Abstract
Patients from minoritized backgrounds based on race/ethnicity, gender, sexuality, and other social identities are more likely to experience inequities in access in kidney transplantation. Although these inequities have been reported over the decades, limited research focuses on the experiences of patients with intersecting minoritized social statuses and the mechanisms that contribute to their reduced access to transplantation. Intersectionality, a framework for understanding the ways in which multiple social identities represent interacting systems of oppression and privilege, offers a nuanced approach for understanding the experiences of patients diagnosed with end-stage organ disease with intersecting social identities. This article outlines complex systems that perpetuate inequities by highlighting the value of intersectionality in studying disparate outcomes to transplant and providing recommendations for the transplant community. This article aligns with the ESOT call for action to promote equity in transplantation worldwide.
Background
Global estimates for Chronic Kidney Disease (CKD) indicate that approximately 10% of the population have a known diagnosis, with diabetes mellitus and hypertension discovered as significant contributors to the development of this condition. This is particularly concerning given high mortality rates associated with the disease [1]. In the US in 2020, it was estimated that 807,920 people had End-Stage Kidney Disease (ESKD). The majority of patients used hemodialysis as their primary form of renal replacement therapy relative to peritoneal dialysis or transplantation [2]. Approximately 30,000 people in the UK were reported as receiving dialysis in 2023, with a yearly rate of 3,000 transplant recipients [3]. Inequities in access to renal transplantation, the optimal form of renal replacement therapy, have been documented for decades [4–8]. These imbalances have been associated with sociocultural factors such as gender, race/ethnicity, income status, and immigrant status. These elements of a patient’s identity often interact with biological and psychological factors resulting in barriers to accessing care [4, 9–13]. Hurdles occur along the steps to transplant, such as referral to transplant, pre-transplant evaluation, being waitlisted, and successful receipt of a deceased or live donor transplant [5, 14]. Insurance issues, financial constraints, limited health literacy, obesity, lack of referrals, reports of discrimination are examples of typical obstacles faced by patients diagnosed with ESKD who seek a transplant [5, 7, 13, 14]. Many patients encounter multiple barriers that interact with each other to affect their successful access to transplantation. This underscores the importance of identifying underlying mechanisms associated with inequities in access to transplantation. The objective of this viewpoint is to highlight complex systems that perpetuate these inequities, discuss the role of intersectionality in examining disparate outcomes to transplant, and provide recommendations to the transplant community. Table 1 provides a list of some key terms and definitions used in the article.
TABLE 1
| Term | Definition |
|---|---|
| Allostatic load | Cumulative long-term effects of exposure to chronic stress and its impact on an individual’s physical and psychological health |
| Cultural competence | The ability to understand, value, and respect people’s culture, customs, and belief systems as well as how they vary among individuals or groups |
| Cultural humility | An ongoing process and commitment to self-reflection of one’s beliefs and assumptions, and an openness to learning from others. It also entails a recognition of power differentials between individuals due to privilege and oppression |
| Cultural safety | Creating and cultivating an environment that values the cultural background and physical, social, and emotional safety of others. It involves an awareness of one’s personal culture and the ways in which this interacts with the culture of others |
| Cisgender | A person’s whose gender identity matches their sex assigned at birth. For example, an individual who was assigned female at birth and self-identifies and lives as a woman |
| Interpersonal racism | Discrimination or bias towards an individual based on their skin tone and/or hair texture. This form of racism occurs between individuals and can be intentional or unintentional |
| Implicit bias | Having negative beliefs or assumptions about a social group that one is not consciously aware of |
| Gender identity | One’s personal conception or sense of who they are in relation to their gender. Some people may self-identify as a man, woman, a combination of both, neither, or somewhere along the gender spectrum |
| Microaggressions | Daily verbal and nonverbal slights, insults, or invalidations that are intentional or unintentional and communicate prejudice towards a person from a specific social group. For example, refusing to call a transgender man by his preferred pronoun, him and instead insisting on using her |
| Personal pronouns | This is a way of referring to an individual without their actual name. Using the appropriate pronouns for an individual shows respect for their gender identity regardless of what your assumptions may be about them |
| Socioecological models of health | This model proposes that health is an interaction between multiple environments of an individual such as the person’s individual beliefs or personal characteristics (intrapersonal), exchanges with family, friends, and other support systems (interpersonal), organizations (e.g., health care systems, workplaces), and other systems. All of these different aspects of an individual’s social environment influence their health behaviors and outcomes |
| Structural racism | Societal expectations, laws, and systems that disadvantage or discriminate against certain racial/ethnic groups, thereby limiting their access to resources such as education, employment, healthcare, and housing |
| Transgender | A general term for individuals whose gender identity, expression, or behaviors are different from the prototype of the sex they were assigned at birth. For example, an individual who was assigned female at birth but self-identifies and lives as a man |
Key terms and definitions.
Sources of Inequities Along the Steps to Transplant
Multiple theories have been implicated in the quest to identify the causes of inequities in access to renal transplantation. Socioecological models account for the interaction between multiple aspects of the individual, for example, at the intrapersonal, interpersonal, institutional, and societal level to affect health outcomes [15, 16]. This model has been used to examine disparities along the steps to kidney transplantation [7, 17]. The role of social determinants of health (i.e., non-medical aspects of an individual’s life such as where they live, are raised, engage in recreational activities, and their vocation) has been established in the literature. Given that these determinants of health overlap with each other as well as biological, sociocultural and political factors, it is important that researchers interrogate these issues and the extent to which they contribute to health inequities.
