Dear Editors,
A 41-year-old woman had been diagnosed with generalized pustular psoriasis (GPP) for 4 years, both clinically and histologically (Figure 1A). Genetic analysis for IL36RN was not conducted according to the patient’s decision. Her symptoms had been stabilized with cyclosporine (2 mg/kg/day). However, 2 weeks prior to her admission, pustules and erythema appeared on her left lower lumbar region, and the skin lesions progressively worsened. Despite increasing the cyclosporine dosage to 3 mg/kg/day, the skin lesions did not improve and the patient developed a fever.
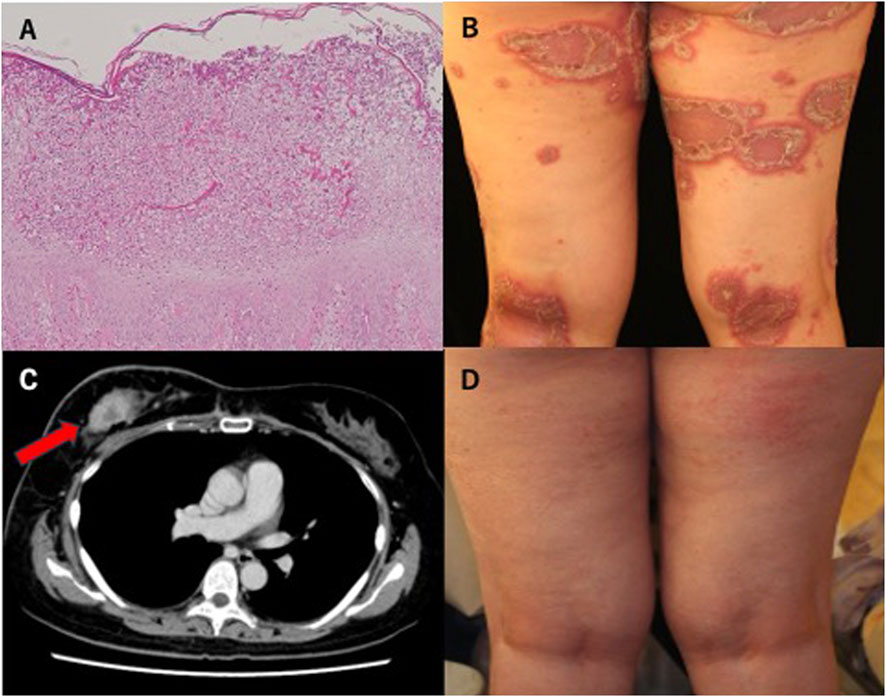
Figure 1. (A) Pathohistological image of spongiform pustules of Kogoj with hematoxylin–eosin staining. (B) Rash with pustules on bilateral legs on admission. (C) Enhanced mass lesion measuring 2.5 cm × 4 cm in the right breast (CT scan image). (D) After five courses of GMA, erythema and pustules were relatively improved.
Physical examination revealed erythema and pustule formation on the trunk, upper extremities, and femoral region, covering approximately 30% of the body surface area (Figure 1B), accompanied by pyrexia of 39.2°C. Initial laboratory results showed leukocytosis (12,700/μL) with neutrophilia (81%) and an elevated C-reactive protein level (6.86 mg/dL). A bacteriologic swab culture was negative. A CT scan revealed a mass lesion measuring 2.5 cm × 4 cm in the right breast and axillary lymphadenopathy (Figure 1C). Based on the CT findings, the patient was suspected of having left breast cancer.
To manage GPP, granulocyte and monocyte adsorption (GMA) was initiated to minimize the possible adverse effects on the suspected cancer. During the five courses of GMA, the patient’s body temperature returned to a normal degree and the pustules and erythema gradually improved (Figure 1D). However, the erythema on her trunk remained. Subsequently, subcutaneous brodalumab administration was introduced (210 mg at weeks 0, 1, 2, and every 2 weeks thereafter). In the meantime, the patient underwent a left breast mastectomy and was diagnosed with right breast cancer with right axillary lymph node metastasis. The patient started hormonal therapy, and tumor markers showed a decreasing trend. However, she gradually developed skin metastases, which grew despite treatment.
