Abstract
Medical professional environments are becoming increasingly multicultural, international, and diverse in terms of its specialists. Many transplant professionals face challenges related to gender, sexual orientation or racial background in their work environment or experience inequities involving access to leadership positions, professional promotion, and compensation. These circumstances not infrequently become a major source of work-related stress and burnout for these disadvantaged, under-represented transplant professionals. In this review, we aim to 1) discuss the current perceptions regarding disparities among liver transplant providers 2) outline the burden and impact of disparities and inequities in the liver transplant workforce 3) propose potential solutions and role of professional societies to mitigate inequities and maximize inclusion within the transplant community.
Introduction
Over the last few years, medical professional environments have seen a change with increasing workforce diversity due to immigration as well as exponential growth of women and minority populations among medical trainees. The positive impact of diversity is well recognized, and it is promising to see the evolving knowledge and research in this area (1–28)1; yet, many professionals continue to face discriminations related to gender, racial background, sexual orientation, or inequities in terms of access to leadership positions, compensation, or professional promotions. Active plans are thus needed by transplant stakeholders both at global and institutional scales to reduce discrimination and to promote female and minorities access to leadership positions. The current review focuses on the burden and impact of disparities and proposes potential solutions to mitigate these inequities.
Current Perceptions About Equity, Diversity, and Inclusion Among Liver Transplantation Professionals and the Impact of Disparity and Inequity Among Liver Transplantation Workforce
According to a recent survey by the Equity, Diversity, and Inclusion (EDI) Committee of the International Liver Transplantation Society (ILTS), 35% of liver transplantation (LT) professionals reported a form of discrimination (1). The reasons for very low rates of woman leadership are consistent across the reports (2–5). A survey by the ILTS EDI Committee, which included 243 transplant centers globally, reported that only 32 (13.2%) had at least 1 woman as the director of LT, chief of transplant surgery, or chief of transplant hepatology (6) while another survey found that woman leadership was present in only 8% of 856 transplant programs globally (1) (Figure 1). Lowest woman leadership was in transplant surgery followed by hepatology and anesthesia (14.2% vs. 20% vs. 32.1% respectively, p = 0.046) (1). Disparities are also notable in the academic sphere, affecting the proportion of female professionals and minorities represented in senior authorship and transplant journals’ editorial boards (7, 8).