Race
In the United States, the origin of many health inequities has been connected to race and racism. Purnell et al. [18] provide examples of the manifestation of racism in the transplant process, specifically for patients with African ancestry who identify as Black. For instance, institutional racism (i.e., implicit or explicit discriminatory practices within the field of transplantation) may be displayed in cultural differences in communication, resulting in provider perception of a patient as non-compliant or uninterested in pursuing transplantation [18]. Race-based modifications for estimating glomerular filtration rate (e-GFR) for Black patients is another example, especially as the removal of these practices indicate positive outcomes for reducing bias [19–21].
Gender
Transplant data indicates that women are underrepresented in referrals for transplant, more likely to be living donors, less likely to be recruited for clinical trials that investigate immunosuppression and rejection outcomes or receive a transplant [22–25]. Data from the United Network for Organ Sharing and Eurotransplant show disparate outcomes for waitlisting, with women being underrepresented on both kidney waitlists [9].
Socioeconomic Status
Socioeconomic status has been continuously documented as a barrier to transplant which may be symbolic of classism [4, 5]. Evidence of the role of classism may be especially prominent in countries with universal healthcare or when federally funded programs are offered to patients with ESKD as they continue to experience barriers [8, 26]. Acknowledging that these systems of oppression contribute to inequities in access to transplantation is the first step towards parity and should be an integral part of the work conducted within the transplant community.
The Importance of Identifying Underlying Mechanisms
An individual’s minoritized status based on race, gender, class, and/or sexuality among others has been connected to physiological and psychological outcomes. One’s social identity can be accompanied with stressors when this identity is disenfranchised in any form, preventing the individual from receiving social benefits afforded to others. As an example, people of European descent tend to have more social benefits and power relative people of African or Asian descent. Race-related stress, a consequence of one’s minoritized status has been connected to persistent occurrences of racism and microaggressions that tax the body’s stress response, resulting in an increase in allostatic load [27, 28]. This rise in allostatic load (refer to Table 1) is linked with a sequela of conditions such as hypertension, depression, and kidney dysfunction, in the absence of adaptive coping approaches to buffer against these stressors [27, 29, 30]. The minority stress model is another example of a theory that has been used to explain the ways in which one’s minoritized status affects their health outcomes. This theory postulates that stigma, prejudice, and discrimination foster stressful social environments for people with a minority status based on their race/ethnicity, gender, and sexuality. This can be compounded by socioeconomic stressors due to poverty, to produce poor mental health outcomes [31, 32]. Concerns about discrimination and risks for depression and anxiety have been documented among transgender and gender non-conforming individuals seeking pharmaceutical care, thereby affecting their health and treatment outcomes [33]. Given the evidence of racism, sexism, transphobia, and other systems of oppression in medicine and how they propagate inequities, ignoring these issues would be a severe disservice to patients with ESKD and other organ diseases.
Social justice initiatives provide a means for empowering transplant professionals and patients invested in health equity. This is in fact an essential part of health equity work if we are to tackle the underlying systems and structures behind these differences rather than proximal estimates such as race/ethnicity, sex, and income status [34]. As the world becomes more diverse through globalization and immigration, the field of transplantation has to evolve to recognize the value of diversity in science. The demographics in the US have changed significantly over the last few decades, a trend that is expected to continue, with more people identifying as Asian, Hispanic/Latine/x or multiracial [35]. Similar trends are apparent in the UK with an increase in the number of people who identify as Asian or Black [36]. Such changes in demographics are accompanied with a multitude of cultural experiences and practices as well as linguistic diversity which must be considered to practice good science [7, 37]. To better support patients, we cannot continue to use color-blind ideological approaches centered on Eurocentric, heteronormative (i.e., perception of heterosexuality as normal and standard), and cisnormative (refer to Table 1) values [37]. This necessitates an all-encompassing transplant science. Decreasing inequities in access to transplantation also comes with a global societal benefit. Diseases weaken an individual’s ability to showcase their talents and make innovative contributions to our society.
The Value of Intersectionality
A term generated by Kimberlé Crenshaw, intersectionality posits that multiple social identities such as race, gender, sexuality, and disability status can converge at the microlevel of an individual. This could be presented as interlacing systems of privilege and oppression, such as racism, sexism, homophobia, transphobia, classism, and ableism [38]. Bowleg [39] conveyed the significance of applying an intersectionality framework in public health, noting that research focused solely on women or racial/ethnic minorities disregards the intersection of both identities and does not cater to the multidimensional nature of the term, minority. Intersectionality is proposed as valuable for comprehending structural inequalities that pertain to racism, sexism, classism, and other structures to produce health inequities [40–42]. This framework allows researchers to understand the experiences of patients from minoritized groups from their vantage point and actual social realities [40].
Specific to the field of nephrology and transplantation, advocates for intersectionality highlight benefits for eradicating inequities for lesbian, gay, bisexual, transgender, and queer (LGBTQ+) individuals [42, 43]. Other studies have performed statistical analyses that investigate interactions between factors such as gender and race with no direct reference to employing an intersectionality framework. Findings revealed fewer living donor evaluations for Black women, while White and Latino/Hispanic men finalized their pre-transplant evaluation sooner than their women counterparts [44, 45]. Altogether, the literature signifies a paucity of research on intersectionality in transplantation. When intersectional analyses are conducted without implementing an intersectionality framework, these studies do not assess for roots causes of inequities (e.g., racism, sexism, classism) but instead focus on proxies such as race, gender, and income status. The implementation of an intersectionality framework to address health inequities in access to transplantation could provide a nuanced understanding of the experiences of certain groups. For example, published research in the US indicates that people who identify as Black experience more barriers in access to transplant with some associations to institutional racism. Other intersectional questions to consider include: how do the experiences of Black men and women differ? How does the ethnic background, immigration status, and income of a Black individual play a role in access to transplantation? Given the potential for scientific gains in addressing inequities along the steps to transplant, the transplant community is encouraged to be intentional about executing this framework in research and practice.
