathological findings from the nodule on the left finger showed prominent edema and dense inflammatory infiltration in the dermis (Figure 1E). Infiltration of neutrophils, lymphocytes, eosinophils, and histiocytes with nuclear dusts of neutrophils was observed around the vessels in the dermis (Figure 1F). A diagnosis of EED was made. Although diaminodiphenyl sulfone 100 mg/day was temporarily initiated, the treatment was discontinued due to anemia. The dose of oral prednisolone was increased to 15 mg/day and gradually improved his skin lesions.
FIGURE 1
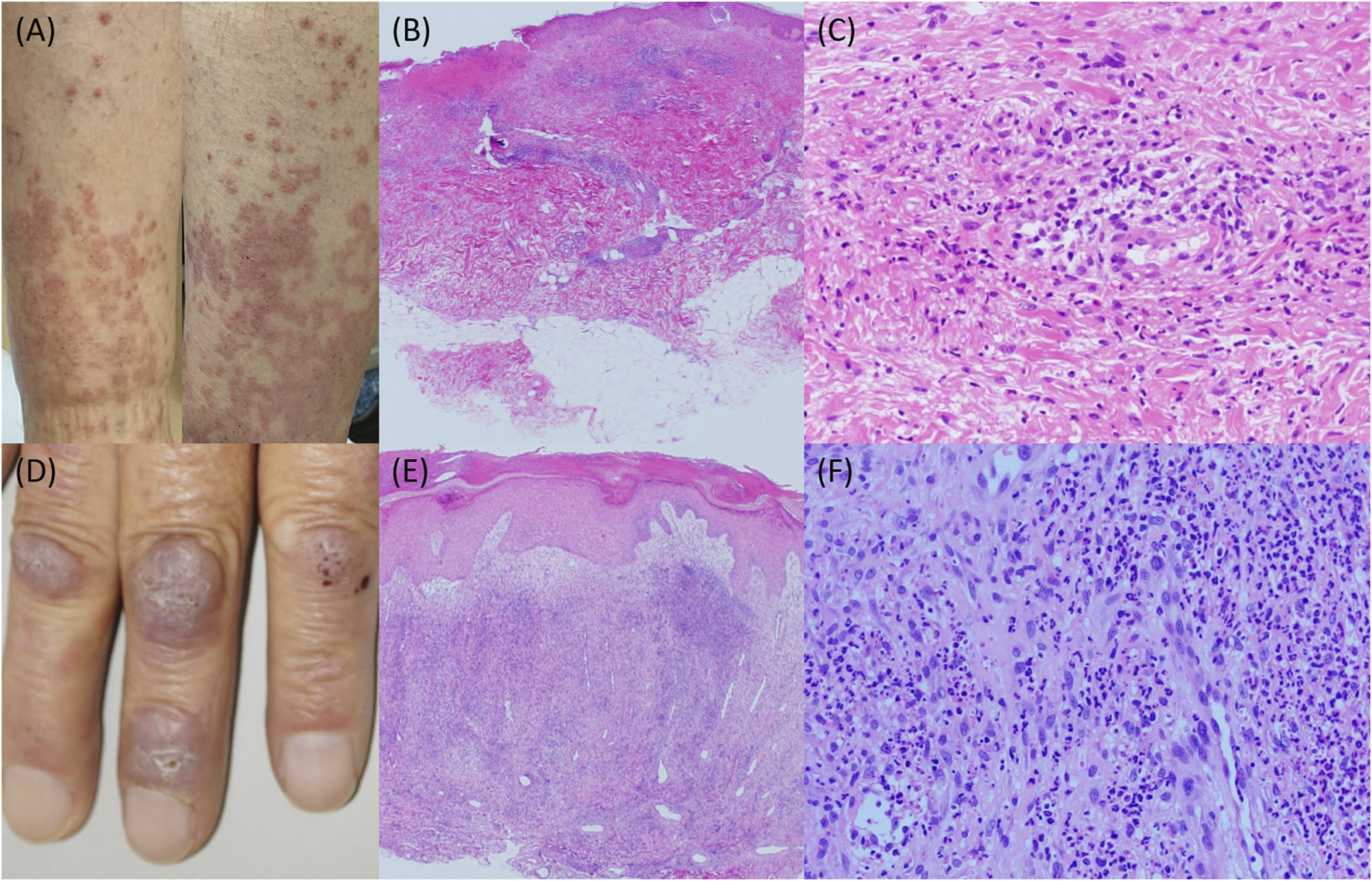
(A) Palpable purpura on the lower extremities. (B) Histopathology showing inflammatory infiltration in the upper dermis (hematoxylin and eosin staining; ×20). (C) Histopathology showing leukocytoclastic vasculitis (hematoxylin and eosin staining; ×200). (D) Crusty red-to-violet nodules on the fingers. (E) Histopathology showing prominent edema and dense inflammatory infiltration in the dermis (hematoxylin and eosin staining; ×20). (F) Histopathology showing leukocytoclastic vasculitis (hematoxylin and eosin staining; ×200).
