Gianluigi Zaza
Department of Pharmacy, Health and Nutritional Sciences, University of Calabria
Arcavacata di Rende, Italy
Submission closed
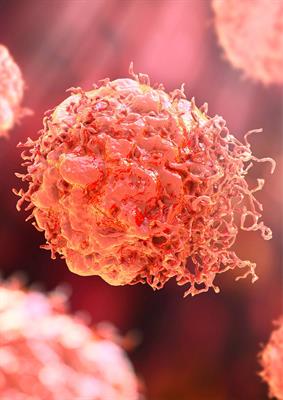
Solid organ transplantation provides life-saving therapy for patients with end-stage organ disease, but, unfortunately, it may be associated with several comorbidities including cancers most of them viral-induced (as non-Hodgkin lymphoma and Hodgkin lymphoma, Kaposi sarcoma, anogenital human papilloma, hepatitis C and B viruses-related liver cancer, non-melanoma skin cancers, prostate and thyroid neoplasia). Different conditions may facilitate the onset/development of these post-transplant malignancies (both viral- and non-viral associated) and several strategies are becoming rapidly available to early diagnose and treat these conditions.
However, a duty of primary importance of transplant medicine is still to minimize the risk of donor-transfer of cancer. In fact, solid organ transplantation carries an inevitable risk of transmission of malignant diseases, and this risk may be enhanced when organs from donors with a history of or ongoing malignancy are recovered. As well, donors are becoming older and this increases the risk of hidden malignancy. Although the low incidence of cancer transmission in many recipients from donors with a history of or ongoing malignancy, there is still some concern regarding the use of such donors because of high morbidity/mortality in recipients in cases of transmission. The transmission of donor-derived malignancy also occurs from donors with no history of malignancy; consequently, vigilance during donor assessment is mandatory. International guidelines, recommendations, and updated data are necessary to provide insight into the factors mainly involved in the risk of transmission of malignancies from donor to recipient.
Additionally, the overall risk of post-transplant cancer is associated with the type of transplant, underlying medical comorbidities, end-stage organ diseases, and, particularly, the use of long-term immunosuppressive therapies. Epidemiological data reveal that the length of exposure to immunosuppressive therapy and the strength of therapy are clearly correlated to the post-transplant risk of malignancy, and that when cancer has developed, more powerful immunosuppression can turn into more aggressive tumor progression. The association between malignancy and immunosuppressive therapy is mediated through numerous pathogenic factors. Indirectly, immunosuppressive drugs greatly increase the post-transplant risk of malignancy by impairing cancer surveillance and facilitating the action of oncogenic viruses. However, the direct pro- and anti-oncogenic actions of antirejection drugs also play an important role. Therefore, the continual introduction of new immunosuppressive drugs and the growing knowledge about their different oncogenic profiles require a continuous evaluation of the available evidence on this topic.
In the last decades, liver transplantation has become even more and widely indicated as a curative treatment for selected patients with hepatocellular carcinoma. However, with recent therapeutic advances as well as efforts to increase the donor pool, liver transplantation has been carefully expanded to patients with other primary or secondary malignancies in the liver. Cholangiocarcinoma, colorectal and neuroendocrine liver metastases, and hepatic epithelioid haemangioendothelioma are amongst the most relevant new indications. This topic could be discussed with a special attention to the newest indications for liver transplantation and future perspectives within the recently established concept of transplant oncology.
Moreover, translational research is accelerating the early identification of these conditions, the selection of biomarkers of progression, and the new therapeutic targets. In particular, with the prospect of “precision medicine” for tumors and the development of next-generation sequencing technology, more attention has been paid to the application of high-throughput sequencing technology in clinical oncology research, which is mainly applied to the early diagnosis of tumors and analysis of tumor-related genes. Additionally, the development of organoid models over the past decade has been one of the major breakthroughs in the field of stem cells. Organoid models of diseases that are highly simulated, such as malignancies, are expected to continue to make new advances in precision medicine and regenerative medicine.
Finally, immune checkpoint inhibitors (ICIs) have become a possible treatment for transplant recipients, even if these treatments are challenging due to the possibility of disrupting immune tolerance. However, increasing data suggest that immunotherapy for cancer in transplant patients may be a feasible option for selected patients; however, clinical experiences/data and prospective trials in specific organ transplant recipients are needed.
Therefore, the aims of this Special Issue will be to analyze and revise all the main aspects of this important topic that involves a large number of clinicians and researchers worldwide in order to provide new clinical evidence, guidelines, and translational/basic research findings on this important topic.
We warmly welcome submissions from both solicited and spontaneous submissions.
Important
As a Gold open access journal, all submissions are subject to publishing fees. Fee solutions are available on a case-by-case basis, including discounts for ESOT members, Institutional Agreements, and authors from low- and middle-income countries. Please contact the editorial office if you have any questions: ti@frontierspartnerships.org.
Please see the following pages for:
Publishing Fees
Author Guidelines
Keywords: solid organ transplantation, cancer, donor-transfer, post-transplant cancer
Department of Pharmacy, Health and Nutritional Sciences, University of Calabria
Arcavacata di Rende, Italy
Innsbruck Medical University
Innsbruck, Austria
University Hospital of Padua
Padua, Italy
University of Edinburgh
Edinburgh, United Kingdom
University of Oslo
Oslo, Norway
Hospital Clinic of Barcelona
Barcelona, Spain
Innsbruck Medical University
Innsbruck, Austria
Share on WeChat
Scan with WeChat to share this article