Recommendations for Research and Practice
One of the first steps in executing an intersectionality framework is to forgo the standardization of research on Eurocentric, cisgender, heterosexual men. Although we have made strides in improving the gender distribution of participants for clinical trials and other research methodologies, many of the surveys used in research are limiting [22]. The inclusion of simple demographical questions about ethnicity, sexuality, gender identity, and disability status could provide substantive information and facilitate intersectional analyses relative to focusing on race and sex. Moreover, most studies do not distinguish between biological sex (based on chromosomes and reproductive traits), and gender (socially constructed templates for men and women), making it harder to capture the experiences of people who do not subscribe to the gender binary or those who are intersex [9]. Race, a sociopolitical construct, is often used as an indicator for a biological construct even though genetic ancestry is a better measure. Racial differences in access to renal transplantation have been reported for decades yet little research has focused on varying forms of racism (e.g., interpersonal or institutional racism, microaggressions) accounting for some of these differences [18]. Of note, scholars are encouraged to be thoughtful in their use of social variables such as race and gender. Providing a rationale for using these variables and explicitly stating limitations (e.g., gender differences studied did not account for gender diverse individuals) as well as collecting data central to the research question, is useful for improving our scientific understanding of the role of social identities. This also reduces the exploitation of participants, especially when the questions contain personal and/or confidential information.
When examining intersections between aspects of a person’s identity, it is advisable to use measures that explore the root causes of these differences. The literature consists of a plethora of measures that assess constructs such as homophobia, racism, sexism, and transphobia. Sample measures with good psychometric properties include, The Gendered-Racial Microaggressions Scale for Black Women [46], the Lesbian, Gay, Bisexual, and Transgender People of Color Microaggressions Scale [47], The Expectations of Racism Scale [48–50], Everyday Discrimination Scale [51], The Neosexism Scale [52], and Attitudes toward Transgender Men and Women [53]. Studies aimed at exploring the role of these underlying mechanisms can make use of such measures. Many of the measures have already been validated in health populations, including patients with CKD [29, 54, 55]. Understudied areas such as the role of ableism, ageism, and xenophobia warrant more attention and may offer a wider range of understanding of the complexities associated with a patient’s multiple social statuses. Thom et al. [56] suggest that inequities may be apparent for patients with impaired decision-making (e.g., intellectual disability, cognitive impairment due to a condition) pursuing transplant.
Qualitative and quantitative guidelines for implementing an intersectionality framework such as an investigation of power and inequality already exist in the literature [57–59]. In many cases, a combination of both methodologies (i.e., a mixed-methods approach) could provide a deeper understanding of a research question [60]. Intersectionality workshops are also available via the Intersectionality Training Institute.
Strength-based approaches focused on the patient’s strengths and abilities instead of deficiencies can be extremely beneficial. These approaches offer an opportunity for providers to learn from their patients who are the experts of their experiences about the strategies already implemented to navigate the barriers they face. This can also be empowering for patients as they are able to contribute to social justice initiatives related to their health. Community-based participatory research and qualitative research designs are examples of research methodologies that enable patients’ role as co-creators of scientific knowledge. Targeted research questions and interventions (e.g., an intervention focused on Asian immigrant women) will also facilitate in-depth examination of an inequity for a specific group with intersecting identities. Scholars interested in implementing intersectionality in their work should dedicate the time to develop the appropriate proficiency for conducting this work and/or collaborate with other researchers that are already undertaking this work. Diverse research teams with members who possess the minoritized statuses being studied can reduce the potential for enacting additional harms and promote quality research [34]. Awareness of the appropriate terminology such as cisgender versus transgender, personal pronouns, and phrases that may be reflective of microaggressions is crucial to prevent harms on groups that already experience social oppression. Cultivating diverse research teams also promotes social justice given that people from minoritized backgrounds have been reported to receive less extramural funding to support their work in comparison to those from more privileged backgrounds [34]. Interdisciplinary work with professionals from backgrounds such as social work, psychology, and sociology would also strengthen the transplant community’s efforts towards health equity. Figure 1 provides a graphical representation of the different recommendations for research.