FIGURE 1
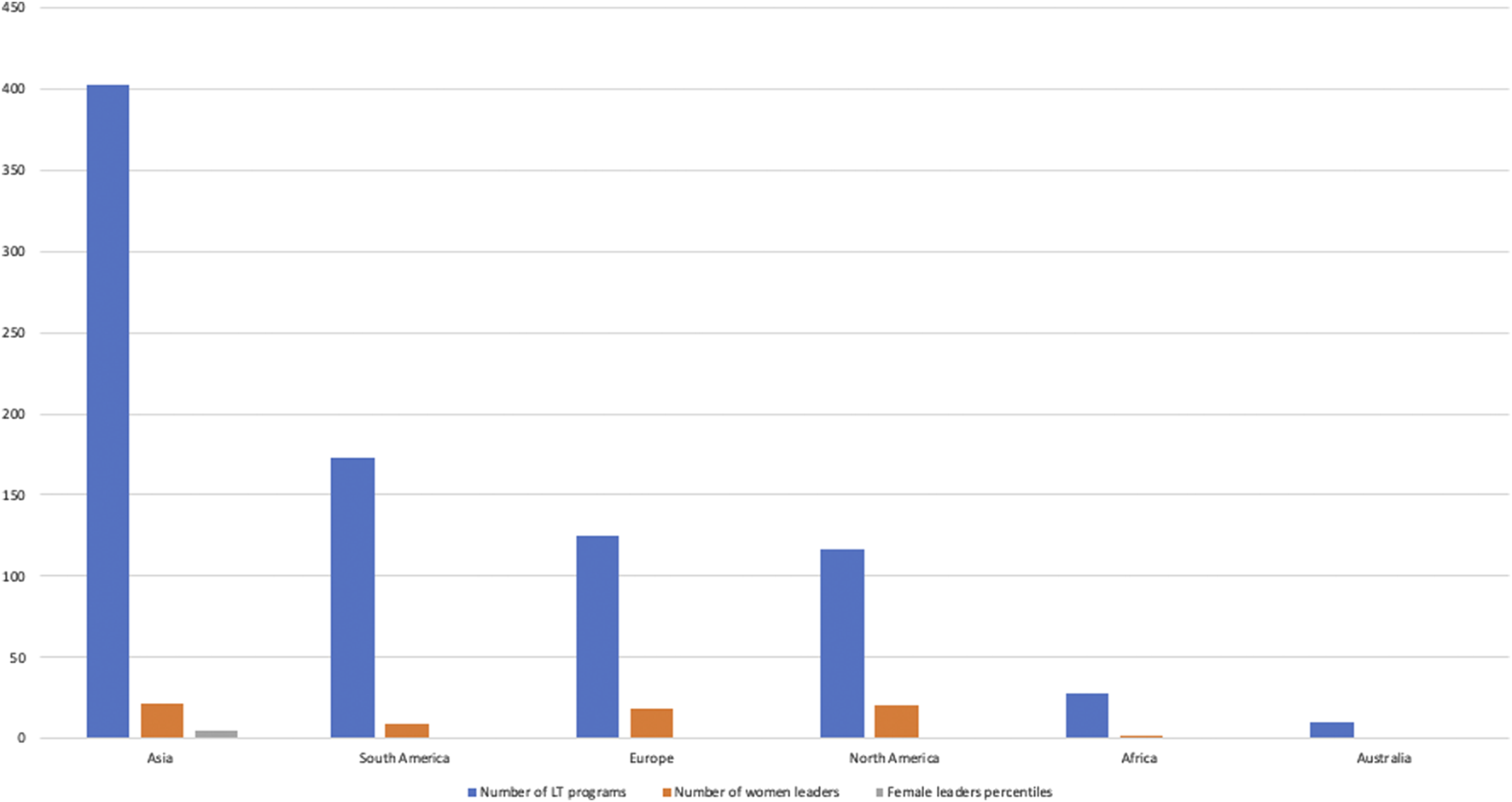
Global distribution of woman leadership in liver transplantation—adapted from Aguilera V et al. (1).
Female surgeons face obstacles, not only in leadership but also advancing their technical skills; as surgeons they are more commonly assigned as assistant surgeon as opposed to being primary surgeon for complex cases; consequently, they end-up having overall less case numbers within the same specialty or less cases for complex cases (9–11). They also face obstacles based on societal perceptions and not having supportive systems for an equitable career growth (9–11). In relation to these issues, the high incidence of attrition experienced by early-career abdominal transplant surgeons is concerning (12). Similarly, while there is wide variety in hepatology workflow and compensation, a burn out percent of 35% among trainees pursuing careers in transplant hepatology is alarming (13).
Effect of Race and Country of Origin on a Career in Liver Transplant
There is evidence to suggest that African American and Hispanic individuals are underrepresented in the field of medicine compared to their representation in the general population (14–16)1. For example, in the United States (US), African American and Hispanic individuals make up approximately 31% of the overall US population. Yet, the American Medical Association (AMA) reported in 2020, that approximately only 7% of all active physicians in the US identified as African American, and approximately 8% identified as Hispanic or Latino (14–16)1. On the other hand, among the surgical directors of LT programs, only 16% were Hispanic or African American (4). This disparity can be due to a range of factors, including social and economic disadvantages, lack of equitable access to educational and training opportunities compared to other groups, and discrimination. It is also possible that a person’s country of origin could impact their potential career in LT, depending on the availability of educational and training programs in that country and the existence of LT in the healthcare system. However, recent initiatives by multiple transplant societies to recognize transplant training of international graduates and offer them equal opportunity for training and certification processes would help to mitigate the disparities among international trainees. The impact of complete or relative lack of EDI in the field of LT can be quite consequential in hindering career development, limiting creativity and innovation among providers affected by this unfortunate reality. Therefore, it is important to recognize and address these issues to promote diversity and inclusion in the field of LT and ensure that individuals from all backgrounds have equal opportunities to enter and excel in this field for the betterment of LT as a specialty, us as a scientific community and importantly our patients.