The patient died of breast cancer 4 years after diagnosis. Brodalumab was continued for 4 years, during which no recurrence of GPP was observed.
GPP is a rare and severe neutrophilic skin disease characterized by widespread erythema and acute pustular eruptions. Flare-ups of GPP can result in life-threatening conditions, making effective treatment essential. Although many of the systemic therapies for plaque psoriasis can be adapted for the treatment of GPP, GPP is now regarded as a distinct entity from plaque psoriasis with a different pathophysiologic mechanism and the safety profiles of these treatments should be evaluated independently in GPP. GMA is a treatment that selectively removes myeloid-lineage leukocytes from peripheral blood, avoiding the potentially harmful effects of systemic oral drugs [1]. In our case, GMA was selected as the initial treatment because the therapeutic strategy for the breast cancer had not yet been determined. Meanwhile, etretinate, corticosteroids, biologics, and their combination are also strong candidates for acute exacerbated GPP. Subsequently, brodalumab allowed the patient to concurrently undergo chemotherapy for breast cancer. A review of the use of IL-17A inhibitors in psoriasis patients with a history of malignancy indicated that only 2 out of 12 patients experienced malignant progression, with no correlation to biologic therapy [2]. While we have found only a few case series or case reports regarding the management of GPP associated with malignancy, this case underscores the potential of brodalumab as a safe and effective long-term treatment option for GPP, even in patients with malignancy. In fact, our case showed no rapid breast cancer progression with brodalumab.
Recurrence of GPP is common, and exacerbating factors include infection, pregnancy, drug withdrawal, and smoking [3]. In our case, while cyclosporine had previously been effective, the malignancy may have worn off the drug.
The humanized anti-IL-36 receptor antibody spesolimab has been approved for the treatment of acute GPP. Recent findings have indicated that IL-36 increases the number of tumor-infiltrating regulatory T cells (Treg) in vivo. Although further investigation is required, this observation suggests that spesolimab may not be a strong driver of tumor progression [4].
In conclusion, due to the rarity of the disease, selecting an appropriate therapy for GPP is often challenging especially considering the management of complications. Further accumulation of the treatment experience would be desirable.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
MT drafted the manuscript and all authors listed have made a substantial and direct contribution to the work and approved it for publication. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
References
1. Gnesotto, L, Mioso, G, and Alaibac, M. Use of granulocyte and monocyte adsorption apheresis in dermatology (Review). Exp Ther Med (2022) 24(2):536. doi:10.3892/etm.2022.11463
2. Bellinato, F, Gisondi, P, Maurelli, M, and Girolomoni, G. IL-17A inhibitors in patients with chronic plaque psoriasis and history of malignancy: a case series with systematic literature review. Dermatol Ther (2021) 34(2):e14889. doi:10.1111/dth.14889
3. Rivera-Díaz, R, Daudén, RE, Carrascosa, JM, Cueva, P, and Puig, L. Generalized pustular psoriasis: a review on clinical characteristics, diagnosis, and treatment. Dermatol Ther (Heidelb) (2023) 13(3):673–88. doi:10.1007/s13555-022-00881-0
Keywords: generalized pustular psoriasis, biologics, breast cancer, psoriasis, granulocyte and monocyte adsorption
Citation: Takahashi M, Tsuchihashi H and Watanabe R (2025) Generalized pustular psoriasis with breast cancer successfully treated with granulocyte and monocyte adsorptive aphaeresis and brodalumab. J. Cutan. Immunol. Allergy 8:14441. doi: 10.3389/jcia.2025.14441
Received: 04 February 2025; Accepted: 04 March 2025;
Published: 13 March 2025.
Copyright © 2025 Takahashi, Tsuchihashi and Watanabe. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Miho Takahashi, bS50YWthaGFzaGlAanVudGVuZG8uYWMuanA=
 Miho Takahashi
Miho Takahashi Hitoshi Tsuchihashi
Hitoshi Tsuchihashi Rei Watanabe
Rei Watanabe