- 1Department of General Medicine, Japanese Red Cross Kagoshima Hospital, Kagoshima, Japan
- 2Department of Dermatology, Jichi Medical University Hospital, Shimotuke, Japan
- 3Department of Dermatology, National Sanatorium Amami-Wakouen, Amami, Japan
- 4Department of Hematology, Kirishima Medical Center, Kirishima, Japan
- 5Internal Medicine, Kagoshima Prefecture Oshima Hospital, Amami, Japan
Dear Editors,
A 77-year-old woman with type 2 diabetes mellitus and hypertension presented to our hospital with swelling in the right leg. The patient had been treated with antibiotics for cellulitis 3 years before admission and experienced recurrent hospitalization for right leg cellulitis (Figure 1A). Despite antibiotic and diuretic therapies, the swelling did not resolve completely. She did not report fever, night sweats, and weight loss.
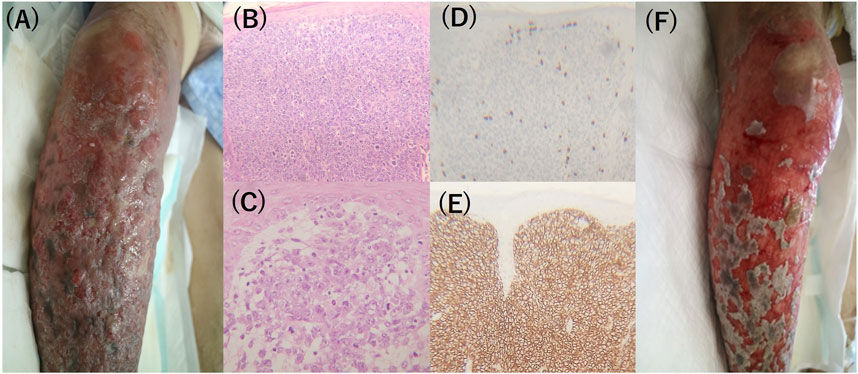
Figure 1. Clinical and histopathological findings of the patient. (A) Swelling and papillomatous changes of lower leg were observed 1 month prior to admission. (B, C) Hematoxilin and eosin staining of the biopsy specimen showed diffuse and condensed infiltration of large round cells in the upper dermis through adipose tissue (200×, 400×). (D) CD3 staining was negative in infiltrating cells (×100). (E) CD20 staining showed diffuse positive staining in infiltrating cells (×200). (F) Necrotized nodules, crusts, and erosive of lower leg after the chemotherapy.
Clinical examination revealed diffuse swelling and redness extending from the right thigh to the calf. Numerous infiltrative plaques and nodules with irregular borders, 1–2 cm in size, were present within the erythematous lesions. No pain or tenderness was observed. Laboratory workup revealed anemia, hypoalbuminemia, elevated C-reactive protein, and a soluble interleukin-2 receptor (sIL-2R) level of 25,700 IU/mL. Computed tomography scan revealed nodules in the left breast and lungs. Core needle biopsy of the lesion on the left breast confirmed an invasive ductal carcinoma. Punch biopsy of the skin lesion on the right leg revealed dense and diffuse infiltration of atypical cells with large nuclei under the subcutis. Immunohistochemical staining was negative for CD3, CD10, and CD138 and positive for CD20, CD-79a, MUM-1, BCL-6, BCL-2, and PD-L1 (Figures 1B–E). Hence, PCDLBCL-LT (primary cutaneous diffuse large B-cell lymphomas-leg type) was diagnosed. After diagnosis, she was started on R-CHOP chemotherapy (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone). The skin lesion gradually epithelialized (Figure 1F) and sIL-2R level decreased. Despite treatment, the patient died of multiple organ failure 2 months after admission.
PCDLBCL-LT presenting as cellulitis-like is rare, with only a few reported cases [1–3]. Previous reports initially misdiagnosed cases as bacterial infections. DLBCL is a non-Hodgkin lymphoma that occurs with extranodal or nodal involvement. The primary sites of the extranodal type include the gastrointestinal tract, head and neck, skin, and soft tissues. PCDLBCL was diagnosed if a patient presented with no extracutaneous involvement upon diagnosis. The patient presented with left breast cancer and lung nodules. This patient showed a 3-year history of repeated cellulitis in the right leg, which we initially assumed to be DLBCL. Although we have no definite evidence because of the lack of a chest radiography 3 years before her first visit, we speculated that this patient had PCDLBCL-LT, which may have spread to the lungs as multiple nodules. PCDLBCL-LT typically present as nodules, and rarely mimic diffuse cellulitis-like clinical findings. The diagnosis of PCDLBCL presenting with cellulitis-like is challenging because of its rarity and clinical features. Provided its aggressive pathology [4], this disease should be considered if patients do not respond to antibiotic therapies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
TK and MK conceived and wrote the manuscript. NO and YM contributed to determining the treatment plan and MB provided histology images. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
References
1. Long, V, Liang, MW, Lee, JSS, and Lim, JH. Two instructive cases of primary cutaneous diffuse large B-cell lymphoma (leg type) mimicking cellulitis and sporotrichosis. JAAD Case Rep (2020) 6(9):815–8. doi:10.1016/j.jdcr.2020.06.043
2. Awad, M, Holzwanger, E, and Jubbal, S. A unique presentation of cutaneous diffuse large B-cell lymphoma. Case Rep Dermatol Med (2020) 2020:8310602. doi:10.1155/2020/8310602
3. Huang, SF, and Liu, WC. A rare case of primary cutaneous diffuse large B-cell lymphoma, leg type, presenting as cellulitis: a case report. J Surg Case Rep (2021) 6:rjab227. doi:10.1093/jscr/rjab227
Keywords: cellulitis, primary cutaneous diffuse large B-cell lymphoma, PCDLBCL, leg type, PCDLBCL-LT
Citation: Kuribayashi T, Komine M, Baba M, Ohnou N and Morita Y (2025) Diffuse large B-cell lymphoma misdiagnosed as cellulitis. J. Cutan. Immunol. Allergy 8:14541. doi: 10.3389/jcia.2025.14541
Received: 25 February 2025; Accepted: 31 March 2025;
Published: 08 April 2025.
Copyright © 2025 Kuribayashi, Komine, Baba, Ohnou and Morita. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tamotsu Kuribayashi, bTE0MDQydGtAZ21haWwuY29t
 Tamotsu Kuribayashi
Tamotsu Kuribayashi Mayumi Komine
Mayumi Komine Mayumi Baba3
Mayumi Baba3