Highlights of the ILTS Experience
In reviewing the ILTS data, over the last 5 years (2017–2022), the female participation rate was 25%–31%, highest years being 2021 and 2022 at 31%. For the 2022 conference, although 21% did not specify their field, female participation was 45% in hepatology, 44% anesthesia and critical care followed by 20% rate in surgery. With the leadership and society efforts, female moderator and female speaker rates went up gradually and annually from 20% to 37% and 21% and 36%, respectively, between 2017–2022 (Figures 2, 3). Similarly, gender distribution of accepted abstracts reached 30% in the last year (Figure 4). Given 30% of total female attendance to the entire conference, speaker and moderator rates of 30% is a clear demonstration of the equitable representation of female participants in ILTS meetings which should be taken as a role model for all professional societies. Regarding country representation, six countries (USA, China, Republic of Korea, Turkey, United Kingdom, and India) accounted for between 50% and 57% of the total attendance in the previous 5 years (2017–2022), which may be reflecting limited access from underdeveloped countries to international medical conferences. Obviously, size of the country and total number of transplant programs would directly impact the participation to meetings. Regardless, attendance from Africa or the rest of the Asian continent remained low relative to North America and Europe. This is one of the areas ILTS and EDI committee is currently working on. For instance, in 2020, ILTS conducted an educational outreach initiative to help develop educational activities focused on the needs of specific regions around the world. The initiative is called the ILTS Regional Expansion of Advanced Learning (REAL) project. The aim of this initiative is to reach out to the different regions, mainly underdeveloped areas, where LT education is much needed, via educational programs tailored to what the key opinion leaders expressed (in prior surveys) as topics or areas of needed learning in their regions. REAL Asia was launched in 2020, REAL Latin America in 2021 and more recently REAL Africa 2022; representing a good example of the collaboration between the educational committee and EDI committee to maximize inclusiveness in educational initiatives.
FIGURE 2
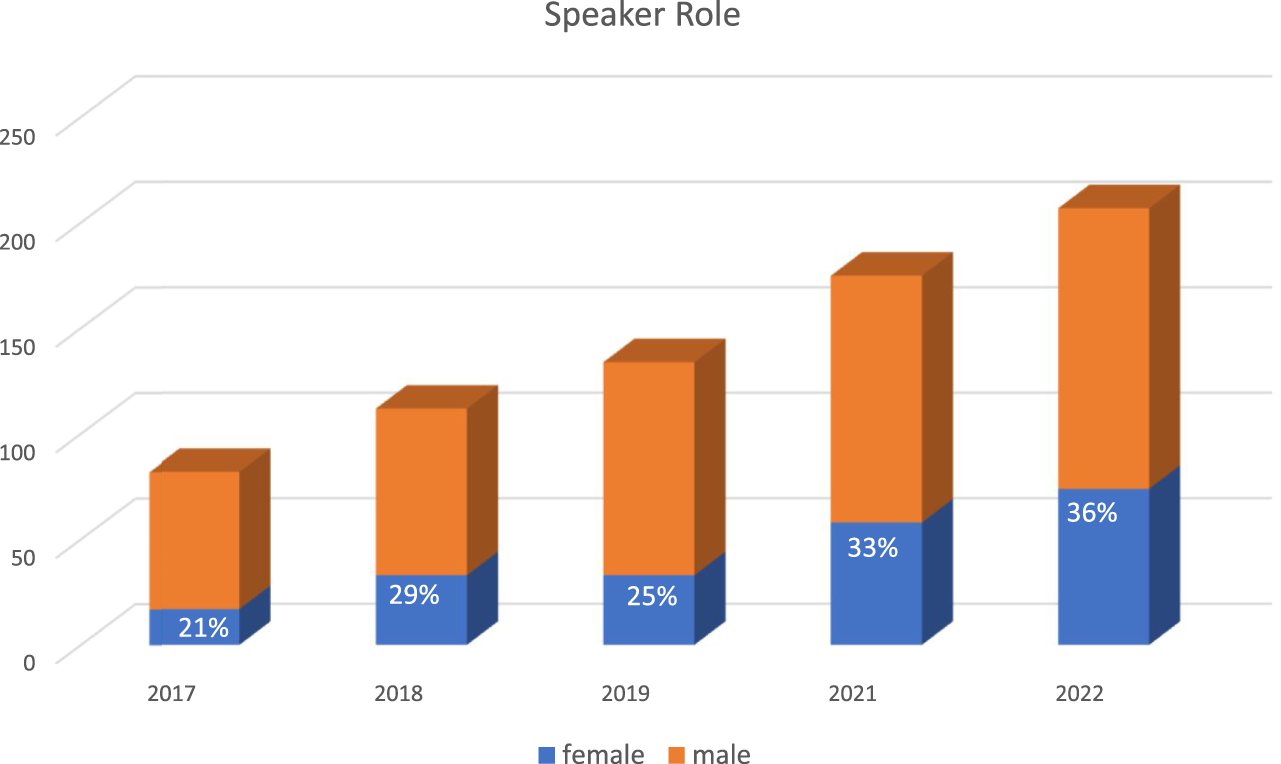
Gender Distribution of ILTS congresses speaker roles.
FIGURE 3
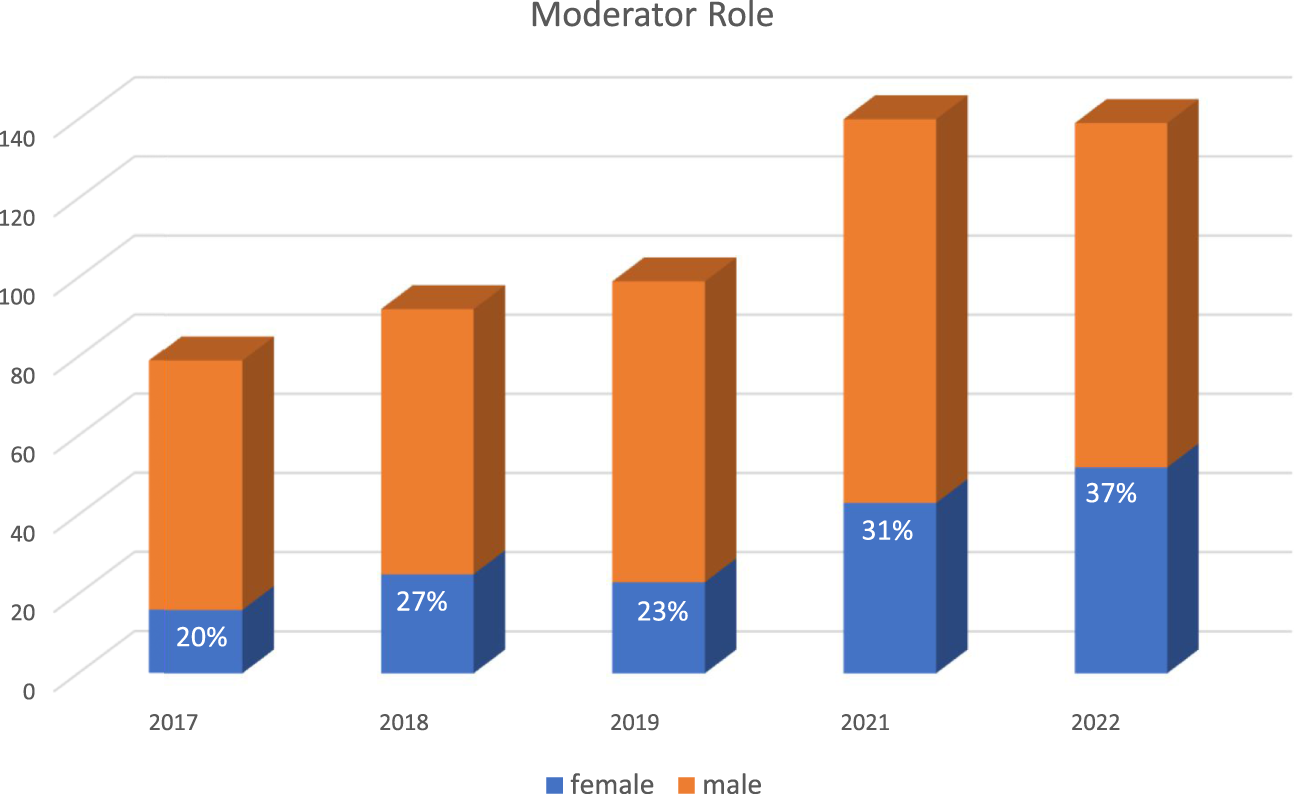
Gender Distribution of ILTS congresses moderator roles.