FIGURE 1
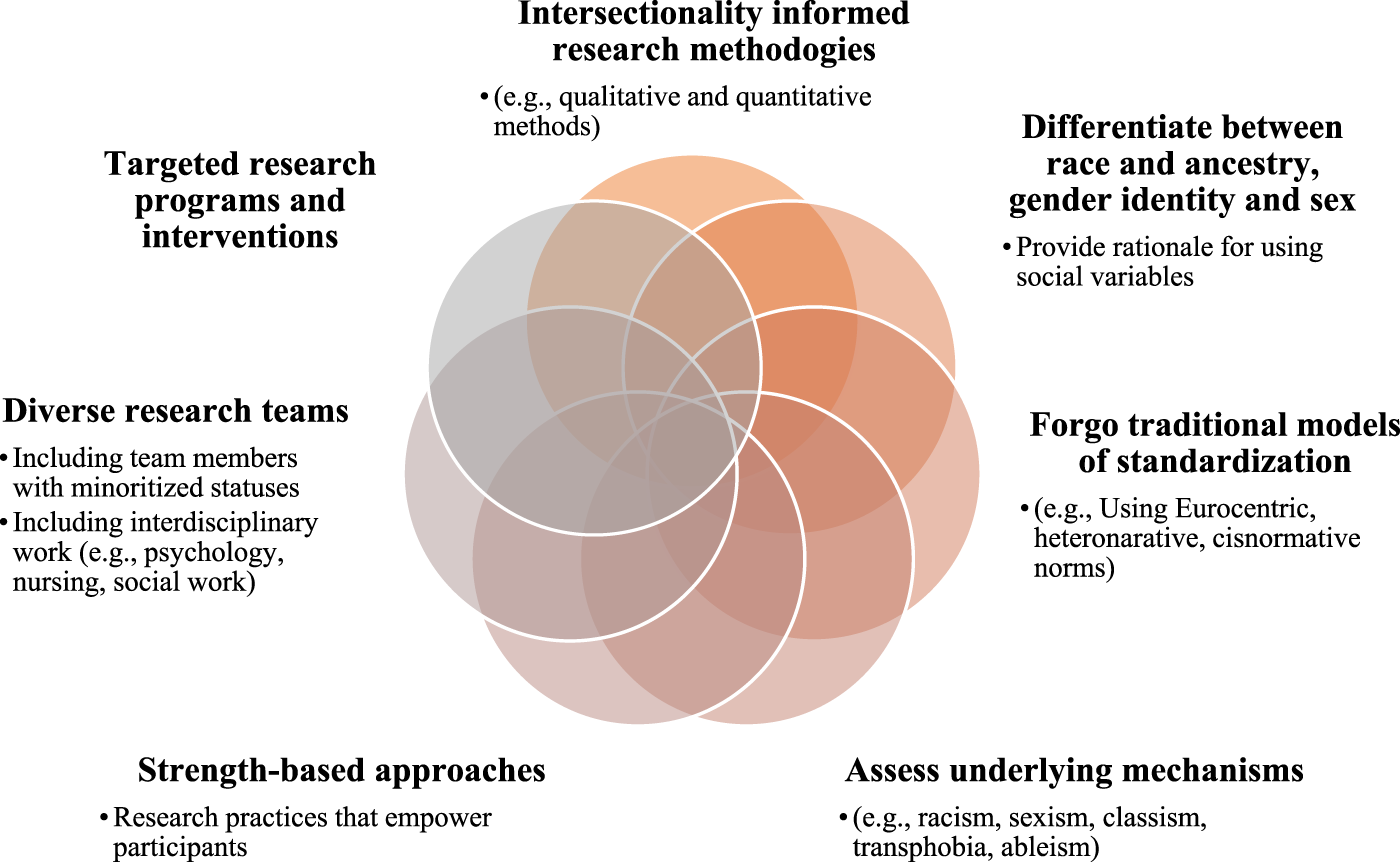
Recommendations for incorporating intersectionality in research.
Specific to practice, curricula changes are needed to promote a more nuanced understanding of the role of intersectionality in patient care. This includes basic knowledge of the intersectionality framework, and instruction that incorporates clinical case studies with patients with intersecting identities, caution should be taken to ensure that these clinical cases do not perpetuate stereotypes but instead allow trainees to engage in critical thinking about the ways in which systems of oppression disenfranchise certain groups. Sabik [61] developed an intersectionality toolkit for public health education which can be tailed to nephrology populations for pedagogical purposes. To get to the root causes of inequities in transplantation, we cannot focus solely on implicit or unconscious bias training or diversity and inclusion initiatives as many of them fail to empower individuals with the necessary tools to combat bias and oppression [62]. Effective trainings use proactive approaches that empower individuals to identify and dismantle systems that allow injustices to persist. The most efficacious trainings comprehend the value of prioritizing the concerns of the most disenfranchised groups, in addition to cultivating environments that promote safety and belonging [62].
Another aspect of practicing intersectionality is basic knowledge of the sociocultural components of social groups and identities, combined with self-reflection. Some of the terms used to describe this process include cultural competence, cultural humility, and cultural safety [63]. Cultural competence and cultural humility are commonly used within the U.S. whereas cultural safety is typically used in New Zealand, Australia, and Canada [63]. The transplant community is encouraged to consider keys elements of these concepts in their application of any form of culturally relevant care. First, healthcare professionals should cater to the sociocultural needs of the patient group, part of which requires education about the group(s). Second, providers must engage in reflective exercises that entail learning new information and unlearning previously held knowledge, confronting and challenging personal biases and worldviews as well as the ways in which they may conflict or align with other worldviews or experiences. Third, awareness of power structures and differentials that may interfere with the patient-provider relationship and recognition of the ways in which colonization, racism, sexism, and other forms of discrimination contribute to health inequities. Finally, to truly invest in health equity, transplant professionals must recognize that patients are the experts of their own experiences. Therefore, providers should be transparent about their limitations in knowledge and devote themselves to a lifetime of learning [63, 64].
Another extension of administering intersectionality is by expanding the workforce with providers whose identities match those of their patients [65]. This is often the first step in decreasing medical mistrust and fears of discrimination among patients with intersecting minoritized identities. Diversity in transplant personnel improves our aptitude for offering culturally relevant interventions given the personal and professional expertise of these providers. Many associations within the field of transplant such as the American Society of Transplantation (AST) and the European Society for Organ Transplantation (ESOT) have already established a range of diversity initiatives. These include objectives focused on increasing the number of professionals from underrepresented groups and eliminating systemic racism. Other actionable steps could entail advocating for policy changes that mandate medical facilities to report on the demographics of their staff relative to that of their patient populations. Hospitals with complimentary statistics can be incentivized whereas those with little to no diversity can be educated on the significance of enhancing diversity within their institution, including specific instruction on intersectionality. Additionally, healthcare facilities with gaps in diversity could be required to cultivate, for example, a 5-year plan to improve their statistics. As part of their advocacy for policy changes, organizations like the ESOT and AST can outline the multiple health and social benefits of enhanced diversity, including increased revenue and innovation for healthcare systems [66].