The diagnosis of EED is made by the characteristic clinical findings and histopathological findings [2]. Although the cause of EED is not fully understood, EED has been reported in association with various systemic diseases, including hematologic diseases, infections, and autoimmune diseases [1]. It is possible that the onset of EED was associated with RA. When EED develops in patients with RA, the disease severity of EED is associated with high serum levels of rheumatoid factor [3, 4]. In our case, serum levels of rheumatoid factor were high but not elevated during the clinical course. Thus, it is speculated that the onset of EED was associated with IgA vasculitis. IgA vasculitis shares many pathogenic similarities with IgA nephropathy [5]. In our case, the disease severity of IgA nephropathy was well controlled with normal serum IgA level. However, serum IgA level had been elevated after the onset of IgA vasculitis. Aberrant IgA and IgA complexes were associated with the pathogenesis of not only IgA vasculitis but also EED. To the best of our knowledge, there have been no case reports of EED associated with IgA vasculitis. Further case accumulation is needed to clarify the underlying pathomechanisms of EED.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
CY and KK wrote the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
References
1.
Newburger J Schmieder GJ . Erythema elevatum diutinum. Treasure Island (FL): StatPearls (2024).
2.
Gibson LE el-Azhary RA . Erythema elevatum diutinum. Clin Dermatol (2000) 18(3):295–9. 10.1016/s0738-081x(99)00120-0
3.
Bittencourt MS Serruya T Loureiro LO De Souza ADC Neri CC Moutinho ATM et al Erythema elevatum diutinum in a patient with rheumatoid arthritis. Dermatol Online J (2023) 29(5). 10.5070/D329562408
4.
Nakajima H Ikeda M Yamamoto Y Kodama H . Erythema elevatum diutinum complicated by rheumatoid arthritis. J Dermatol (1999) 26(7):452–6. 10.1111/j.1346-8138.1999.tb02025.x
5.
Song Y Huang X Yu G Qiao J Cheng J Wu J et al Pathogenesis of IgA Vasculitis: An Up-To-Date Review. Front Immunol (2021) 12:771619. 10.3389/fimmu.2021.771619
Summary
Keywords
erythema elevatum diutinum, IgA nephropathy, IgA vasculitis, leukocytoclastic vasculitis, rheumatoid arthritis
Citation
Yamamoto C, Kamiya K, Toyama Y, Okada H, Kado S, Sato A and Komine M (2024) A case of erythema elevatum diutinum associated with immunoglobulin A vasculitis. J. Cutan. Immunol. Allergy 7:14007. doi: 10.3389/jcia.2024.14007
Received
30 October 2024
Accepted
18 November 2024
Published
27 November 2024
Volume
7 - 2024
Updates
Copyright
© 2024 Yamamoto, Kamiya, Toyama, Okada, Kado, Sato and Komine.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Koji Kamiya, m01023kk@jichi.ac.jp
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.