FIGURE 4
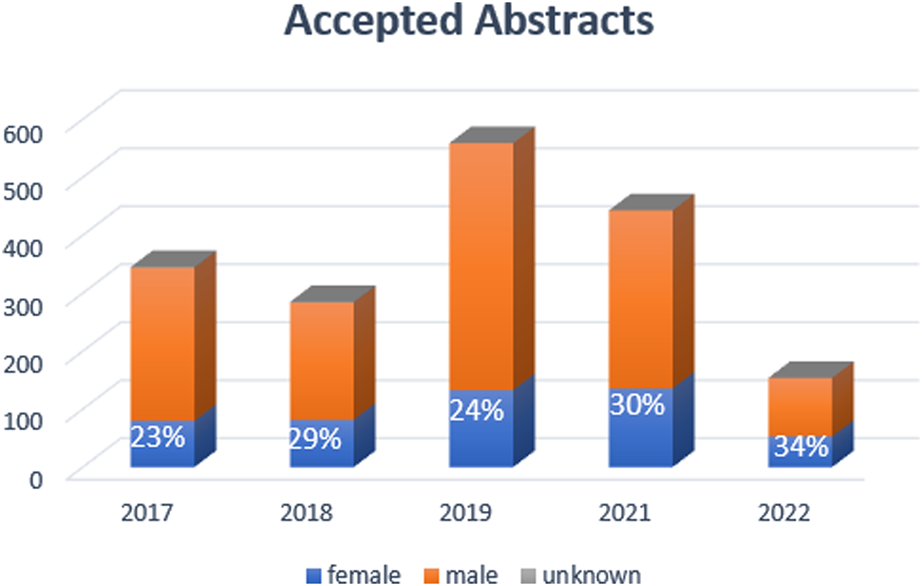
Gender Distribution of ILTS congresses accepted abstracts.
Representation of women participants can be augmented both by encouraging more female professionals to participate in scientific events as well as encouraging the professional societies to be more inclusive of women in organizing committees and nominating them for moderator or chairperson roles and encouraging male professionals to recognize the achievements made by women in this challenging field. It is not a question of gender but a question of having the same unbiased opportunities within the given field.
Strategies to Include Young Professionals in Transplant Societies
With increased representation of younger members in the field (17), they seem to be integrating into medical societies by creating subgroups or specific subcommittees in the various specialties. This can provide a good opportunity for younger members to establish their footprint as well as gain leadership skills. This would also serve to rejuvenate professional societies with new creative ideas. On the other hand, there needs to have mentors at the society level who can understand the expectations and needs of these of young members (18). ILTS founded the Young Investigators (YIs) subcommittee bringing together a variety of specialties that have expertise and training background in LT.
Online surveys have proven to be a tool used and appreciated by younger age groups (19). Despite several limitations in health epidemiology, they remain a valuable instrument for exploring trends (20). The role of online resources has become prominent in recent years and YIs rely upon online clinical resources in their practice (21). Even the use of social media has become very popular in the field of liver disease (22). In this respect, ILTS offers a wide range of online resources for its affiliates, stratified by macro-areas of interest (anesthesia, surgery, hepatology). Specifically, ILTS has promoted the Vanguard Committee. This committee’s mission is to promote the participation of younger members of the LT community in all ILTS activities, and to guide the society in responding to their educational and professional needs. Scopes of the committee include: to organize the part of the annual congress dedicated to YIs; to select the best published clinical and basic science research papers during the calendar year for the Vanguard Awards; to contribute to the Scientific Content in the monthly ILTS Newsletter; to assist in social media profile management and to lead monthly ILTS Vanguard Webinars on complex cases in LT.