Practical efforts towards health equity through an intersectional lens include institutional changes. Examples comprise but are not limited to inclusive in-take forms that account for the reporting of multiple forms of social identities and improved e-GFR guidelines for transgender and gender diverse ESKD patients who have undergone gender affirming hormone therapy. Finally, allyship, is an essential part of health equity and comprises practices and actions undertaken by people with privilege as they advocate for those who are susceptible to systems of oppression. Key tenets of authentic allyship require openness to criticism and constructive feedback, humility, advocacy, and consciousness of one’s power. An essential component of authentic allyship is the amplify the voices of people with marginalized identities without taking up space from those same voices [67]. See Figure 2 for a pictorial view of these recommendations.
FIGURE 2
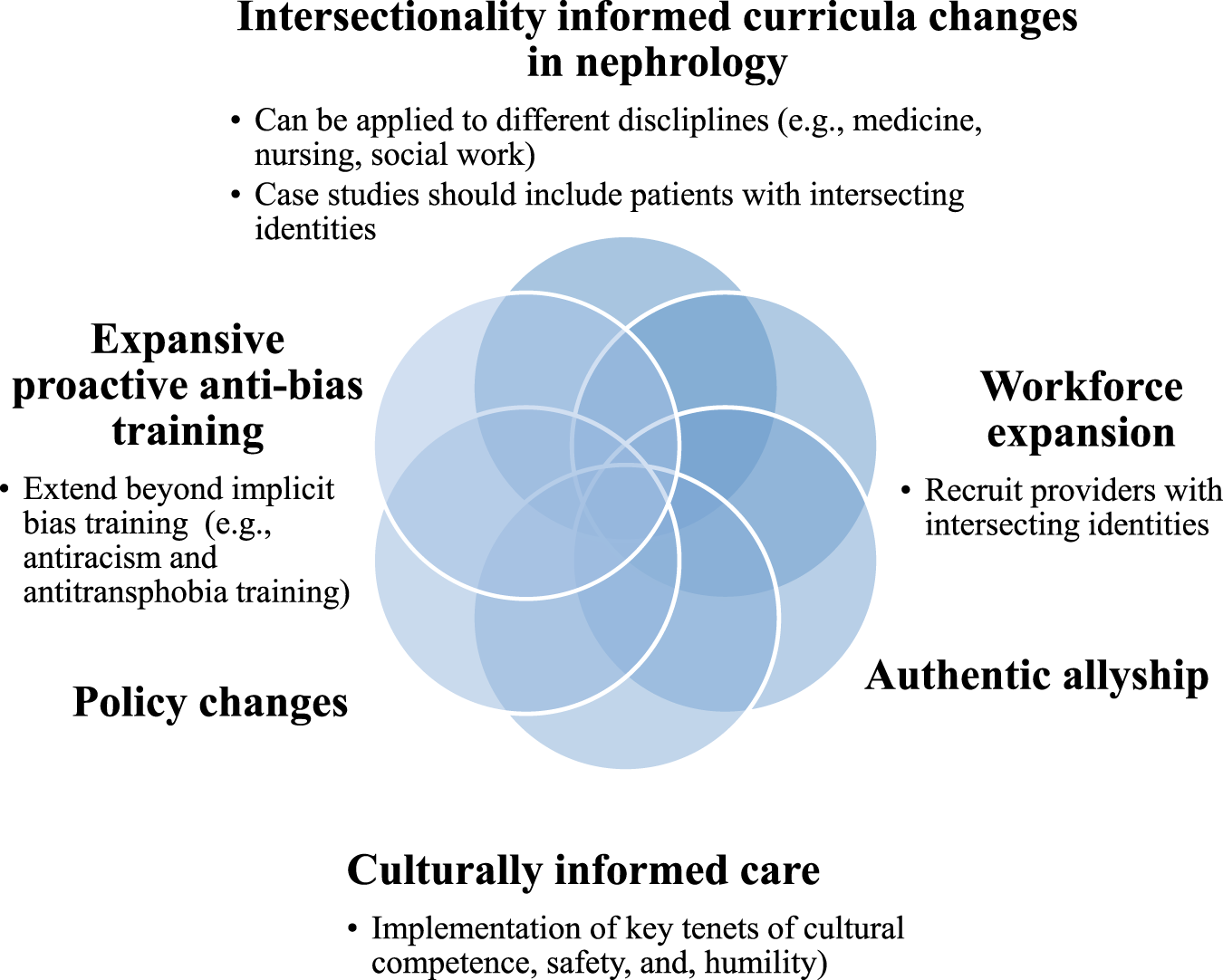
Recommendations for incorporating intersectionality in practice.
Conclusion
Intersectionality offers a valuable opportunity for the transplant community to make advancements towards parity in access to kidney transplantation. It requires multifaceted approaches and dedicated transplant professionals invested in improving outcomes for all patients.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
CN conceptualized and wrote the manuscript.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1.
Kovesdy CP . Epidemiology of Chronic Kidney Disease: An Update 2022. Kidney Int Suppl (2022) 12(1):7–11. 10.1016/j.kisu.2021.11.003
2.
United States Renal Data System. USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (2022). Available From: https://usrds-adr.niddk.nih.gov/202 (Accessed May 28, 2023).
3.
Kidney Research UK. The Health Economics of Kidney Disease to 2033 (2023). Available From: https://www.kidneyresearchuk.org/wp-content/uploads/2023/06/Economics-of-Kidney-Disease-full-report_accessible.pdf (Accessed August 23, 2023).