Solutions to Mitigate Inequities and Maximize Inclusion Within the Transplant Community
Multiple medical professional societies have initiated programs to improve diversity, equity, and inclusiveness for physicians and allied health professionals in recent years. These ongoing efforts have been developed as disparities ranging from work compensation (23, 24), manuscript publication conference speaker representation, academic promotion, to leadership position have all been identified in the field of medicine (25–28). The heightened awareness on racial and gender disparities has urged professional societies to be the physicians’ voice and organize the physicians to unite in the front of combating discriminations. In the field of LT, ILTS is no exception on being a driving force to fight against disparities and inequities.
LT is a unique medical field that integrates various medical specialties, and ILTS serves as a unifying entity that encourages collaborations between these physicians from different countries all over the world. In 2017, the ILTS created the Equity, Diversity, and Inclusion Committee to promote equity, diversity, and inclusion in LT. Since 2017, the committee has been utilizing the DMAIC (Define, Measure, Analyze, Improve, Control) (28) approach of Six Sigma to overcome the complex tasks of finding impactful EDI initiatives to reduce disparities among women and other racial or gender minorities.
When issues were raised after gathering feedback from the ILTS members, the EDI Committee defined the opportunities for improvement. Once the focus of each EDI project was identified, granular data were gathered to provide measurements of the existing issue. Subsequently, the data were analyzed to understand the scope of the problem and to determine the root causes of the issue. From each EDI project, the data gave ILTS the insight on how to reduce disparities and improve diversity. Whenever an initiative was put forward, ILTS EDI Committee continued to monitor progress after each project implementation to ensure success and look for other routes to further increase project impact. The data obtained from the EDI committee initiatives resulted in series of recommendations aiming to mitigate gender and racial disparities in LT practices (Table 1).
TABLE 1
| 1. Acknowledge the existence of disparities at multiple levels |
| 2. Prioritize society membership recruitment towards underrepresented groups |
| 3. Modify the open-ended text field for members to accurately define their gender and ethnicity/race identity |
| 4. Ensure adequate representation of gender and racial minorities for society participation including committee appointments, leadership positions, conference session speakers |
| 5. Initiate mentorship programs, with focuses on trainees and junior physicians |
| 6. Continue to increase awareness on EDI topics at the international level and collaborate with local EDI committees |
| 7. Study disparities physician compensation |
| 8. Promote adequate parental leave policies |
| 9. Publish gathered data in international journals to increase visibility of EDI topics with recommendations on how to incorporate changes at local, national, and international levels |
| 10. Journals to promote more women and under-represented groups to be included in editorial boards |
Proposed international society initiatives to decrease disparities.
Conclusion
Significant disparities exist in the field of LT at multiple levels from leadership to training to societal representation. These disparities can have a remarkable impact on career development of the affected LT professionals. As ILTS and other international societies continue to provide initiatives, the support should be extended to local institutions aiming to mitigate inequities, strengthen the networking among underrepresented providers, and enhance optimal clinical practice, academic promotion, and leadership development in the field of LT.
Statements
Author contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
Funding
MB received grants from IISCarlos III (INT20/00061, PI19/01360). Ciberehd is partially funded by IISCarlos III.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
ILTS, International Liver Transplant Society; EDI, Equity, Diversity, and Inclusion; LT, Liver Transplantation; USA, United States of America; YIs, Young Investigators.
Footnotes
1.^US Census data. Explore Census Data: Learn about America’s People, Places, and Economy (2020). Available from: https://data.census.gov/ (Accessed December 15, 2022).
References
1.
Aguilera V Andacoglu O Francoz C Berlakovich G Pai SL Adelmann D et al Gender and Racial Disparity Among Liver Transplantation Professionals: Report of a Global Survey. Transpl Int (2022) 35:10506. 10.3389/ti.2022.10506
2.