4.
Elrggal ME Gokcay Bek S Shendi AM Tannor EK Nlandu YM Gaipov A . Disparities in Access to Kidney Transplantation in Developing Countries. Transplantation (2021) 105(11):2325–9. 10.1097/TP.0000000000003585
5.
Harding JL Perez A Snow K Retzloff S Urbanski M White MS et al Non-Medical Barriers in Access to Early Steps of Kidney Transplantation in the United States – A Scoping Review. Transplant Rev (Orlando) (2021) 35(4):100654. 10.1016/j.trre.2021.100654
6.
Udayaraj U Ben-Shlomo Y Roderick P Casula A Dudley C Johnson R et al Social Deprivation, Ethnicity, and Access to the Deceased Donor Kidney Transplant Waiting List in England and Wales. Transplantation (2010) 90(3):279–85. 10.1097/TP.0b013e3181e346e3
7.
Grossi AA Ouoti F Masiero L Troni A Cianchi T Maggiore U et al Inequities in Organ Donation and Transplantation Among Immigrant Populations in Italy: A Narrative Review of Evidence, Gaps in Research and Potential Areas for Intervention. Transpl Int (2023) 36:11216. 10.3389/ti.2023.11216
8.
Boulware LE Ephraim PL Ameling J Lewis-Boyer L Rabb H Greer RC et al Effectiveness of Informational Decision Aids and a Live Donor Financial Assistance Program on Pursuit of Live Kidney Transplants in African American Hemodialysis Patients. BMC Nephrol (2018) 19(1):107. 10.1186/s12882-018-0901-x
9.
Melk A Babitsch B Borchert-Mörlins B Claas F Dipchand AI Eifert S et al Equally Interchangeable? How Sex and Gender Affect Transplantation. Transplantation (2019) 103(6):1094–110. 10.1097/TP.0000000000002655
10.
Nonterah CW Gardiner HM . Pre-Transplant Evaluation Completion for Black/African American Renal Patients: Two Theoretical Frameworks. Patient Educ Couns (2020) 103(5):988–98. 10.1016/j.pec.2019.11.005
11.
Ramadan OI Naji A Levine MH Porrett PM Dunn TB Nazarian SM et al Kidney Transplantation and Donation in the Transgender Population: A Single-Institution Case Series. Am J Transpl (2020) 20(10):2899–904. 10.1111/ajt.15963
12.
Sheikh SS Locke JE . Gender Disparities in Transplantation. Curr Opin Organ Transpl (2021) 26(5):513–20. 10.1097/MOT.0000000000000909
13.
Sullivan C Leon JB Sayre SS Marbury M Ivers M Pencak JA et al Impact of Navigators on Completion of Steps in the Kidney Transplant Process: A Randomized, Controlled Trial. Clin J Am Soc Nephrol (2012) 7(10):1639–45. 10.2215/CJN.11731111
14.
Nonterah CW Utsey SO Gupta G Wilkins S Gardiner HM . A Nominal Group Technique Study of Patients Who Identify as Black or African American and Access to Renal Transplantation. Prog Transpl (2023) 33(2):141–9. 10.1177/15269248231164164
15.
McLeroy KR Steckler A Bibeau D Glanz K . An Ecological Perspective on Health Promotion Programs. Health Educ Q (1988) 15(4):351–77. 10.1177/109019818801500401
16.
Stokols D . Translating Social Ecological Theory Into Guidelines for Community Health Promotion. Am J Health Promot (1996) 10(4):282–98. 10.4278/0890-1171-10.4.282
17.
Waterman AD Rodrigue JR Purnell TS Ladin K Boulware LE . Addressing Racial and Ethnic Disparities in Live Donor Kidney Transplantation: Priorities for Research and Intervention. Semin Nephrol (2010) 30(1):90–8. 10.1016/j.semnephrol.2009.10.010
18.
Purnell TS Simpson DC Callender CO Boulware LE . Dismantling Structural Racism as a Root Cause of Racial Disparities in COVID-19 and Transplantation. Am J Transpl (2021) 21(7):2327–32. 10.1111/ajt.16543
19.
Bellini MI Nozdrin M Naesens M Martins PN . Eliminating Race From eGFR Calculations: Impact on Living Donor Programs. Transpl Int (2022) 35:10787. 10.3389/ti.2022.10787
20.
Boulware LE Mohottige D Maciejewski ML . Race-Free Estimation of Kidney Function: Clearing the Path Toward Kidney Health Equity. JAMA (2022) 327(23):2289–91. 10.1001/jama.2022.7310
21.
Umeukeje EM Koonce TY Kusnoor SV Ulasi II Kostelanetz S Williams AM et al Systematic Review of International Studies Evaluating MDRD and CKD-EPI Estimated Glomerular Filtration Rate (eGFR) Equations in Black Adults. PLoS One (2022) 17(10):e0276252. 10.1371/journal.pone.0276252
22.
Park C Jones MM Kaplan S Koller FL Wilder JM Boulware LE et al A Scoping Review of Inequities in Access to Organ Transplant in the United States. Int J Equity Health (2022) 21(1):22. 10.1186/s12939-021-01616-x
23.
Ross LF Thistlethwaite JR . Gender and Race/Ethnicity Differences in Living Kidney Donor Demographics: Preference or Disparity?Transplant Rev (Orlando) (2021) 35(3):100614. 10.1016/j.trre.2021.100614
24.