Dwyer KM Clark CJ MacDonald K Paraskeva MA Rogers N Ryan J et al Gender Equity in Transplantation: A Report from the Women in Transplantation Workshop of the Transplantation Society of Australia and New Zealand. Transplantation (2017) 101:2266–70. 10.1097/TP.0000000000001900
3.
Giner R, Spanish Hepatologist Women Group GEMHEP. Spanish Hepatologist Women G. Spanish Women Hepatologists: Breaking the Glass Ceiling?Am J Gastroenterol (2018) 113:622–3. 10.1038/ajg.2018.32
4.
Choubey AP Bullock B Choubey AS Pai K Ortiz AC Khan SA et al Transplant Surgery Departmental Leaders Do Not Represent Workforce Demographics Especially Among Women and Underrepresented Minorities – A Retrospective Analysis. Am J Surg (2022) 224:153–9. 10.1016/j.amjsurg.2021.11.008
5.
Agawu A Fahl C Alexis D Diaz T Harris D Harris MC et al The Influence of Gender and Underrepresented Minority Status on Medical Student Ranking of Residency Programs. J Natl Med Assoc (2019) 111:665–73. 10.1016/j.jnma.2019.09.002
6.
de Rosner-van Rosmalen M Adelmann D Berlakovich GA Francoz C Selzner N Berenguer M et al Women Leadership in Liver Transplantation-Results of an International Survey. Transplantation (2022) 106:1699–702. 10.1097/TP.0000000000004034
7.
Jordan S Emamaullee J . Gender Equity in Surgical Literature Authorship: Are We There yet?Am J Surg (2022) 224:1215–6. 10.1016/j.amjsurg.2022.06.008
8.
Lim WH Quek J Tay PWL Ng CH Vathsala A Muthiah MD . Gender Distribution Among Transplant Journal Editorial Members: a Call to Empower Women in Academic Medicine. Transpl Int (2021) 34:2897–8. 10.1111/tri.14117
9.
Malik M Inam H Janjua MBN Martins RS Zahid N Khan S et al Factors Affecting Women Surgeons' Careers in Low-Middle-Income Countries: An International Survey. World J Surg (2021) 45(2):362–8. 10.1007/s00268-020-05811-9
10.
Kono E Isozumi U Nomura S Okoshi K Yamamoto H Miyata H et al Surgical Experience Disparity between Male and Female Surgeons in Japan. JAMA Surg (2022) 157(9):e222938. 10.1001/jamasurg.2022.2938
11.
Lucidi D Parini S Reale M Azzolina D Verdi D Spolverato G . Women in Surgery Italia: what Are the Opportunities in the Operatory Room? Results from a Nationwide Interdisciplinary Survey. Updates Surg (2022) 74(3):803–16. 10.1007/s13304-022-01304-7
12.
Delman AM Kassam AF Turner KM Ammann AM Lynch C Morris MC et al Incidence of Attrition Among Early-Career Abdominal Transplant Surgeons. Surgery (2022) S0039-6060(22):1113–9. 10.1016/j.surg.2022.08.017
13.
Kriss M Te HS Verna EC VanWagner LB Scott FI Lai JC . National Early Career Transplant Hepatologist Survey: Compensation, Burnout, and Job Satisfaction. Hepatol Commun (2021) 5(4):701–12. 10.1002/hep4.1666
14.
Association of American Medical Colleges. Physician Specialty Data Report (2023). Available from: https://www.aamc.org/data-reports/workforce/report/physician-specialty-data-report (Accessed January 31, 2023).
15.
Association of American Medical Colleges. Press Release: New AMA Policy Recognizes Racism as a Public Health Threat (2022). Available from: https://www.ama-assn.org/press-center/press-releases/new-ama-policy-recognizes-racism-public-health-threat (Accessed January 2023).
16.
Association of American Medical Colleges. Diversity in Medicine: Facts and Figures (2019). Available from: https://www.aamc.org/data-reports/workforce/report/diversity-medicine-facts-and-figures-2019 (Accessed January 31, 2023).
17.
Ianiro G Castro V Dolak W Ilie M Holleran G Salaga M et al The Organisation and Needs of Young Sections Belonging to UEG National Societies: Results of a Europe-wide Survey. United Eur Gastroenterol J (2017) 5:750–5. 10.1177/2050640617713936
18.
Skuja V Nakov R van Herwaarden Y Rodriguez-Lago I Acedo P Mikolasevic I et al How to Start a Young GI Section in Your Country: A Cookbook. United Eur Gastroenterol J (2020) 8:355–8. 10.1177/2050640620912635
19.
Greenlaw C Brown-Welty S . A Comparison of Web-Based and Paper-Based Survey Methods: Testing Assumptions of Survey Mode and Response Cost. Eval Rev (2009) 33:464–80. 10.1177/0193841X09340214
20.
Safdar N Abbo LM Knobloch MJ Seo SK . Research Methods in Healthcare Epidemiology: Survey and Qualitative Research. Infect Control Hosp Epidemiol (2016) 37:1272–7. 10.1017/ice.2016.171
21.
Chong HT Weightman MJ Sirichai P Jones A . How Do Junior Medical Officers Use Online Information Resources? A Survey. BMC Med Educ (2016) 16:120. 10.1186/s12909-016-0645-x
22.
Mikolajczyk AE Ufere N Breu AC Parikh ND Garcia-Tsao G Tapper EB . #LiverTwitter: An Emerging Tool for Liver Education and Research. Hepatol Commun (2020) 4:1229–33. 10.1002/hep4.1539
23.
Association of American Medical Colleges. Exploring Faculty Salary Equity at U.S. Medical Schools by Gender and Race/Ethnicity (2021). Available from: https://www.aamc.org/data-reports/workforce/report/exploring-faculty-salary-equity-us-medical-schools-gender-and-race/ethnicity (Accessed September 6, 2022).
24.
Hertzberg LB Miller TR Byerly S Rebello E Flood P Malinzak EB et al Gender Differences in Compensation in Anesthesiology in the United States: Results of a National Survey of Anesthesiologists. Anesth Analg (2021) 133(4):1009–18. 10.1213/ANE.0000000000005676
25.
Krstacic JE Carr BM Yaligar AR Kuruvilla AS Helali JS Saragossi J et al Academic Medicine’s Glass Ceiling: Author’s Gender in Top Three Medical Research Journals Impacts Probability of Future Publication success. PLoS One (2022) 17(4):e0261209. 10.1371/journal.pone.0261209
26.
Association of American Medical Colleges. Data & Report, Table F: Faculty by Gender, Rank, and Age Group, 2020 (Excel) (2020). Available from: https://www.aamc.org/media/54811/download (Accessed September 6, 2022).
27.
Pai SL . Top 10 Things Women Anesthesiologists Must Do for Academic Promotion. Int Anesthesiol Clin (2018) 56(3):96–109. 10.1097/AIA.0000000000000196
28.
American society for Quality. The Define, Measure, Analyze, Improve, Control (DMAIC) Process (2022). Available from: https://asq.org/quality-resources/dmaic (Accessed September 6, 2022).
Summary
Keywords
liver transplantation, equity, diversity, inclusion, professional societies
Citation
Andacoglu O, Izzy M, Adelmann D, Aguilera V, Becchetti C, Berenguer M, Berlakovich GA, Ghosh S, Giorgakis E, Kemmer N, Lunsford KE, Montasser IF, Montenovo MI, Mrzljak A, Pai S-L, Scalera I and Selzner N (2023) Addressing the Burden and Management Strategies for Disparities and Inequities Among Liver Transplant Professionals: The ILTS Experience. Transpl Int 36:11240. doi: 10.3389/ti.2023.11240
Received
31 January 2023
Accepted
14 April 2023
Published
02 June 2023
Volume
36 - 2023
Updates
Copyright
© 2023 Andacoglu, Izzy, Adelmann, Aguilera, Becchetti, Berenguer, Berlakovich, Ghosh, Giorgakis, Kemmer, Lunsford, Montasser, Montenovo, Mrzljak, Pai, Scalera and Selzner.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Oya Andacoglu, oya-andacoglu@ouhsc.edu; Manhal Izzy, manhal.izzy@vumc.org
†These authors share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.