Rota-Musoll L Brigidi S Molina-Robles E Oriol-Vila E Perez-Oller L Subirana-Casacuberta M . An Intersectional Gender Analysis in Kidney Transplantation: Women Who Donate a Kidney. BMC Nephrol (2021) 22(1):59. 10.1186/s12882-021-02262-9
25.
Vinson AJ Ahmed SB . Representation of Women in Contemporary Kidney Transplant Trials. Transpl Int (2023) 36:11206. 10.3389/ti.2023.11206
26.
Bailey PK Caskey FJ MacNeill S Tomson CRV Dor FJMF Ben-Shlomo Y . Mediators of Socioeconomic Inequity in Living-Donor Kidney Transplantation: Results From a UK Multicenter Case-Control Study. Transplant Direct (2020) 6(4):e540. 10.1097/TXD.0000000000000986
27.
Clark R Anderson NB Clark VR Williams DR . Racism as a Stressor for African Americans. A Biopsychosocial Model. Am Psychol (1999) 54(10):805–16. 10.1037//0003-066x.54.10.805
28.
Harrell SP . A Multidimensional Conceptualization of Racism-Related Stress: Implications for the Well-Being of People of Color. Am J Orthopsychiatry (2000) 70(1):42–57. 10.1037/h0087722
29.
Arriola KJ Lewis TT Pearce B Cobb J Weldon B Valentin MIZ et al A Randomized Trial of Race-Related Stress Among African Americans With Chronic Kidney Disease. Psychoneuroendocrinology (2021) 131:105339. 10.1016/j.psyneuen.2021.105339
30.
Cobb RJ Thorpe RJ Norris KC . Everyday Discrimination and Kidney Function Among Older Adults: Evidence From the Health and Retirement Study. J Gerontol A Biol Sci Med Sci (2020) 75(3):517–21. 10.1093/gerona/glz294
31.
Brooks VR . Minority Stress and Lesbian Women. MA: Lexington Books (1981).
32.
Meyer IH . Prejudice, Social Stress, and Mental Health in Lesbian, Gay, and Bisexual Populations: Conceptual Issues and Research Evidence. Psychol Bull (2003) 129(5):674–97. 10.1037/0033-2909.129.5.674
33.
Lewis NJW Batra P Misiolek BA Rockafellow S Tupper C . Transgender/Gender Nonconforming Adults’ Worries and Coping Actions Related to Discrimination: Relevance to Pharmacist Care. Am J Health Syst Pharm (2019) 76(8):512–20. 10.1093/ajhp/zxz023
34.
Kelly C Dansereau L Sebring J Aubrecht K FitzGerald M Lee Y et al Intersectionality, Health Equity, and EDI: What's the Difference for Health Researchers? Int J Equity Health (2022) 21(1):182. 10.1186/s12939-022-01795-1
35.
Jones N Marks R Ramirez R Rios-Vargas M . 2020 Census Illuminates Racial and Ethnic Composition of the Country. United States: United States Census Bureau (2021). Available at: https://www.census.gov/library/stories/2021/08/improved-race-ethnicity-measures-reveal-united-states-population-much-more-multiracial.html (Accessed May 28, 2023).
36.
Office for National Statistics (ONS). Ethnic Group, England and Wales: Census 2021 (2022). Available From: https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity/bulletins/ethnicgroupenglandandwales/census2021 (Accessed May 28, 2023).
37.
Plaut VC . Diversity Science: Why and How Difference Makes a Difference. Psychol Inq (2010) 21(2):77–99. 10.1080/10478401003676501
38.
Crenshaw K . Demarginalizing the Intersection of Race and Sex: A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory and Antiracist Politics. Univ Chicago Leg Forum (1989) 1(8).
39.
Bowleg L . The Problem With the Phrase Women and Minorities: Intersectionality-An Important Theoretical Framework for Public Health. Am J Public Health (2012) 102(7):1267–73. 10.2105/AJPH.2012.300750
40.
Bowleg L . We're Not All in This Together: On COVID-19, Intersectionality, and Structural Inequality. Am J Public Health (2020) 110(7):917. 10.2105/AJPH.2020.305766
41.
Heard E Fitzgerald L Wigginton B Mutch A . Applying Intersectionality Theory in Health Promotion Research and Practice. Health Promot Int (2020) 35(4):866–76. 10.1093/heapro/daz080
42.
Lett E Logie CH Mohottige D . Intersectionality as a Lens for Achieving Kidney Health Justice. Nat Rev Nephrol (2023) 19(6):353–4. 10.1038/s41581-023-00715-y
43.
Mohottige D Lunn MR . Advancing Equity in Nephrology: Enhancing Care for LGBTQ+ Patients and Our Workforce. Clin J Am Soc Nephrol (2019) 14(7):1094–6. 10.2215/CJN.01950219
44.
Gillespie A Hammer H Kolenikov S Polychronopoulou A Ouzienko V Obradovic Z et al Sex Differences and Attitudes Toward Living Donor Kidney Transplantation Among Urban Black Patients on Hemodialysis. Clin J Am Soc Nephrol (2014) 9(10):1764–72. 10.2215/CJN.12531213
45.
Monson RS Kemerley P Walczak D Benedetti E Oberholzer J Danielson KK . Disparities in Completion Rates of the Medical Prerenal Transplant Evaluation by Race or Ethnicity and Gender. Transplantation (2015) 99(1):236–42. 10.1097/TP.0000000000000271
46.
Lewis JA Neville HA . Construction and Initial Validation of the Gendered Racial Microaggressions Scale for Black Women. J Couns Psychol (2015) 62(2):289–302. 10.1037/cou0000062
47.
Balsam KF Molina Y Beadnell B Simoni J Walters K . Measuring Multiple Minority Stress: The LGBT People of Color Microaggressions Scale. Cultur Divers Ethnic Minor Psychol (2011) 17(2):163–74. 10.1037/a0023244
48.
Benkert R Peters RM Clark R Keves-Foster K . Effects of Perceived Racism, Cultural Mistrust and Trust in Providers on Satisfaction With Care. J Natl Med Assoc (2006) 98(9):1532–40.
49.
Lewis TT Lampert R Charles D Katsz S . Expectations of Racism and Carotid Intima-Media Thickness in African American Women. Psychosom Med (2019) 81:759–68. 10.1097/PSY.0000000000000684
50.
Mendoza-Denton R Downey G Purdie VJ Davis A Pietrzak J . Sensitivity to Status-Based Rejection: Implications for African American Students' College Experience. J Pers Soc Psychol (2002) 83(4):896–918. 10.1037//0022-3514.83.4.896
51.
Williams DR Yu Y Jackson JS Anderson NB . Racial Differences in Physical and Mental Health: Socioeconomic Status, Stress, and Discrimination. J Health Psychol (1997) 2(3):335–51. 10.1177/135910539700200305
52.
Tougas F Brown R Beaton AM Joly S . Neosexism: Plus Ça Change, Plus C'est Pareil. Pers Soc Psychol Bull (1995) 21(8):842–9. 10.1177/0146167295218007
53.
Billard TJ . Attitudes Toward Transgender Men and Women: Development and Validation of a New Measure. Front Psychol (2018) 9:387. 10.3389/fpsyg.2018.00387
54.
Dale SK Nelson CM Wright IA Etienne K Lazarus K Gardner N et al Structural Equation Model of Intersectional Microaggressions, Discrimination, Resilience, and Mental Health Among Black Women With HIV. Health Psychol (2023) 42(5):299–313. 10.1037/hea0001275
55.
Hamoda RE McPherson LJ Lipford K Jacob Arriola K Plantinga L Gander JC et al Association of Sociocultural Factors With Initiation of the Kidney Transplant Evaluation Process. Am J Transpl (2020) 20(1):190–203. 10.1111/ajt.15526
56.
Thom RL Dalle-Ave A Bunnik EM Krones T Assche KV Ruck Keene A et al Inequitable Access to Transplants: Adults With Impaired Decision-Making Capacity. Transplantation (2022) 106(9S):10084–S92. 10.3389/ti.2022.10084
57.
Bowleg L Bauer G . Invited Reflection: Quantifying Intersectionality. Psychol Women Q (2016) 40(3):337–41. 10.1177/0361684316654282
58.
Else-Quest NM Hyde JS . Intersectionality in Quantitative Psychological Research: I. Theoretical and Epistemological Issues. Psychol Women Q (2016) 40(2):155–70. 10.1177/0361684316629797
59.
Kelly C Kasperavicius D Duncan D Etherington C Giangregorio L Presseau J et al ‘Doing’ or ‘Using’ Intersectionality? Opportunities and Challenges in Incorporating Intersectionality Into Knowledge Translation Theory and Practice. Int J Equity Health (2021) 20(1):187. 10.1186/s12939-021-01509-z
60.
Watson-Singleton NN Lewis JA Dworkin ER . Toward a Socially Just Diversity Science: Using Intersectional Mixed Methods Research to Center Multiply Marginalized Black, Indigenous, and People of Color (BIPOC). Cultur Divers Ethnic Minor Psychol (2023) 29(1):34–42. 10.1037/cdp0000477
61.
Sabik NJ . The Intersectionality Toolbox: A Resource for Teaching and Applying an Intersectional Lens in Public Health. Front Public Health (2021) 9:772301. 10.3389/fpubh.2021.772301
62.
Asare JG . What People Misunderstand About Anti-Racism Training. New Jersey, U.S: Forbes (2022). Available at: https://www.forbes.com/sites/janicegassam/2022/01/04/what-people-misunderstand-about-anti-racism-training/?sh=771ab29243b5 (Accessed May 28, 2023).
63.
Thompson PB Taylor K . A Cultural Safety Approach to Health Psychology. Palgrave Macmillan Cham (2021). Available at: https://link.springer.com/10.1007/978-3-030-76849-2 (Accessed May 28, 2023).
64.
Tervalon M Murray-García J . Cultural Humility Versus Cultural Competence: A Critical Distinction in Defining Physician Training Outcomes in Multicultural Education. J Health Care Poor Underserved (1998) 9(2):117–25. 10.1353/hpu.2010.0233
65.
Butler T Cummings LS Purnell TS . The Case for Prioritizing Diversity in the Transplantation Workforce to Advance Kidney Health Equity. J Am Soc Nephrol (2022) 33(10):1817–9. 10.1681/ASN.2022040429
66.
Gomez LE Bernet P . Diversity Improves Performance and Outcomes. J Natl Med Assoc (2019) 111(4):383–92. 10.1016/j.jnma.2019.01.006
67.
Nonterah CW . Making Space When Black Voices Speak Their Truth. In: SmallCFullerMF, editors. Anti-Blackness, White Privilege and Authentic Allyship. New York: Oxford University Press (2024).
Summary
Keywords
intersectionality, inequities, transplant access, kidney transplant, health disparities
Citation
Nonterah CW (2024) Systems Connected to Inequities in Access to Kidney Transplantation and the Value of Intersectionality. Transpl Int 37:11658. doi: 10.3389/ti.2024.11658
Received
07 June 2023
Accepted
10 January 2024
Published
26 January 2024
Volume
37 - 2024
Updates
Copyright
© 2024 Nonterah.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Camilla W. Nonterah, cnontera@richmond.edu
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.